Submit a Tip to DEA
3 hours ago Report Suspected Unlawful Sales of Pharmaceutical Drugs on the Internet. RX Abuse Online Reporting. Report illegal sales/distribution of prescription drugs (i.e., oxycodone, hydrocodone, etc.); doctors and pharmacies. Synthetic Drug Online Reporting. Report an incident with Synthetic Drugs (i.e., Green Giant, Joker, N … >> Go To The Portal
Full Answer
Can a doctor report you for drug abuse?
You may worry that telling a doctor about illegal drug use will get you in trouble with the law, or your family. While admitting drug use to your doctor is not an easy thing to do, it’s crucial, to be honest with your care provider. Vices such as alcohol or drug abuse can cause or complicate symptoms.
How do you report a drug activity?
Method 1 Method 1 of 3: Making a Report
- Collect the necessary information. If you suspect that there is illegal drug activity occurring in your area, you will want to make a report with the proper authorities.
- Contact local resources. Your first step should be to contact the police department nearest you. ...
- Find national agencies. ...
- Stay anonymous. ...
How to report drug activity anonymously?
Young was charged with the following charges:
- Resisting an Officer
- Two counts of Battery of a Police Officer
- Two counts of Possession of a Controlled Dangerous Substance with Intent to Distribute
- Two counts of Possession of a Controlled Dangerous Substance
- Possession of Drug Paraphernalia
- Five counts of Possession of a Firearm while in Control of a Controlled Dangerous Substance
How to recognize prescription drug abuse?
What Are the Prescription Drug Abuse Symptoms?
- Opioids. Pain medication addiction or opioid addiction are some of the most common pill addictions. ...
- Stimulants. Stimulants are used to treat attention deficit hyperactivity disorder (ADHD) and some sleep disorders.
- Anti-Anxiety Medications, Hypnotics, and Sedatives. ...
- Common Drug Abuser Behaviors. ...
What to do if patient is on drugs?
Advise: Provide medical advice about the patient's drug use. Recommend quitting before problems (or more problems) develop. Give specific medical reasons. Refer patients with suspected co-occurring conditions (e.g., depression, pain) to a relevant specialist.
What are the priority nursing interventions for substance abuse?
Nursing interventions for a client with substance abuse include:Providing health teaching for client and family. Clients and family members need facts about the substance, its effects, and recovery.Addressing family issues. ... Promoting coping skills.
Is drug use protected under Hipaa?
The information shared is protected. If you tell your doctor that you have been using drugs or drinking alcohol in risky ways (e.g., while driving, or illegally) the doctor cannot have you arrested or send you to jail. HIPAA protects you from the provider sharing (disclosing) your information to non-treatment entities.
What does CFR 42 stand for?
42 CFR Part 2 (“Part 2”) is a federal regulation that requires substance abuse disorder treatment providers to observe privacy and confidentiality restrictions with respect to patient records.
What is the most effective intervention for substance abuse?
CBT is often rated as the most effective approach to treatment with a drug and alcohol population.
What is nada in nursing?
NANDA International (formerly the North American Nursing Diagnosis Association) is a professional organization of nurses interested in standardized nursing terminology, that was officially founded in 1982 and develops, researches, disseminates and refines the nomenclature, criteria, and taxonomy of nursing diagnoses.
What is a patient required to do in order for a request to restrict the use or disclosure of their PHI to their health plan to be granted?
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item ...
Which of the following could be a reason why a client is denied access to their health information?
General concerns about psychological or emotional harm are not sufficient to deny an individual access (e.g., concerns that the individual will not be able to understand the information or may be upset by it). In addition, the requested access must be reasonably likely to cause harm or endanger physical life or safety.
What are the penalties for violating 42 CFR part 2?
New Penalties for Violations of Part 2 Under the CARES Act, Congress gave HHS the authority to issue civil money penalties for violations of Part 2 in accordance with the civil money penalty provisions established for HIPAA violations, ranging from $100 to $50,000 per violation depending on the level of culpability.
What is a QSOA?
Qualified Service Organization Agreements (QSOAs): Part 2 requires the QSO to agree in writing that in receiving, storing, processing, or otherwise dealing with any information from the program about patients, it is fully bound by Part 2, it will resist, in judicial proceedings if necessary, any efforts to obtain ...
What are Part 2 Records?
Part 2 was introduced to encourage people suffering from drug and alcohol addiction issues to seek treatment without fear of retribution; therefore, these records are to be held in the highest confidence allowing the patient to act as the gatekeeper in the movement of these records.
What information does 42 CFR Part 2 Protect?
