FREE 14+ Patient Report Forms in PDF | MS Word
36 hours ago Check out our 4 patient report sheet selection for the very best in unique or custom, handmade pieces from our templates shops. >> Go To The Portal
What are the parts of a patient report form?
The Parts of Patient Report Forms In completing the patient report forms, below are the following important or essential information that should be provided. Otherwise, results from medical assessments cannot be given due to deficiency of relevant information. The patient’s personal information The patient’s full name The date of birth The gender
What information should be included in a hospital report?
The patient’s social security number The medical assessmentinformation The patient’s attending physician or doctor The date and time when the patient was admitted or hospitalized The type of injuries or health problem conditions The patient’s medical diagnosis The symptoms of current condition The level of consciousness The vital signs and details
What are the benefits of patient report forms?
Therefore, one thing that could help are the patient report forms. These are used to summarize the overall findings from the diagnosis of a patient assessment, thus, making it easier to display and explain the results briefly yet comprehensively. Generic Patient Report Form
What do you put on a report sheet?
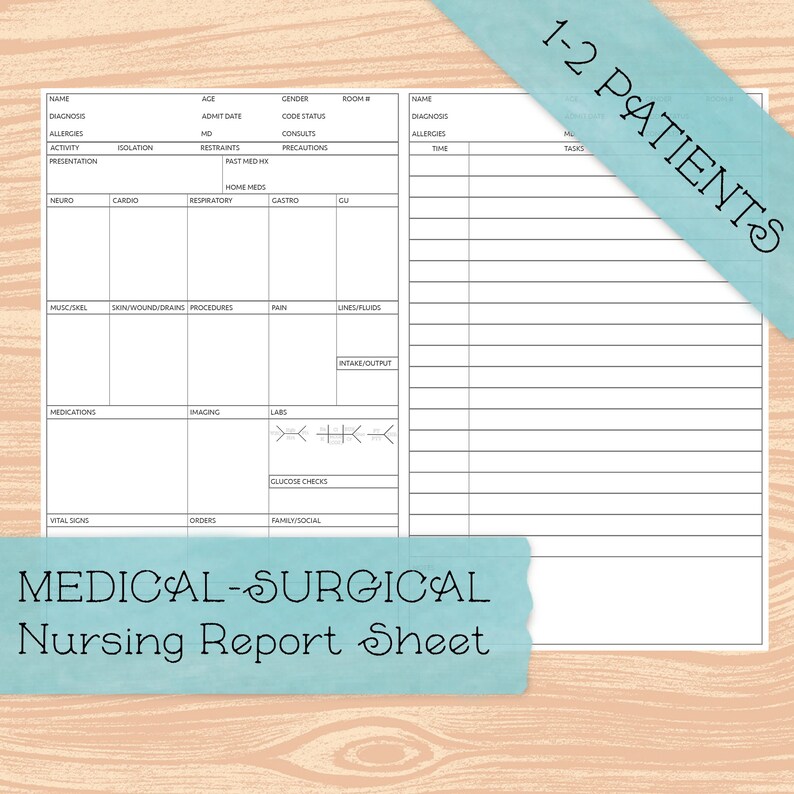
A report sheet like this does a great job of giving the charge nurse a few boxes to check . . . of just the important stuff (vent, isolation, foley). Every now and then I will post a pic of a typical IV pole for an ICU patient.
How do I write a nursing report sheet?
0:0020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is atMoreSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is at the top right and type nursing report templates or nursing report sheets.
What is a report sheet in nursing?
A Nurse's Brain, also known as a nursing report sheet, is a term for a sheet of paper that nurses use to capture important patient information and stay organized. It contains sections for key areas like patient history, diagnoses, labs, medications, body systems status, and more.
What should a nursing report include?
Written by nurses who are wrapping up their shifts and provided to those nurses beginning the next shift, these details should include a patient's current medical status, along with his or her medical history, individual medication needs, allergies, a record of the patient's pain levels and a pain management plan, as ...
How do I fill out report sheet?
0:025:46FILLED IN REPORT SHEET - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd then I have their admitting diagnosis. When they are admitted in history and accidentallyMoreAnd then I have their admitting diagnosis. When they are admitted in history and accidentally flipped these around. So this was the admitting diagnosis. Across them or admitting.
How do you write a patient report?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
How do you make a report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What is SBAR template?
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
How do I write a good bedside report?
5 Tips for an Effective End-of-Shift ReportGive a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
Why do nurses need a report sheet?
A nursing report sheet enables these nurses to keep a track of the tasks that they have to perform. This allows them to go through their activities, in an untroubled manner and without missing out on any of the tasks.
Why are nursing report sheets important?
These report sheets are highly beneficial in helping the medical staff to obtain information efficiently.
What is an ICU nursing report?
ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
What is patient monitoring?
Patient Monitoring: Vital Signs – The Patient Monitoring section contains the vital signs that have been recorded at some particular time during their stay at the healthcare center. A few of the most important characteristics which are present in all the nursing reports are the Time Check, Blood Pressure details, Heart Rate, Temperature, Oxygen Saturation Levels, Oxygen, Respiratory Rates, Pain (if any, that has been inflicting the patient), Blood Sugar Details, Details of Dispensed Medications and Medicine Administration Timing.
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
Why is it important to create a nursing report?
A1. A nursing report is created to facilitate the job of transferring information. Therefore, it is highly essential that the nursing report is created in a manner that successfully fulfills its objective. Given below are a few tips which all nurses keep in mind to create a near-perfect nursing report:
How many nursing brainsheets are there?
But seriously . . . I’ve only shown you small portions of 20 of the 33 nursing brainsheets included in our massive database.
How many patients do you have in an ICU?
When you work ICU a lot of times you only have two patients . . .sometimes even just one.
Do nurses have to take reports?
Yep. Even charge nurses have to take report.

Popular Posts:
- 1. ou family medicine tulsa patient portal
- 2. patient portal michael smith
- 3. dentrix patient login
- 4. skylands medical patient portal
- 5. vital heart and vein patient portal login humble tx
- 6. patient portal una
- 7. tampa bay hearing and balance center patient portal
- 8. how to view lab results through altamed patient portal
- 9. annual statistical report of patient waiting time in nigeria
- 10. advanced dermatology specialties cape coral fl patient login