How to Report Medical Billing Fraud: 8 Steps (with Pictures)
30 hours ago · Complaints about medical billing. Starting in 2022, insurance companies and plans, providers, and health care facilities must follow new rules that protect consumers from surprise medical bills. If you have a question about these rules or believe the rules aren’t being followed, contact the No Surprises Help Desk at 1-800-985-3059 from 8 am to 8 pm EST, 7 … >> Go To The Portal
If you suspect or witness a provider inappropriately billing or a member receiving inappropriate services, please call our anonymous and confidential WAF hotline at 1-866-685-8664. Louisiana Healthcare Connections and Centene take all reports of potential waste, abuse or fraud very seriously and investigate all reported issues.
- By Phone. Health & Human Services Office of the Inspector General. 1-800-HHS-TIPS. (1-800-447-8477) ...
- Online. Health & Human Services Office of the Inspector General Website.
- By Fax. Maximum of 10 pages. 1-800-223-8164.
- By Mail. Office of Inspector General. ATTN: OIG HOTLINE OPERATIONS. P.O. Box 23489.
What is medical billing abuse?
If a code is a bundled code and all components are billed separately, then this is considered fraud. Bill patients more than their co pays for services, which is referred to as “balance billing.” Medical billing abuse is going against accepted business practices. This can be unintentional and is why internal audits are so necessary.
How do I report fraudulent health care billing?
These Bureaus are typically run through the state Department of Insurance or Attorney General's office. Call to report fraudulent billing by a health-care provider under ACA. If you're registered for your health care under the Affordable Care Act, you can contact their billing department directly.
How do I report a medical billing error to the hospital?
Contact the hospital's billing department. In case the doctor or hospital made an honest mistake, it's best to bring the billing error to their attention as soon as you notice the problem. Look on the office's or hospital's website to find information regarding billing disputes.
How do I report questionable billing practices?
Find your local SMP. If the provider cannot resolve your billing concerns, report it. If you have Medicare, you can report questionable billing practices to Medicare. Report questionable billing practices to your insurance company’s antifraud department. You should find a number to report fraud on your insurance Explanation of Benefits (EOB).
What do you do if you suspect you are involved in inappropriate billing practices at your facility?
If you suspect or witness a provider inappropriately billing or a member receiving inappropriate services, please call OIG's Hotline at 1-800-HHS-TIPS (1-800-447-8477), directly to a Medi-Cal Fraud Control Unit (MFCU), or our anonymous and confidential FWA hotline at 1-866-685-8664. California Health & Wellness and ...
What is abuse in healthcare billing?
Abuse is defined as practices that are inconsistent with accepted sound fiscal, business, or medical practices, and result in an unnecessary cost or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care.
How do you fight medical billing errors?
How to Contest a Medical BillGet an Itemized Copy of Your Bill.Talk to Your Medical Provider.Talk to Your Insurance Company.Dispute a Medical Bill With the Collection Agency.Work With a Medical Advocate.Negotiate a Medical Bill With Your Medical Provider.Avoid Future Problems by Reviewing Your Insurance.
How do I report to CMS?
How to File a Complaint.CMS, on behalf of HHS, enforces HIPAA Administrative Simplification requirements.Go to ASETT.CMS.GOV.Upon logging in, click the "New Complaint" button on the welcome page.Click “Complaint Type” and select the issue you are reporting.More items...
Which of the following is an example of healthcare abuse?
Changing or forging an order or prescription, medical record, or referral form. Selling prescription drugs or supplies obtained under healthcare benefits. Providing false information when applying for benefits or services. Using Transportation Services to do something other than going for medical services.
What is defamation healthcare?
Examples of defamation per se, as applied to health care workers, are statements like falsely accusing someone of a crime.
What are the common medical billing errors?
5 Common Medical Billing ErrorsDuplicate Practice and Hospital Medical Billing. ... Incorrect Billing in Hospitals and Practices. ... Unbundling. ... Failure to Follow Hospital Billing Guidelines: Upcoding and Undercoding. ... Confusing a Denied Claim with a Rejected Claim.
What are some common billing errors?
The Most Common Billing & Coding Errors And How to Prevent ThemIncorrect Procedure Codes. ... Mishandled Overpayments. ... Lack of Data. ... Missing Or Incorrect Information. ... Invalid Codes. ... Upcoding. ... Healthcare Tech Errors. ... Get A Free Billing Process Audit!
Is medical bills on credit report Hipaa violation?
HIPAA does not regulate credit reporting of medical bills. The FCRA does. And the FCRA does not allow deletion of reported debt even in the case of a HIPAA violation. But the creditor may be willing to delete the reporting if you threaten to sue them for violating the law.
