5+ SAMPLE Patient Incident Report in PDF
7 hours ago What Is the Purpose of the Patient Incident Report? 1. Management of Risks. Having the knowledge that an incident has happened can motivate administrators to address the... 2. Control of the Product’s Quality. Medical facilities strive to … >> Go To The Portal
A patient incident report, according to Berxi, is “an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.” Reports are typically completed by nurses or other licensed personnel.
- Patient name and hospital number/date of birth.
- Date and time of incident.
- Location of incident.
- Brief, factual description of incident.
- Name and contact details of any witnesses.
- Harm caused, if any.
- Action taken at the time.
How to write an incident report?
Writing Incident Reports-Tips and Examples How to write a helpful and professional incident report Be specific, detailed, factual, and objective. Language: This information can be used by many institutional and external partners so make sure to use language that you wouldn’t mind President Phipps reading.
How to write a good accident or incident report?
- The type of incident that took place
- Where the incident happened
- The date, day and time of the incident
- Names of the people involved
- Injuries that were obtained
- Medical treatment that may have been required
- Equipment that was involved
- Events leading up to the incident that could have contributed to it taking place
Why to write an incident report?
- When someone has passed away.
- When someone lost a limb or part of a limb.
- When someone is likely to pass away due to the events of the incident.
What is an example of an incident report?
If there is an injury, illness or damage as a result of the hazard, that is an incident and should be reported as such. For example… If no one changes a burned out lightbulb leading to dimly lit conditions in an area, that is a hazard.
How do you write a patient incident report?
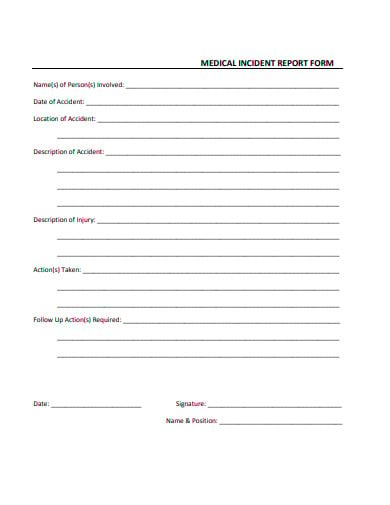
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
How do you write a simple incident report?
What Does an Incident Report Need to Include?Type of incident (injury, near miss, property damage, or theft)Address.Date of incident.Time of incident.Name of affected individual.A narrative description of the incident, including the sequence of events and results of the incident.Injuries, if any.More items...•
What should be included in an incident report for healthcare?
Just the factsPatient name, date of birth, and hospital ID number.Names of any other affected individuals (e.g., staff or visitors)Date, time, and location of the incident.Name and address of the facility where the event occurred.Type of incident (e.g., medication error, fall, equipment failure)More items...
How do you write an incident report in nursing example?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
What is an example of an incident?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
How do I write a report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What are the five elements of good incident report?
The key tasks to mention in the workflow includes notification of the incident, identification of responsible, interviews, investigation and analysis, conclusion, sharing learnings and implementation.
What is an example of an incident in healthcare?
Another example of an incident in healthcare could be caused by something as simple as not following established clinical protocols. For example, if a physician doesn't properly wash their hands before suturing a wound, the wound could become infected.
What is an example of a patient safety event?
A patient safety incident occurs but does not result in patient harm – for example a blood transfusion being given to the wrong patient but the patient was unharmed because the blood was compatible. or expected treatment – for example he/she did not receive his/her medications as ordered.
What are incident reports in nursing?
An incident report in nursing is a report which details an event where a person is injured, or property is damaged. If these conditions occur on medical facility property, completion of an incident report is necessary.
What is included in an incident report nursing?
Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected. Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient's physician.
How do you write a hospital report?
HOW TO WRITE A MEDICAL REPORTKnow that a common type of medical report is written using SOAP method. ... Assess the patient after observing her problems and symptoms. ... Write the Plan part of the Medical report. ... Note any problems when you write the medical report.More items...
How Effective Are Incident-Reporting Systems for Improving Patient Safety?
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a...
When to Report an Incident to the Police?
The general rule of thumb is that an incident report should be completed as quickly as possible after an occurrence happens. Minor injuries should...
How Are Patient Safety Event Reporting Systems used?