The 42 CFR Part 2 regulations (Part 2) serve to protect patient records created by federally assisted programs for the treatment of substance use disorders (SUD).
How to report someone who is abusing prescription drugs?
One of the ways you can report someone who is abusing prescription drugs is by contacting the DEA. The DEA has a tip hotline where you can let them know if someone is abusing prescription drugs. It can be tough to call the DEA on a loved one or friend. However, if they are abusing prescription drugs, such as hydrocodone or oxycodone, ...
How many people abuse prescription drugs?
According to HealthDay, in the United States of America, around seven million people abuse prescription drugs. This is a much higher statistic than it is for those who abuse heroin, ecstasy, and cocaine combined. Many people think about addiction and don’t want to relate to it. They don’t think it will ever happen to someone they love.
Can a doctor run a drug test?
Most doctors, nowadays, run random drug tests. This allows them to test the levels of drugs in their patient’s system, to make sure they aren’t abusing them. This isn’t done all the time, though. If you want to report someone who is abusing prescription drugs, you can make a call to the prescribing doctor.
Can a doctor tell you about a patient?
The truth is the doctor can’t tell you anything about their patients, even if it is your loved one, unless you are on the contact list. However, that doesn’t mean you can’t talk to the doctor and just have them listen to you. Most doctors, nowadays, run random drug tests.
Can prescription painkillers be addictive?
There are some prescription drugs that are more addictive than others, such as prescription painkillers and ADHD medications. While these medications should always be taken only by the person they are prescribed to and at the dosage prescribed, that doesn’t always happen.
What is the abuse in the exam room?
Patients in your exam room may be experiencing one of a number of forms of abuse—domestic violence, human trafficking or other violence— and identifying those being abused can sometimes be tough.
What to consider before reporting suspected violence?
What to consider before reporting. Before reporting suspected violence or abuse, the Code says physicians should: Inform patients about requirements to report. Obtain the patient’s informed consent when reporting is not required by law.
How many victims of trafficking had contact with a health professional?
The authors noted research showing that 88% of victims had contact with a health professional while being trafficked, but none were identified or offered help in getting out of their situation during the medical encounter.
Do you have to see one on one for a trafficked patient?
Dr. Ravi said it is also important to establish a policy—even putting it in writing in the exam and waiting rooms—that says a patient needs to be seen one-on-one for part of the visit. Trafficked patients may come in with a man or woman who is trafficking them; sometimes that person could even be a relative.
Can a physician make exceptions to patient privacy?
Exceptions can be made if a physician reasonably believes that a patient’s refusal to authorize reporting is coerced and therefore does not constitute a valid informed treatment decision. Physicians should also protect patient privacy when reporting by disclosing only the minimum necessary information.
What is crime stoppers?
Crime Stoppers is an effective national program that collects anonymous crime tips. Anyone who wants to report drug activity can contact Crime Stoppers via phone or online. A national tip line is available 24/7, and the program also operates out of local offices.
How many arrests have been made by Crime Stoppers?
As of March 2019, Crime Stoppers’ efforts have resulted in over 746,000 arrests, clearing out over one million legal cases.1.
What is David's new neighbor selling drugs?
David’s new neighbor, Jeff, is selling drugs and he’s worried about what it will do to the neighborhood. David fears for the safety of not only his kids but all the children on the block. He wants to do something—he wants to put a stop to the drug activity before it gets any worse.
What is the number to dial to ensure anonymity?
To further ensure anonymity, callers can dial *67 before calling any agency or organization. This blocks the number of the caller. Reporting activity to the local police is also an option, but anonymity may be harder to keep.
Can a witness make a phone call?
Witnesses to drug crimes can make an anonymous phone call or fill out an online form. What’s more, you can rest easy knowing that all Crime Stoppers workers are trained to protect the caller’s identity and, instead of caller ID, all incoming phone calls are assigned a numerical code.
Is David and Lisa alone?
One thing’s for sure: David and Lisa are not alone. Concerns about personal safety and legal prosecution scare many people away, ultimately leading to them opting to keep drug crimes quiet.
What to do if you know you have a substance use problem?
If you know you have a substance use problem, it’s time to talk to your doctor, even if the drug (s) you’re using are illegal. The point of talking to your doctor is to seek and obtain the kind of treatment that will help you stop abusing drugs and end your addiction. Your doctor can help you find the right treatment.
What is the biggest fear people face when just thinking about admitting substance use to their doctor?
