BLS/ALS Patient Care Report Form - wildsafe.org
1 hours ago Advised patient to seek care with an Emergency Department or physician as soon as possible. Advised the patient to call 911 if their condition changes or they change their mind regarding care/transport. Patient: I, , understand that people maintain the right to refuse medical care, treatment and/or the advice to be transported via local ... >> Go To The Portal
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What is a SOAP note in Aha?
A well-completed SOAP note is a useful reference point within a patient’s health record. Like BIRP notes, the SOAP format itself is a useful checklist for clinicians while documenting a patient’s therapeutic progress. [2]
Why is it important to have a soap in a hospital?
It is essential as proof that the patient is being treated regularly and effectively by different people. SOAP is actually an acronym and it stands for: S ubjective – This basically refers to everything the patient has to say about the issue, concern, problem and intervention procedures.
What is soap progress in occupational therapy?
In Occupational Therapy, a SOAP Progress Note might include the patient’s injuries and their severity, home exercises, and their effectiveness. Based on observations and interaction with their client, an OT professional might adjust their treatment program accordingly.
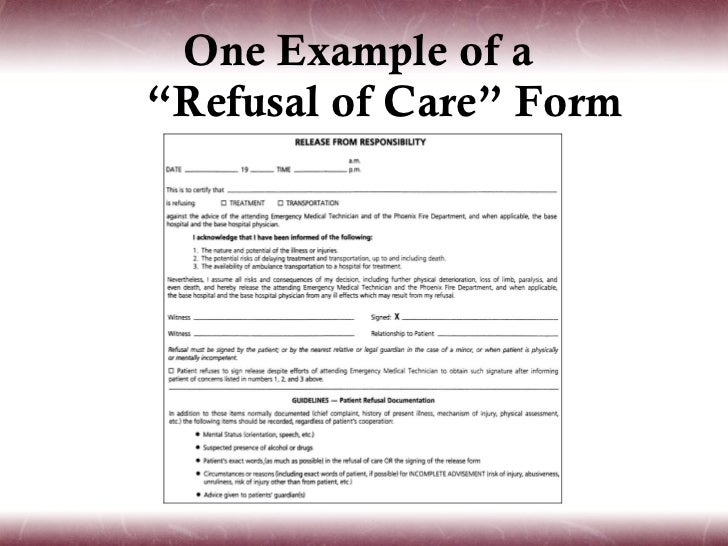
How do you document patient refusal of treatment?
DOCUMENTING INFORMED REFUSALdescribe the intervention offered;identify the reasons the intervention was offered;identify the potential benefits and risks of the intervention;note that the patient has been told of the risks — including possible jeopardy to life or health — in not accepting the intervention;More items...
What are 3 elements of getting and documenting a refusal of care?
This can be accomplished by using the CASE CLOSED acronym for bulletproof documentation of a refusal. C = Condition, Capacity, and Competence—The documentation should include the patient's chief complaint(s) in the patient's own words.
When a patient is refusing medical treatment which information should be included in the documentation?
When a patient or the patient's legal representative refuses medically indicated treatment, documentation should reflect that the physician discussed the nature of the patient's condition, the proposed treatment, the expected benefits and outcome of the treatment and the risks of nontreatment.
Should the medical assistant document that the patient refused the medication?
But to avoid legal and ethical ramifications, you must document such refusals properly. If your patient refuses treatment or medication, your first responsibility is to make sure that he's been informed about the possible consequences of his decision in terms he can understand.
What is included in informed refusal?
Refusing care Along with the right of informed consent comes the right of informed refusal. People who have legal and clinical capacity may refuse any medical care. They may refuse care even if it is something almost everyone else would accept or something that is clearly life-saving.
What would you do if a client refused to give their informed consent?
When a patient refuses to sign an informed consent form. Competent patients have the right to not consent, or to refuse treatment. If one of your patients refuses to sign a consent form, do not proceed without further attempting to obtain the consent.
What is the process when a resident refuses medication?
Possible action that can be taken Patient refuses medication • Try to identify why the resident has refused the medication, their beliefs, understanding of what the medicine is for and consequences of not taking the medication. Establish if there is a pattern of refusal. Address any issues identified.
Who should you inform when a service user refuses to take prescribed medication?
If, for some reason, the person you care for is unwilling to take their medicines, talk to their GP or pharmacist. They may be able to suggest a form of the medicine that's more acceptable than tablets.
What are the two exceptions to informed consent?
Several exceptions to the requirement for informed consent include (1) the patient is incapacitated, (2) life-threatening emergencies with inadequate time to obtain consent, and (3) voluntary waived consent.
Do patients have the right to refuse medication?
Every competent adult has the right to refuse unwanted medical treatment. This is part of the right of every individual to choose what will be done to their own body, and it applies even when refusing treatment means that the person may die.
Can a patient refuse a prescription?
