SBAR Tool: Situation-Background-Assessment …
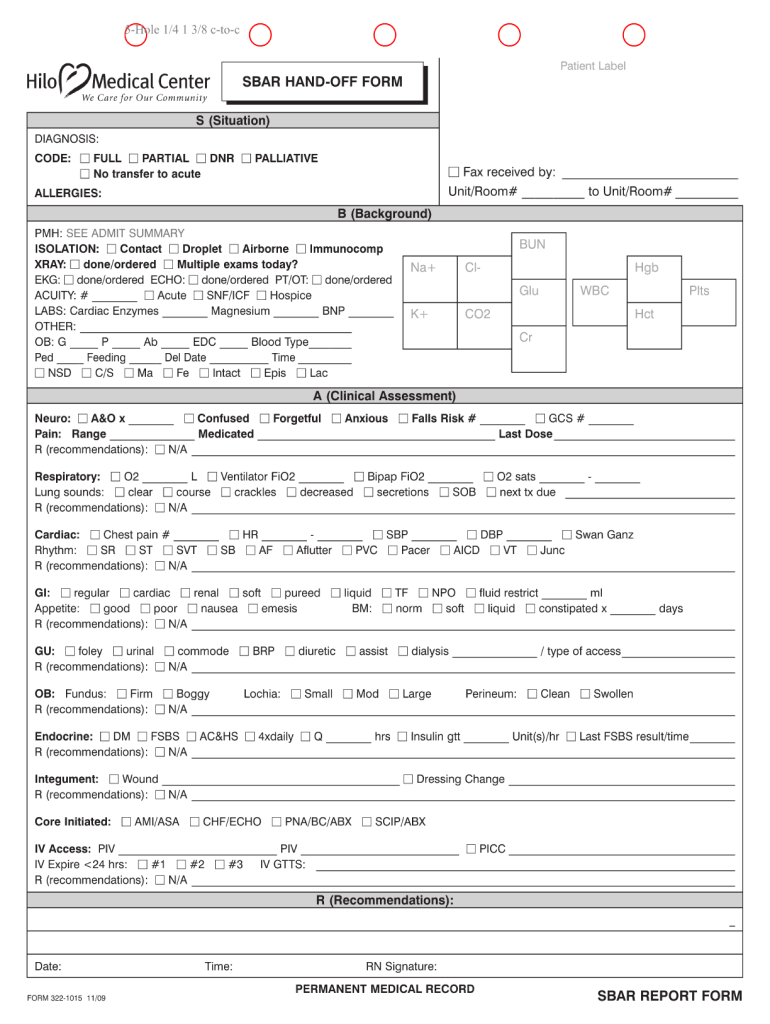
6 hours ago The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition. S = Situation (a concise statement of the problem) B = Background (pertinent and brief information related to the situation) >> Go To The Portal
You can use the SBAR nursing document to communicate any non-urgent and urgent patient information to other healthcare professionals like therapists and doctors. SBAR examples are typically used for: Conversations with physical therapists, physicians, and other medical professionals.
Full Answer
How can I use the SBAR nursing document?
You can use the SBAR nursing document to communicate any non-urgent and urgent patient information to other healthcare professionals like therapists and doctors. SBAR examples are typically used for:
What is SBAR in healthcare?
The SBAR concept was first developed by the USA Navy as a means of communicating information to nuclear submarines. Because of its success, the SBAR template got introduced to the health care system in the 1990s. The SBAR technique offers a framework of communication between the members of a healthcare team regarding the condition of a patient.
Can SBAR replace an executive summary in a report?
In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information. SBAR was introduced by the United States military in the 1940s and later targeted specifically for nuclear submarines where concise and relevant information was essential for safety.
What are the disadvantages of the SBAR technique for bedside reporting?
This is because some nurses feel too intimidated to give recommendations to physicians. One disadvantage of using the SBAR technique for bedside reporting is when you have to wake the patients up or their families when you start the discussion.
What is SBAR documentation?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
How do you write an SBAR report?
The components of SBAR are as follows, according to the Joint Commission:Situation: Clearly and briefly describe the current situation.Background: Provide clear, relevant background information on the patient.Assessment: State your professional conclusion, based on the situation and background.More items...