The biggest fear people face when just thinking about admitting substance use to their doctor is consequences. Discomfort grows when a person is using an illegal substance. The biggest fear is being reported to the authorities. Thanks to doctor-patient confidentiality, this fear is often only as big as you make it.
Can drug use affect insurance?
Those records can then be submitted to your insurance agency, and they can then use those records to increase premiums, deny payment, or deny coverage for certain conditions and/or procedures. It is possible that admitting to drug use could affect future coverage when most needed.
Do doctors report injuries?
Harm Must be Reported: By law and ethics, a doctor must report severe bodily injury. For example, if a doctor were to fail to report a bullet or gunshot wound, a powder burn, or other injury resulting from the discharge of a gun or firearm, they risk a Class A misdemeanor.
Can a doctor discuss drug use?
A doctor cannot discuss the information you share in confidence, and if they do, you can take legal recourse, even when admitting something like heroin or cocaine use. If you choose to talk to your doctor about illegal substance use, you can, in most cases, rest assured that your conversation will remain confidential.
What is the responsibility of a pharmacist?
You have a professional responsibility to prescribe and dispense controlled substances appropriately, guarding against abuse while ensuring that patients have medication available when they need it. You have a personal responsibility to protect your practice from becoming an easy target for drug diversion.
Why do health care workers lose their lives?
Tragically, some health care workers have even lost their lives to their drug addiction because the people who saw the signs and symptoms of their drug use refused to get involved.
What is a treatment program?
Treatment programs range from self-help to formal recovery programs. A number of state licensing boards, employee assistance programs, state diversion programs and peer assistance organizations will refer individuals and their families to appropriate counseling and treatment services.
What are ordinary tasks?
Ordinary tasks require greater effort and consume more time; Interpersonal relations with colleagues, staff and patients suffer. Rarely admits errors or accepts blame for errors or oversights; Heavy "wastage" of drugs; Sloppy recordkeeping, suspect ledger entries and drug shortages;
What is the meaning of "unreliability" in the workplace?
Unreliability in keeping appointments and meeting deadlines; Work performance which alternates between periods of high and low productivity and may suffer from mistakes made due to inattention, poor judgment and bad decisions; Confusion, memory loss, and difficulty concentrating or recalling details and instructions.
Can losing a job affect a drug abuser?
The threat of losing a job may have more influence on a drug abuser than a spouse' s threat to leave or a friend's decision to end a relationship. Many drug abusers will seek help for their problem if they believe their job is at stake, even though they have ignored such pleas from other people important in their life.
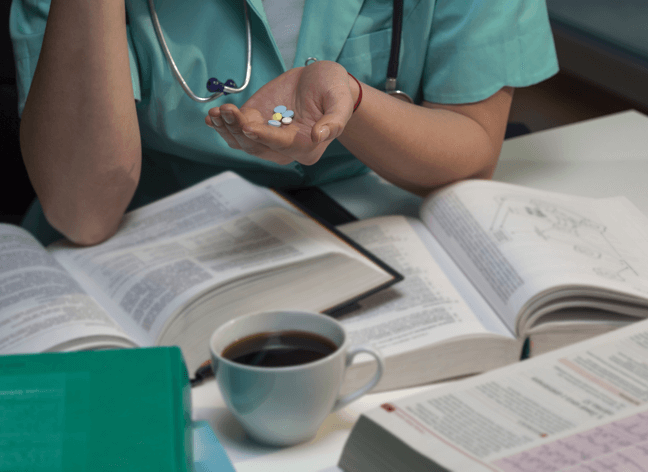
Is drug abuse a health problem?
Drug Addiction in Health Care Professionals. The abuse of prescription drugs—especially controlled substances—is a serious social and health problem in the United States today. People addicted to prescription medication come from all walks of life. However, the last people we would suspect of drug addiction are health care professionals—those ...
What is the mandate of a nurse?
As mandated, they are trained to identify signs and symptoms of abuse or neglect and are required by law to report their findings. Failure to do so may result in discipline by the board of nursing, discipline by their employer, and possible legal action taken against them. If a nurse suspects abuse or neglect, they should first report it ...
What should a nurse do when treating a patient?
Nurses should provide a calm, comforting environment and approach the patient with care and concern. A complete head-to-toe examination should take place, looking for physical signs of abuse. A chaperone or witness should be present if possible as well.
Where is Amanda Bucceri?
Amanda Bucceri Androus is a Registered Nurse from Sacramento, California. She graduated from California State University, Sacramento in 2000 with a bachelor's degree in nursing. She began her career working night shifts on a pediatric/ med-surg unit for six years, later transferring to a telemetry unit where she worked for four more years. She currently works as a charge nurse in a busy outpatient primary care department. In her spare time she likes to read, travel, write, and spend time with her husband and two children.