Hospitals are replete with patient safety event reporting systems, which serve as a cornerstone of efforts to detect patient safety incidents and q...
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
How many hospital incidents go unreported?
According to a study by the US Department of Health and Human Services, 86 per cent of hospital incidents go unreported. Even more staggering, though, is the reason behind this. Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements.
How to organize an incident report?
How a report is organized depends on the complexity of the incident and the type of report being written. Usually, writing in chronological order is the simplest way to organize a report. However, an inspection incident report may be written by enumerating details according to findings. 5. A Good Incident Report Must Be Clear.
What is the best way to write an incident report?
It is also best to write in an active voice, which is more powerful and interesting than the passive voice. 2. A Good Incident Report Must Be Factual and Objective.
What is incident report?
1. An Incident Report Must Be Accurate and Specific. When you write an incident report, you must be specific and accurate about the details, not merely descriptive. For example, instead of writing "the old patient", it is more accurate to describe him as "the 76-year old male patient".
What abbreviations should be used in an incident report?
A Good Incident Report Must Only Include Proper Abbreviations. The use of abbreviations may be appropriate in certain cases, such as the use of Dr. Brown and Mr. Green, instead of writing Doctor or Mister.
Do you have to include your opinion in a report?
If you must include an opinion in your report, it is best to state it with the similar description that appears on some incident report samples: "In my opinion, there were too many people in the overloaded bus. In fact, there were 80 persons inside, when a bus of this size is only allowed to carry 70 individuals."
Do you need an incident report in court?
Your incident report may be needed in court someday and you should be prepared to be questioned based on your report. So the more details you have on your report, the less you have to depend on your memory and the more credible you are.
What is incident report?
An incident report is a formal recording of the facts related to a workplace accident, injury, or near miss. Its primary purpose is to uncover the circumstances and conditions that led to the event in order to prevent future incidents. Every incident report you file should contain a minimum of the following:
Why do you need to create an incident report?
Create an incident report as soon as your employees are safe, which includes seeking medical attention and implementing an immediate corrective action to prevent further danger or damage. By recording details immediately, you improve the accuracy of your report and the effects of your corrective actions.
Why is incident reporting important?
Their importance means you want to get as much relevant information as you can as quickly as possible.
How long does it take to complete an OSHA 301?
If the incident resulted in a recordable injury, you must complete OSHA Form 301 within seven days.
What to do after documenting an incident?
After documenting the incident, you may have legal reporting requirements. Report and store the files according to recordkeeping requirements from regulatory bodies. It’s generally best practice to preserve the files for the duration of employment.
What are the two common mistakes you should avoid when reporting an accident?
But sometimes, safety teams can get in their own way and miss out on important details by making common mistakes. Blame-casting and just getting it done are two common incident reporting mistakes you should avoid. It is easy to go on a witch hunt when accidents happen.
What happens if you rush through a report?
In addition, if you rush through the report to “just get it done,” you may miss out on important details or lack clarity in wording. Irresponsible reporting can lead your team into even more danger, while detailed, clear reporting can lead to improved work conditions and better training.
What is clinical incident?
A clinical incident is an unpleasant and unplanned event that causes or can cause physical harm to a patient. These incidents are harmful in nature; they can severely harm a person or damage the property. For example—
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
What Is a Nursing Incident Report?
A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side.
What Are the Information Needed in a Nursing Incident Report?
An incident report should be completed every time that an accident or any mishaps in giving care to the patient or any instances or possibilities of deviating from the normal operation and routine of the facility and/or from the patient.
What Is the Desired Outcome of Writing a Nursing Incident Report?
In writing an incident report a positive outcome should always be manifested but that depends on the event of the accident. There are times that the outcomes are deviated from what we expect and manifest. For pessimistic situations that will not happen in the future, a good, desired outcome must be manifested in writing a nursing incident report.
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Incidents happen from time to time. We cannot deny the fact that accidents of different kinds may occur or happen unexpectedly. Such cases may happen inside a hospital facility. It can happen in the operating room, wards, nurses’ station, laboratories, and even emergency rooms.
Purpose of a Nursing Incident Report
Nursing incident reports are used to initiate communication in sequencing events about the important safety information to the hospital administrators and keep them updated on aspects of patient care. Writing an incident report has its own purpose that will provide us a clearer understanding of how it works and how it is done.