What is SBAR in nursing example?
In nursing, the situation, background, assessment and recommendation (SBAR) technique is a tool that allows health professionals to communicate clear elements of a patient's condition.
What is an SBAR and how is it used?
SBAR is an easy-to-use method for improving accuracy in medical communication. It works best for nurse/physician interaction, either verbally or in written form. It's a standardized communication method endorsed by the Joint Commission to increase patient safety.
What is the essence of SBAR documentation to nursing health assessment and nursing care?
[7] The main purpose of SBAR technique is to improve the effectiveness of communication through standardization of communication process. Published evidence shows that SBAR provides effective and efficient communication, thereby promoting better patient outcomes.
Why is SBAR used in nursing?
The nurses found SBAR to “help organize their thinking and streamline data.” This made the transition of care smoother and ultimately resulted in better patient care.
What does SBAR mean in healthcare?
situation, background, assessment and recommendationCommunicating with SBAR. The SBAR (situation, background, assessment and recommendation) tool is provided below to aid in facilitating and strengthening communication between nurses and prescribers throughout the implementation of this quality improvement initiative.
What is recommendation in SBAR?
SBAR: Situation-Background- Assessment-Recommendation. The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition.
What does the SBAR approach to patient safety encourage?
The SBAR approach to patient safety encourages: Consistency in assessment and practices. As a manager in a new nursing home, where might you consult for guidance and evidence to support the development of safe patient practices?
How do I give my SBAR to a doctor?
2:5012:26Nurse-to-Physician Communication Report NCLEX - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo the first thing what you want to do is you want to get a layout of an s bar a lot of units willMoreSo the first thing what you want to do is you want to get a layout of an s bar a lot of units will have these created for you and you just fill them in.
What does SBAR mean in healthcare?
situation, background, assessment and recommendationCommunicating with SBAR. The SBAR (situation, background, assessment and recommendation) tool is provided below to aid in facilitating and strengthening communication between nurses and prescribers throughout the implementation of this quality improvement initiative.
What is SBAR handoff?
Situation, Background, Assessment, Recommendation (SBAR) is a mnemonic used to structure information sharing to avoid communication failures during handoffs.
How does SBAR improve communication?
Widely used to standardize patient handoff practice, SBAR was first developed by the U.S. Navy to improve communication of critical information. Applied to the clinical setting, it can be used to organize information into a logical, easily recalled pattern, which expedites the handoff process and reduces error.
What is the SBAR technique in nursing?
In nursing, the situation, background, assessment and recommendation (SBAR) technique is a tool that allows health professionals to communicate clear elements of a patient's condition.
Benefits of SBAR technique in nursing
The SBAR technique is beneficial because it gives nurses a framework to communicate important details of precarious scenarios quickly and efficiently. It ensures other healthcare team members receive all the relevant information in an organized and timely manner with specific instructions on how to respond.
When to use SBAR in nursing
You can use the SBAR technique in a variety of care scenarios and settings. It can begin care, such as when you admit a patient to a unit. The technique can help you relay patient information when transferring care over to a new care team. It can also be effective in times of crisis, such as alerting a physician to an alarming development.
Tips for using SBAR in nursing
Here are some tips you can use to communicate effectively using the SBAR technique:
Examples of SBAR in nursing
If you're ready to get started using the SBAR technique, here are some examples of the communication strategy in practice for your reference:
What is SBAR in nursing?
With an acronym that’s easy to remember, SBAR nursing is a concrete tool that can be very useful in framing conversations that require immediate attention or action, especially if they are about patients with critical status.
What is a SBAR?
What is the SBAR? The SBAR concept was first developed by the USA Navy as a means of communicating information to nuclear submarines. Because of its success, the SBAR template got introduced to the health care system in the 1990s. The SBAR technique offers a framework of communication between the members of a healthcare team regarding ...
How do you write a good SBAR?
The use of an SBAR communication template provides you with an easy-to-remember concrete mechanism that proves useful for the framing of any conversation, especially the critical ones that require the immediate attention or action of a clinician.
