Reporting Patient Incidents: A Best Practices Guide | i-Sight
26 hours ago · Types of patient incidents that may occur include: Patient complaints (e.g. problems with care or care provider) Unexpected events related to treatment (e.g. adverse reaction to medication, equipment malfunction) Bodily harm (e.g. injury to patient, staff, contractor or visitor) Patient-related ... >> Go To The Portal
What Is the Purpose of the Patient Incident Report?
- Management of Risks. Having the knowledge that an incident has happened can motivate administrators to address the...
- Control of the Product’s Quality. Medical facilities strive to deliver the highest level of care and customer service...
- Training. New employees can be better prepared for real-life events that...
Full Answer
What is a patient incident?
As defined by Berxi, a patient incident report is “a detailed, written description of the chain of events leading up to and following an unforeseen scenario in a healthcare context,” which can be either computerized or paper-based. Nurses or other qualified professionals are often responsible for completing reports.
What is a hospital incident report?
The man has not been identified. Medical staff at the hospital told investigators that the man's injuries were not consistent with a traffic accident. The incident report indicates that the man was injured by a gunshot. However, the official cause of death ...
How to write a good accident or incident report?
- The type of incident that took place
- Where the incident happened
- The date, day and time of the incident
- Names of the people involved
- Injuries that were obtained
- Medical treatment that may have been required
- Equipment that was involved
- Events leading up to the incident that could have contributed to it taking place
How do I get an incident report?
Please bring the following to your appointment:
- Appointment confirmation code from Eventbrite.
- Completed Request Forms DPS-96-C
- Payment in the amount of $16.00 per incident requested. Check or Money Order payable to “Treasurer-State of CT”.
- Cash payments must be the exact dollar amount. Change cannot be provided.

How do you write an incident report on a patient?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What is the process of reporting an incident?
The seven critical steps of incident investigation are:Take immediate action. ... Report the incident. ... Report to the authorities. ... Investigate and develop corrective actions. ... Calculate the costs. ... Conduct a root cause analysis. ... Record the details.
What is the incident reporting process in healthcare?
Incident reporting in healthcare refers to collecting healthcare incident data with the goal to improve patient safety and care quality. Done well, it identifies safety hazards and guides the development of interventions to mitigate risks, thereby reducing harm.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What are the 5 steps the person reporting an incident accident or near miss must do?
5. Process (following incident occurrence)5.1 Minimise the risk of injury or damage. ... 5.2 Seek support for any injuries. ... 5.3 Notifiable incidents. ... 5.4 Report the incident. ... 5.5 Incident response. ... 5.6 Review and monitor.
What are the five elements of good incident report?
The key tasks to mention in the workflow includes notification of the incident, identification of responsible, interviews, investigation and analysis, conclusion, sharing learnings and implementation.
What is the nurse's responsibility regarding incident reporting?
Nurses have a duty to report any error, behaviour, conduct or system issue affecting patient safety. This accountability is found in section 6.5 of the Code of Conduct. Medications and devices prescribed to patients can cause unforeseen and serious complications.
How do you write an incident report in nursing?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
Why do nurses report incidents?
Nurses must comply with any formal internal reporting procedure, typically a written incident report. The next step is internal investigation or tracking, depending on the nature and seriousness of the event. It is helpful for an organization to know what worked well during the incident as well as what did not.
What are the 3 types of incidents?
3 Types of Incidents You Must Be Prepared to Deal WithMajor Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What are examples of incidents?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
What incidents should be reported?