How to Write a Nursing Incident Report
This is to confirm that an accident or incident has occurred that requires an incident report. Clinical reasoning and judgment must be possessed by a clinical health practitioner or any healthcare professional. It is a skill that is needed to be learned in a span of time.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes that need to be made in the facility or to facility processes to prevent recurrence of the incident and promote overall safety and quality of care.
What is hospital incident report?
Hospital Incident Reports are just a few of the types of reports done to record details of accidents or incidents inside the workplace. Hospitals, nursing homes and healthcare workers are usually the types that fill out this incident report.
When to use an outline?
Outlines are used when you are planning on how to address the situation. If you are thinking about making a step by step report, I highly recommend using an outline. It would be easier to break down the incident into specific sub plots and look for ways to avoid the problem or to improve on it.
What is an official statement?
An official statement that is being written down to state the occurrence and how it happened. A well written document that can also be considered an official document where a person, usually the one who filed for the report, states what had happened during the event.
Can hospital incidents be avoided?
Hospital incidents are a common thing to happen. It cannot be avoided but it can be recorded to make sure occurrences like that would not happen again.
Can anything happen at any moment?
Anything can happen at any moment. Being prepared may sometimes feel like a risk to take when you planned out everything in order to avoid any incidents that may come. Unfortunately, you cannot stop what may have already been set in motion. However, you can report it so that people would know how to avoid it or at least, ...
Can you write a letter to report an incident?
You are using that tool to file for the report. So check out some of the common ones listed below. Letter – Yes, you can write a letter to report an incident. This is still considered a tool or a way to write your incident report. It follows the same rule and format as any other letter.
What is incident report?
An incident report is a document that accurately provides the details of an incident; especially one that causes damages, injury or death. It helps an organization to accurately profile the different events leading to such an incident and the aftermath (s) of this occurrence.
Who files a safety incident report?
A safety incident report is usually filed by the security personnel in charge of the premises where the security breach took place. It can also be filed in cases of computer system breaches, unauthorized access to an organization's database and compromised user accounts.
What are some examples of workplace incident reports?
Examples of workplace incident report include: A report about sexual harassment or assault in the workplace.
Why is a security incident report important?
This report is important because it helps an organization to keep track of security breaches and safety measures.
What is the objective of an incident report?
Objectivity: An incident report must be written in an objective manner that is devoid of any emotions; regardless of the nature of the incident. The reporter must take extra care to avoid sentiments that can get in the way of an objective presentation of the details of the incident.
How soon after an incident should you write a letter?
Write your Letter as Soon as Possible: Typically, an incident report letter should be sent in, at most, 48 hours after the incident. Writing your letter immediately after the incident would help you to provide vivid and accurate descriptions of the events surrounding the incident.
Why is an accident report called an incident report?
It is also referred to as an accident report because it typically outlines information relating to an accident or injury. However, an incident report can also contain information about near misses or other unusual or hazardous happenings in different contexts.
What is an incident report?
A workplace incident report is a document that states all the information about any accidents, injuries, near misses, property damage or health and safety issues that happen in the workplace.
Why is a safety incident report important?
A safety incident report helps ensure nobody is subject to mistreatment because it contains information from the injured employee as well as eyewitnesses. This helps fill in missing pieces of information and figure out how the accident occurred exactly.
What is a general staff accident report?
It includes all the necessities to describe a workplace incident to ensure it is recorded correctly. This general form is ideal for any business type.
Why should an accident report be signed?
The accident report should be signed to acknowledge that it is everything that the employee remembers happening. This workplace incident report template includes the basic guidelines and best practices of what to include to make sure the report includes all the details it should.
What form do you fill out to keep a log of an OSHA incident?
If this is an OSHA recordable incident (accident) and the company is exempt from OSHA recordkeeping, the employer must also fill in OSHA Form 300 . This form enables both the employer and the agency to keep a log of the injuries or illnesses that happen in the workplace.
How long does it take to complete an accident report?
Typically, a workplace accident report should be completed within 48 hours of the incident taking place. The layout of an accident incident report should be told like a story, in chronological order, with as many facts as the witnesses can possibly remember.
What is an eyewitness in a chemical incident?
Eyewitnesses that can tell their side of the story. For example…If a chemical was involved in the incident, it should be noted if the victim was wearing appropriate PPE or not, as well as a photograph of the damage and the chemical’s label stating its components.