Do nurses have to be able to connect victims of abuse?
While not required by law, nurses should also offer to connect victims of abuse to counseling services. Many times, victims fall into a cycle of abuse which is difficult to escape.
Do nurses have a responsibility to care for victims of abuse?
Employers are typically clear with outlining requirements for their workers, but nurses have a responsibility to know what to do in case they care for a victim of abuse.
Should a nurse report abuse?
The nurse should notify law enforcement as soon as possible, while the victim is still in the care area. However, this depends on the victim and type of abuse. Adults who are alert and oriented and capable of their decision-making can choose not to report on their own and opt to leave. Depending on the state, nurses may be required ...
What information is required for a Part 2 notification?
To promote compliance, SAMHSA recommends that the notification include all the information that the Part 2 program is required to document in the patient’s records (e.g., date and time of disclosure, the nature of the emergency, etc.).
What is a Part 2 patient?
Part 2 permits the disclosure of information under certain circumstances without consent during a medical emergency or in other limited situations. If a Part 2 program (or a healthcare provider that has received Part 2 patient information) believes that there is an immediate threat to the health or safety of any individual, there are steps described below that the Part 2 program or healthcare provider can take in such a situation:
Can a patient revoke a multiparty consent?
Yes. Under 42 CFR Part 2 (hereafter referred to as “Part 2”), a patient can revoke consent to one or more parties named in a multi-party consent form while leaving the rest of the consent in effect. In a non-Health Information Exchange (HIE) environment, this can be accomplished simply by the Part 2 program indicating on the consent form or in the patient’s record that consent has been revoked with respect to one or more named parties. In an HIE environment, the revocation with respect to one or more parties should be clearly communicated to the Health Information Organization (HIO) as well as noted in the patient’s record by the Part 2 program.
Can a QSOA be used to redisclose lab results?
The QSOA authorizes communication only between the Part 2 program and QSO. The QSO, in this case the lab, would not be allowed to redisclose lab results about the Part 2 program’s patient to another QSO such as an HIO, even if the HIO has also signed a QSOA with the Part 2 program.
Is a controlled substance program federally assisted?
No. Not every primary care provider who prescribes controlled substances meets the definition of a “program” or part of a “program” under Part 2. For providers to be considered “programs” covered by the Part 2 regulations, they must be both ”federally-assisted” and meet the definition of a program under 42 CFR § 2.11.
Do restrictions on disclosure apply to child abuse?
Reports of child abuse and neglect: The restrictions on disclosure do not apply to the reporting under State law of incidents of suspected child abuse and neglect to the appropriate State or local authorities.
Does SAMHSA require oral revocation?
While oral revocations must be honored under Part 2, SAMHSA recommends the entity obtaining the revocation get it in writing and/or document the revocation in the patient’s record. Part 2 prohibits a program from making a disclosure on the basis of a consent which it knows has been revoked.

Contacting The Dea
- One of the ways you can report someone who is abusing prescription drugs is by contacting the DEA. The DEA has a tip hotlinewhere you can let them know if someone is abusing prescription drugs. It can be tough to call the DEA on a loved one or friend. However, if they are abusing prescription drugs, such as hydrocodone or oxycodone, their life is at stake. Your loved one or friend may even be buying prescription drugs off others or selling theirs. If this i…
Calling 9-1-1
- One of the most difficult things someone may have to face is dealing with a loved one’s addiction. Have you ever noticed that your loved one is abusing prescription drugs? Maybe they are even selling them or buying drugs from someone else. If so, you can call 9-1-1. You want your loved one to stay safe. Every time they abuse prescription drugs they are at a risk of overdosing. If they are selling or buying drugs from others, they are putting themselve…
Contacting The Prescribing Doctor
- One of the things many people don’t consider is calling their loved one’s doctor. They think the doctor won’t hear them out due to privacy laws. The truth is the doctor can’t tell you anything about their patients, even if it is your loved one, unless you are on the contact list. However, that doesn’t mean you can’t talk to the doctor and just have them listen to you. Most doctors, nowadays, run random drug tests. This allows them to test the levels of drugs i…
Contacting The Pharmacy
- Another thing you can do to report someone who is abusing prescription drugs is to contact the pharmacy where they are getting their medications. Depending on which pharmacist you speak with, they may refuse to fill the prescriptions any longer or they may make a note to that patient’s doctor as well. Pharmacies keep track of what prescriptions are...