3+ SAMPLE Patient Medical Report in PDF
17 hours ago Step 3: Report the specimens. Whatever test and examination that you have given to the patient, have the result documented. These will be the laboratory results and test results to have an analysis of what disease could have touched the patient. There should be a clear notation how you have derived the specimens. >> Go To The Portal
What does a patient care report consist of?
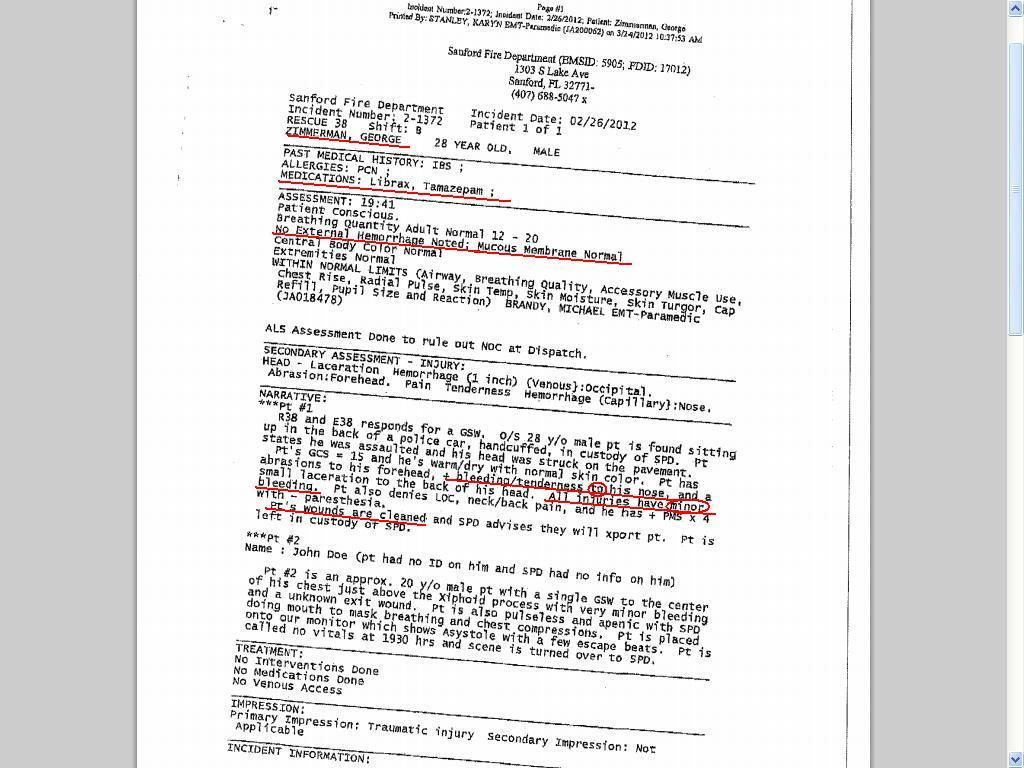
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care. What should not be written in a patient care report?
Who has the access to the patient medical report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must.
What is the difference between patient medical records and patient medical reports?
Patient medical records are simple data about the patient while a patient medical report is more elaborate and comprehensive. Though the importance of medical records and the purpose of medical records are almost the same with a patient medical report, the patient medical report is more beneficial.
Why do hospitals keep patient medical report?
They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report. It can be a proof if there is any doctor withholding treatments.
How do you write a patient care report for a narrative?
How to Write an Effective ePCR NarrativeBe concise but detailed. Be descriptive in explaining exactly what happened and include the decision-making process that led to the action. ... Present the facts in clear, objective language. ... Eliminate incorrect grammar and other avoidable mistakes. ... Be consistent and thorough.
What is a component of the narrative section of a patient care report?
The narrative section of the PCR needs to include the following information: Time of events. Assessment findings. emergency medical care provided. changes in the patient after treatment.
How do you write a proper PCR?
The following five easy tips can help you write a better PCR:Be specific. ... Paint a picture of the call. ... Do not fall into checkbox laziness. ... Complete the PCR as soon as possible after a call. ... Proofread, proofread, proofread.
What is SAMPLE in patient assessment?
SAMPLE, a mnemonic or memory device, is used to gather essential patient history information to diagnose the patient's complaint and make treatment decisions.
What is the purpose of the narrative section of the patient care report?
Detailed explanation of medical necessity: Your narrative should be detailed and provide a clear explanation for why the patient needed to be transported by ambulance. Include what the medical reasons were that prevented the patient from being transported by any other means.
What is a PCR document?
The PCR documentation is considered a medical document that becomes part of the patient's permanent medical record. It is also considered a legal document in cases where liability and/or malpractice issues arise. It is the source in which all medical billing claims are based.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
How do you write a patient narrative EMT?
0:4011:38How to Write a Narrative in EMS || DCHART Made Easy ... - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo while in route dispatch advises that the patient can be found outside the residence. Then i talkMoreSo while in route dispatch advises that the patient can be found outside the residence. Then i talk about what i see whenever i get onto the scene upon arrival ems is directed toward the curb.
What is an objective patient assessment finding?
Examples of objective assessment include observing a client's gait , physically feeling a lump on client's leg, listening to a client's heart, tapping on the body to elicit sounds, as well as collecting or reviewing laboratory and diagnostic tests such as blood tests, urine tests, X-ray etc.
What are the five steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
What is initial assessment of patient?
6.1. 3 Initial Assessment for In Patient to be carried out by RMO, Treating Doctor or his / her Team Member (as appropriate) within one hour of admission to determine immediate care needs and to decide on plan of care.
What is primary assessment?
A primary assessment is the first examination and evaluation of a patient by a medical person such as a trained emergency medical technician or other first responder to an emergency situation, and is focused on stabilizing the patient.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
Definition of Narrative
A narrative is a story. The act of telling a story in the form of a narrative. An oral or written document that describes a series of events in the form of a story. The process of writing or speaking about what happened by explaining using a narrative.
Definition of Assessment
An assessment is an examination. A written examination to evaluate a person. The process of evaluating an individual through their knowledge, skills, and value. To examine a person before giving the final verdict. To judge someone by means of giving them an examination.
Definition of Narrative Assessment
A narrative assessment is a type of evaluation that describes an individual’s learning and wellness. It allows the assessor to know just how far the student has progressed. In addition to that, it also helps understand the key points and the points where the individual needs to improve on.
Importance of a Narrative Assessment
The importance of writing a narrative assessment is to assess the important moments. To write down all the achievements and the milestones of your students. To highlight their strengths and to improve on their weaknesses.
Tips for Writing a Narrative Assessment
Regardless if you are a student in college who is told to write a narrative assessment, or a teacher who wants to write a narrative assessment for their student, you can surely admit that writing one can sometimes be difficult. Especially when you have no idea where to begin and how to begin.
Are narrative assessments useful?
Yes, narrative assessments are very useful when you want to write down the results of the assessments given to students or patients.
Is there a minimum word count when writing a narrative assessment?
There is no minimum word count but the maximum word count should be around 1,000 words. This contains the introduction to your narrative assessment, followed by the examination, the result and evaluation. Lastly, the concluding statement.

Popular Posts:
- 1. premier clarksville tn patient portal
- 2. for a patient prescribed amitriptyline (elavil) and should instruct the patient to report:
- 3. patient portal internal medicine group lawrence ks
- 4. wcg patient portal
- 5. dr georgalus patient portal
- 6. shirazi patient portal
- 7. my lifetime health patient portal
- 8. are we required to report to the cdc if a patient has syphilis
- 9. my genesis patient portal tricare
- 10. wordpress medical patient portal