What is a CMS grievance?
A grievance is an expression of dissatisfaction (other than an organization determination) with any aspect of the operations, activities, or behavior of a Medicare health plan, or its providers, regardless of whether remedial action is requested.
What is the purpose of CMS reporting?
The purpose of Section 111 reporting is to enable CMS to pay appropriately for Medicare-covered items and services furnished to Medicare beneficiaries.
What does CMS stand for?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
What are the consequences of health care fraud?
The violations of health care fraud laws lead to serious consequences that comprise: 1 imprisonment and fines 2 civil fiscal penalties 3 loss of licensure 4 loss of staff privileges 5 elimination from involvement in federal health care programs
Can a doctor waive co-pays?
Although it may seem harmless to fulfill a waiver request the law is clear that physicians can only waive co-payments and/or deductibles in a limited situation. But routine waiver of co-payments and deductibles may be considered fraudulent in most government health care plans and insurance companies.
Can a provider bill for a treatment that is not approved?
Claiming for the treatments that were not performed. Medicaid and Medicare only reimburse for approve procedures. In this case, the provider cannot bill for tests and treatments which are not approved.#N#However, by manipulating the diagnosis, healthcare providers add procedures that were not essential and were provided only to increase reimbursements.#N#These are common unethical medical billing practices and is a serious violation of the healthcare act. It often goes unnoticed, since many patients don’t examine their EOBs and bills closely.#N#So, in such case call the doctor’s office for correction. If, they’re unwilling to correct it, then report them to your insurance company.
How to report Medicare fraud?
Where to report. If you have Medicare, you can report questionable billing practices to Medicare. Phone: 1-800-633-4117 (1-800-MEDICARE) TTY: 1-877-486-2049. Report questionable billing practices to your insurance company’s antifraud department. You should find a number to report fraud on your insurance Explanation of Benefits (EOB).
Where to report fraud on Medicaid?
If you are on Medicaid, you should report your concerns to the State Medical Assistance Office. Military personnel and veterans can report to Tricare. You may also want to contact your state insurance department.
Why do billing errors happen?
Because there are thousands of billing codes, mistakes can happen. These billing errors can be fixed if you call the mistake to the attention of the provider. By changing the codes, providers can get paid differing amounts of money. When providers use the correct codes for the procedures actually done, they get paid what they are due.
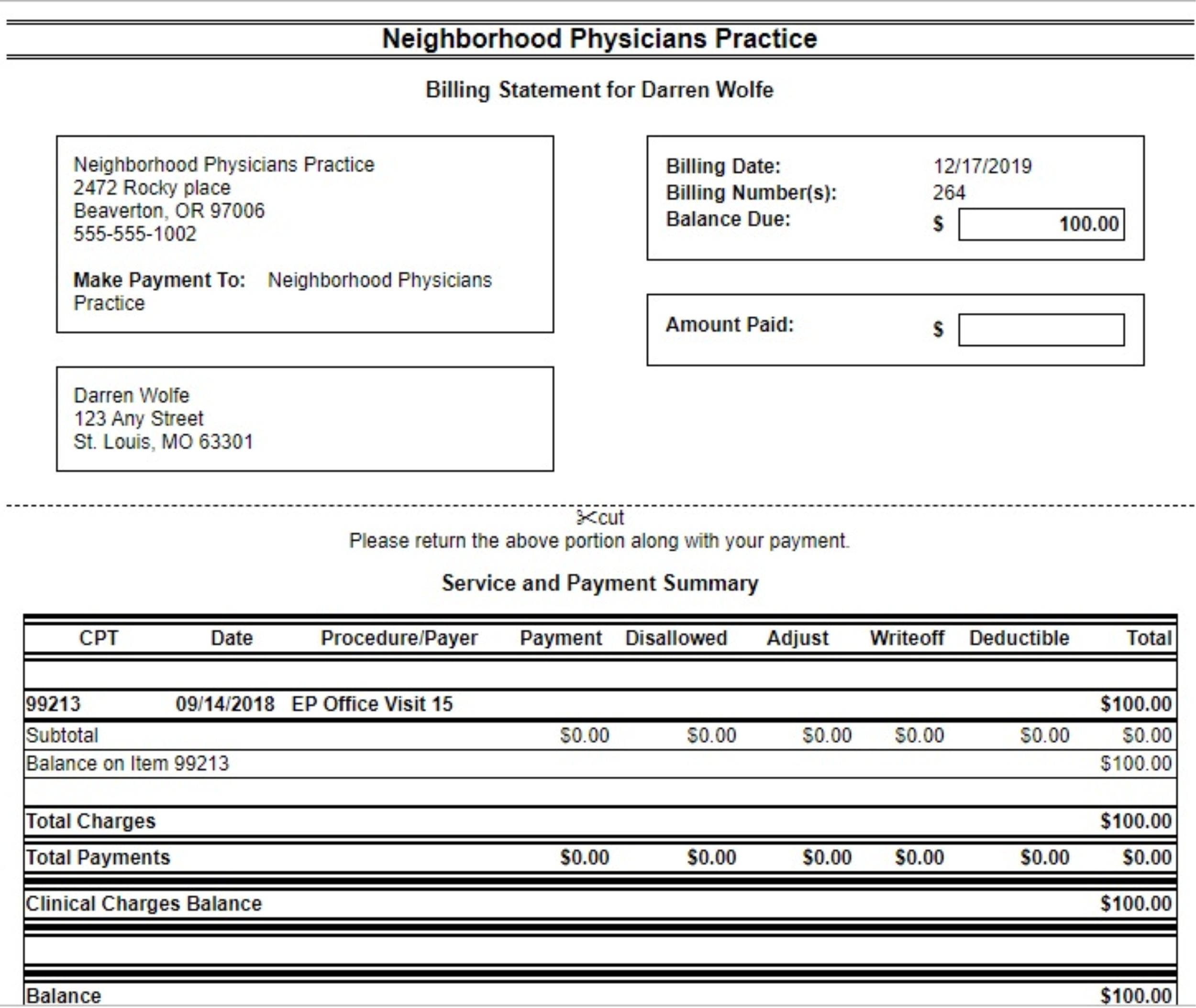
What is a CPT code?
Each procedure that your doctor or other health care provider performs has a billing code. This code is called the CPT code or Current Procedural Terminology. Providers use these codes when they submit claims to insurance companies or Medicare. The code determines how much your provider will be paid. Because there are thousands of billing codes, mistakes can happen. These billing errors can be fixed if you call the mistake to the attention of the provider. By changing the codes, providers can get paid differing amounts of money. When providers use the correct codes for the procedures actually done, they get paid what they are due.