Residents have the legal right to refuse medications, and long-term care facilities need to employ a process to resolve disagreement between the health care team that recommends the medication and the resident who refuses it.
Can nurses refuse to give medications?
When there is a realistic, reasonable, and individualized evaluation by a nurse that to administer a medication to a specific patient could result in injury to or death of the patient, then the nurse must withhold the medication, promptly notify the physician or other healthcare provider who ordered the medication, ...
How do you document patient refusal in EMS?
Refuses to sign refusal However, you will need to insert in the refusal form that the person refused to sign and what you did to secure the person's signature on the form. Whether or not the refusal form is signed by the patient or the patient's representative, it also should be signed by you and dated.
Does a patient have the right to refuse treatment?
To the extent permitted by law, participation shall include the right to refuse treatment." Under federal law, the Patient Self-Determination Act (PSDA) guarantees the right to refuse life sustaining treatment at the end of life.
How do you document a medical error?
Disclosing medical errors the right wayBegin by stating there has been an error;Describe the course of events, using nontechnical language;State the nature of the mistake, consequences, and corrective action;Express personal regret and apologize;Elicit questions or concerns and address them; and.More items...
What should you remember when you are documenting?
Medical Documenting: 5 Important Things to RememberWrite Clearly and Legibly. According to a report in Medscape, the modern health care system puts increasing demands on nurses' time. ... Handle Records with Care. ... Document All Your Actions. ... Record Only Objective Facts. ... Capture Orders Correctly.
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
What is a soap note?
An effective SOAP note is a useful reference point in a patient’s health record, helping improve patient satisfaction and quality of care.
What is a soap progress note?
SOAP is an acronym for the 4 sections, or headings, that each progress note contains: Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
What is the purpose of a detailed assessment?
A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and. Plan: Where future actions are outlined.
Is soap a subjective or unbiased?
Unbiased: In the Subjective section, particularly, there is little need for practitioners to use weighty statements, overly positive, negative, or otherwise judgmental language. SOAP notes are frequently used both as legal documents and in insurance claims.
Why are soap notes still used?
SOAP notes have been around for some time now and because of their efficiency and functionality, they are still being used now. The very first SOAP note template was created and developed by a brilliant doctor named Lawrence Weed way back in the 1960s. It was done at the University of Vermont as an element of the POMR (Problem-Oriented Medical Record). During those times, objective documentation did not exist so physicians had the tendency to make decisions about treating patients without scientific basis.
What is a soap note?
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data. Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors. Using these kinds of notes allows the main health care provider ...
What is a soap note template?
A SOAP note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. A SOAP note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
1. Facts surrounding the dispatch undocumented
Many times when an ambulance responds to a 911 call, that simple fact is missing from the ePCR. And in way too many chart reviews or audits, we find no dispatch determinants or other clear indication of the patient’s reported condition at the time of dispatch.
3. Vague explanation of specific interventions and procedures performed
Too many times we find nothing more than "per protocol" to explain why a cardiac monitor was applied, an IV was initiated or some other procedure was performed. Just like the ambulance service must be medically necessary to be reimbursed by Medicare and other payers, the treatments provided must also be medically necessary.
4. No explanation for EMS-specific care and treatment
This is important with regard to two areas. First, is clearly explaining the transport itself and the service or care the patient required during the transport that could not be provided other than by trained medical professionals in an ambulance.
5. Inadequate description of patient complaints or findings
The most common example of an inadequately described or quantified complaint or finding is with regard to a patient's pain.
About the author
For over 20 years, PWW has been the nation’s leading EMS industry law firm. PWW attorneys and consultants have decades of hands-on experience providing EMS, managing ambulance services and advising public, private and non-profit clients across the U.S.
What was the Medic 1 response to above location?
(Location): Medic 1 responded to above location on a report of a 62 y.o. male c/o of chest pain. Upon arrival, pt presented sitting in a chair attended by first responder. Pt appeared pale and having difficulty breathing.
Is PT allergic to shellfish?
PT has a sensitivity to Morphine Sulfate and is allergic to shellfish. PT has been complaint with his medication, according to his wife. PTs last meal was a chicken breast and rice. Upon our arrival PT was found sitting on the couch, in a high state of anxiety due to his flooded basement.
Does the patient respond to questions?
Patient does not respond to questions, but crew is informed by family that patient is deaf. Per family, the patient has been "sick" today and after consulting with the patient's doctor, they wish the patient to be transported to HospitalA for treatment.
Popular Posts:
- 1. osu my patient portal faq.com
- 2. elite medicine patient portal tupelo, ms
- 3. university of toledo patient portal login
- 4. valley medical patient portal florence ma
- 5. patient portal | brazosport regional
- 6. main portal vein patient
- 7. moffitt tampa patient portal
- 8. delta dental patient michigan login
- 9. marianne santioni rheumatology patient portal
- 10. timpanogos hospital patient portal