What must be reported?Deaths and injuries caused by workplace accidents.Occupational diseases.Carcinogens mutagens and biological agents.Specified injuries to workers.Dangerous occurrences.Gas incidents.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
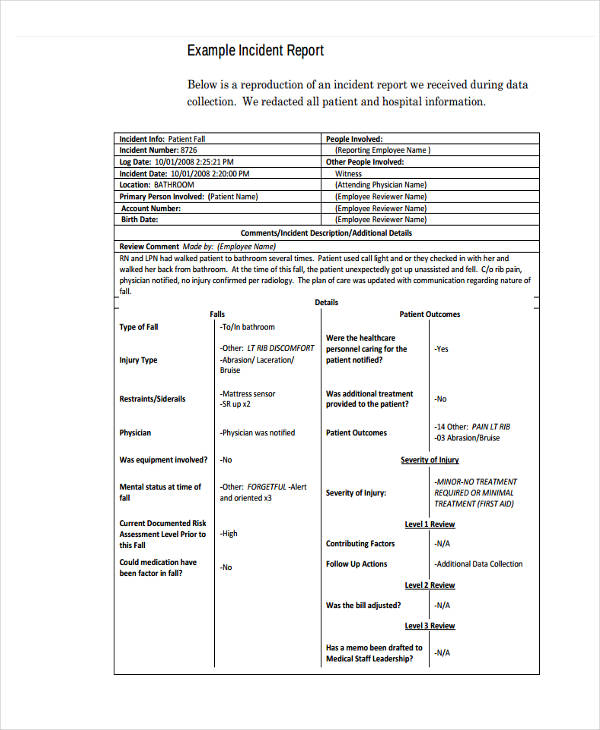
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
What is AHRQ common format?
AHRQ has also developed Common Formats —standardized definitions and reporting formats for patient safety events— in order to facilitate aggregation of patient safety information. Since their initial release in 2009, the Common Formats have been updated and expanded to cover a broad range of safety events.
What is the Patient Safety and Quality Improvement Act?
The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to work with a PSO and specify the scope and volume of patient safety information to share with a PSO. Because health care providers can set limits on the ability of PSOs to use and share their information, this system does not follow the pattern of traditional voluntary reporting systems. However, health care providers and PSOs may aggregate patient safety event information on a voluntary basis, and AHRQ will establish a network of patient safety databases that can receive and aggregate nonidentifiable data that are submitted voluntarily. AHRQ has also developed Common Formats —standardized definitions and reporting formats for patient safety events—in order to facilitate aggregation of patient safety information. Since their initial release in 2009, the Common Formats have been updated and expanded to cover a broad range of safety events.
How is event reporting used in health care?
A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require further, more detailed investigation. While event reporting utilization can be a marker of a positive safety culture within an organization, organizations should resist the temptation to encourage event reporting without a concrete plan for following up on reported events. A PSNet perspective described a framework for incorporating voluntary event reports into a cohesive plan for improving safety. The framework emphasizes analysis of the events and documenting process improvements arising from event analysis, rather than encouraging event reporting for its own sake.
What is patient safety event reporting?
Patient safety event reporting systems are ubiquito us in hospitals and are a mainstay of efforts to detect patient safety events and quality problems. Incident reporting is frequently used as a general term for all voluntary patient safety event reporting systems, which rely on those involved in events to provide detailed information. Initial reports often come from the frontline personnel directly involved in an event or the actions leading up to it (e.g., the nurse, pharmacist, or physician caring for a patient when a medication error occurred), rather than management or patient safety professionals. Voluntary event reporting is therefore a passive form of surveillance for near misses or unsafe conditions, in contrast to more active methods of surveillance such as direct observation of providers or chart review using trigger tools. The Patient Safety Primer Detection of Safety Hazards provides a detailed discussion of other methods of identifying errors and latent safety problems.
What is PSNet perspective?
A PSNet perspective described a framework for incorporating voluntary event reports into a cohesive plan for improving safety. The framework emphasizes analysis of the events and documenting process improvements arising from event analysis, rather than encouraging event reporting for its own sake.
Why are event reports limited?
The spectrum of reported events is limited, in part due to the fact that physicians generally do not utilize voluntary event reporting systems.
What is structured mechanism?
A structured mechanism must be in place for reviewing reports and developing action plans. While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic medical records.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
How long does it take to file an incident report?
Usually, nurses or other hospital staff file the report within 24 to 48 hours after the incident occurred. The outcomes improve by recording incidents while the memories of the event are still fresh.
How to write an incident report?
In determining what to include in an incident report and which details can be omitted, concentrate on the facts.#N#Describe what you saw when you arrived on the scene or what you heard that led you to believe an incident had taken place. Put secondhand information in quotation marks, whether it comes from a colleague, visitor, or patient, and clearly identify the source.# N#Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected .#N#Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient’s physician. Include any statement a patient makes that may help to clarify his state of mind, as well as his own contributory negligence.#N#It’s equally important to know what does not belong in an incident report.#N#Opinions, finger-pointing, and conjecture are not helpful additions to an incident report.#N#Do not:
When is an incident report required?