What to include?
You can use the SBAR nursing document to communicate any non-urgent and urgent patient information to other healthcare professionals like therapists and doctors. SBAR examples are typically used for:
Why is the R in SBAR the weakest point?
Usually, the “R” in SBAR is the weakest point of nurses. This is because some nurses feel too intimidated to give recommendations to physicians. One disadvantage of using the SBAR technique for bedside reporting is when you have to wake the patients up or their families when you start the discussion.
How to prevent negative outcomes for patients while strengthening teamwork in healthcare?
An excellent way to prevent negative outcomes for patients while strengthening teamwork in healthcare is by improving the communication between caregivers. In this aspect, SBAR examples can provide common expectations like what needs communication, how to structure communication, and what the required elements are.
Why use a SBAR template?
One such technique is the use of an SBAR tool template as this provides a framework for effective communication. As a result, it can help you create an environment that allows people to express their concerns by speaking up. Such actions can reduce the risks of adverse events and foster a safer culture in the hospital.
What is SBAR in a report?
Quality Glossary Definition: SBAR. SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
Why is SBAR used in a report?
In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information. SBAR was introduced by the United States military in the 1940s and later targeted specifically for nuclear submarines where concise and relevant information was essential for safety.
Why is SBAR important?
Because of its simplicity and usefulness in crucial situations, SBAR has many implementations in healthcare. It can be used between professional staff such as nurses and physicians, and it also has value for hand-offs by nurses between change of shifts or patient transfers. Below is a basic example of how SBAR communication can be used in a healthcare setting, but SBAR can be used as a leadership communication tool in any industry.
What is the purpose of SBAR?
SBAR can be written or provided verbally, but the purpose is to provide essential, concise information, usually during crucial situations.
What is background section?
The background section present s essential information related to the situation. This information should pertain only to the current situation.
Why is handoff report nerve wracking?
It is nerve-wracking because you don’t want to miss important information, but you don’t want to give too much or too little information. Providing the right amount of information pertinent to each healthcare provider is what makes a handoff report great. While I was in school, I thought it was a little silly to repeat the information ...
What to say in the beginning of a drip?
In the beginning, say the situation, any drips, and the plan for the patient. And if you anticipate that you’ll need help from her, this is the time to speak up.
Is SBAR good for nurses?
SBAR is comprehensive and is great for the oncoming nurse. Here are the elements.
What is a SBAR in nursing?
What is SBAR? It’s a communication method used to promote and simplify communicating important patient information to other members of the healthcare team. The SBAR method strategically helps communicate a specific patient situation along with the patient’s background, your assessment, and possible recommendations.
What is background information?
Background (focused information that the listener needs to know in order to understand the current patient problem)
How to say hello to a patient?
Say hello and the listener’s name along with your name and the unit you’re on, patient’s name, room number, the patient’s current situation (why you’re calling and this should be a short sentence).
What is SSESbar in nursing?
SSESBAR takes the common SBAR ( S ituation, B ackground, A ssessment, R equest/ R ecommendation) communication tool , focuses it on the situation, problem or condition being faced , and expands it to include data collection, suggested SBAR content & notification urgency, and management options. SSESBAR is based on decades-old work, enhanced with diagnostic and management options available today. Designed for long-term (LTC) and post-acute (PA) care in nursing homes and skilled nursing facilities (SNF), Situation-Specific SBARs can also be used in other healthcare settings such as home care, hospitals and assisted living facilities (ALF), when appropriate. SSESBAR can also be used as examples of scenarios for education or as a template.
What is SSESbar?
SSESBAR can also be used as examples of scenarios for education or as a template. SSESBAR begins with Situations. Find the Situation in the list that best fits the problem or condition, exploring the "Also consider:" options.

Popular Posts:
- 1. auburn miller clinic patient portal
- 2. community hospital patient portal missoula mt
- 3. st vincents patient portal
- 4. nextmd patient portal enroll
- 5. manatee patient portal
- 6. patient portal um
- 7. patient portal sentara medical center
- 8. carthage family wellness patient portal
- 9. north atlanta obgyn patient portal
- 10. dilworth dermatology patient portal