What is an improper care complaint?
Improper care or unsafe conditions. You may have a complaint about improper care (like claims of abuse to a nursing home resident) or unsafe conditions (like water damage or fire safety concerns).
How to file an appeal with Medicare?
For questions about a specific service you got, look at your Medicare Summary Notice (MSN) or log into your secure Medicare account . You can file an appeal if you disagree with a coverage or payment decision made by one of these: 1 Medicare 2 Your Medicare health plan 3 Your Medicare drug plan
What is medical billing fraud?
Health insurance and medical billing fraud occurs when a health care provider or individual deceives an insurer in order to receive greater reimbursement. Examples of health insurance and medical billing fraud are: “Upcoding,” or billing for a more expensive service than the one actually performed. “Unbundling,” or billing each stage ...
What is billing for services not performed?
Billing for services not actually performed. “Upcoding,” or billing for a more expensive service than the one actually performed. “Unbundling,” or billing each stage of a procedure as if it were a separate procedure. Falsifying a patient's diagnosis to justify procedures that aren't medically necessary.
What is home health fraud?
Home health care fraud is when home health agencies bill insurers, government benefit programs, or homebound patients for unnecessary services or for services that were never delivered. This can also fall under Medicare or Medicaid fraud if the homebound patient receives home care as part of either benefit program.
What is health care fraud?
Health care fraud is a deliberate deception or misrepresentation of services that results in an unauthorized reimbursement. Health care abuse refers to practices that are inconsistent with accepted medical, business, or fiscal practices. These practices can take many forms, the most common including: The Consumer Protection Division of the Office ...
Where to file a Medicaid complaint in Texas?
To file a Medicaid complaint, contact the Austin headquarters. Mail: Medicaid Fraud Control Unit at the Office of the Attorney General, P.O. Box 12307, Austin, TX 78711-2307. Email: MFCU@oag.texas.gov.
What is the purpose of the Consumer Protection Division of the Office of the Attorney General?
The Consumer Protection Division of the Office of the Attorney General aims to help educate consumers on how to recognize fraud and abuse and how to file a complaint with the appropriate agency.
What is medical billing fraud?
Medical billing fraud is an intentional deception that results in an unauthorized payment. Examples include the following: Billing for services not provided. Up-coding which means a service was provided, but billed out at a higher level.
Is a bundled code fraud?
For procedures which require a number of steps and can be billed at one amount, a provider may instead bill them individually so they add up to more reimbursement. If a code is a bundled code and all components are billed separately, then this is considered fraud.