When a situation is significant—resulting in an injury to a person or damage to property —it’s obvious that an incident report is required. But many times, seemingly minor incidents go undocumented, exposing facilities and staff to risk. Let’s discuss three hypothetical situations.
Why is incident reporting important?
An incident report invariably makes its way to risk managers and other administrators, who review it rapidly and act quickly to change any policy or procedure that appears to be a key contributing factor to the incident. The report may also alert administration that a hospital representative should talk to a patient or family to offer assistance, an explanation, or other appropriate support. That’s an important function because such communication can be the balm that soothes the initial anger—and prevents a lawsuit.
Why is it important to file incident reports?
Filing incident reports that are factually accurate is the only way to help mitigate potentially disastrous situations arising from malpractice and other lawsuits. It’s your responsibility to record unexpected events that affect patients, colleagues, or your facility, regardless of your opinion of their importance.
What is the duty of a nurse?
As a nurse, you have a duty to report any incident about which you have firsthand knowledge. Failure to do so could lead to termination. It could also expose you to liability, especially in cases of patient injury. Protect yourself and your patients by filing incident reports anytime unexpected events occur.
What happens when incident reports are filled out properly?
If the incident report has been filled out properly with just the facts, there should be no reason to be concerned about how it’s used. The danger comes only when incident reports contain secondhand information, conjecture, accusations, or proposed preventive measures that do not belong in these reports.
Why is it important to talk to a hospital representative?
That’s an important function because such communication can be the balm that soothes the initial anger —and prevents a lawsuit.
What is incident report?
1. An Incident Report Must Be Accurate and Specific. When you write an incident report, you must be specific and accurate about the details, not merely descriptive. For example, instead of writing "the old patient", it is more accurate to describe him as "the 76-year old male patient".
What is the best way to write an incident report?
It is also best to write in an active voice, which is more powerful and interesting than the passive voice. 2. A Good Incident Report Must Be Factual and Objective.
How to organize an incident report?
How a report is organized depends on the complexity of the incident and the type of report being written. Usually, writing in chronological order is the simplest way to organize a report. However, an inspection incident report may be written by enumerating details according to findings. 5. A Good Incident Report Must Be Clear.
What abbreviations should be used in an incident report?
A Good Incident Report Must Only Include Proper Abbreviations. The use of abbreviations may be appropriate in certain cases, such as the use of Dr. Brown and Mr. Green, instead of writing Doctor or Mister.
Why is it important to know what happened in the workplace?
This is important, especially when considering the liabilities of the workers involved and how similar incidents can be avoided . It is, therefore, critical ...
Do you need an incident report in court?
Your incident report may be needed in court someday and you should be prepared to be questioned based on your report. So the more details you have on your report, the less you have to depend on your memory and the more credible you are.
Do you have to include your opinion in a report?
If you must include an opinion in your report, it is best to state it with the similar description that appears on some incident report samples: "In my opinion, there were too many people in the overloaded bus. In fact, there were 80 persons inside, when a bus of this size is only allowed to carry 70 individuals."
Background
Characteristics of Incident Reporting Systems
- An effective event reporting system should have four key attributes: While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic medical records. Specialized systems have also been developed for specific settings, such as th…
Limitations of Event Reporting
- The limitations of voluntary event reporting systems have been well documented. Event reports are subject to selection bias due to their voluntary nature. Compared with medical record review and direct observation, event reports capture only a fraction of events and may not reliably identify serious events. The spectrum of reported events is limited, in part due to the fact that ph…
Using Event Reports to Improve Safety
- A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require furth…
Current Context
- At the national level, regulations implementing the Patient Safety and Quality Improvement Act became effective on January 19, 2009. The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to wo…
Popular Posts:
- 1. dr.dorociak patient login
- 2. if the patient has adverse reaction to medication report to
- 3. ems patient care report documentation
- 4. healow patient portal terrible reviews
- 5. patient portal beaufort
- 6. north houston family medicine patient portal
- 7. pain management of tulsa patient portal
- 8. dr mark nelson patient portal
- 9. ascension patient portal, st. vincent carmel
- 10. site:www.tassajarasystems.com patient portal