Pseudo- or real progression? An ovarian cancer patient …
22 hours ago · Clinicians should be aware of pseudoprogression, its underlying mechanisms and strategies to discriminate pseudo- from real progression in ovarian cancer. ... An ovarian … >> Go To The Portal
Is pseudoprogression a true tumor progression?
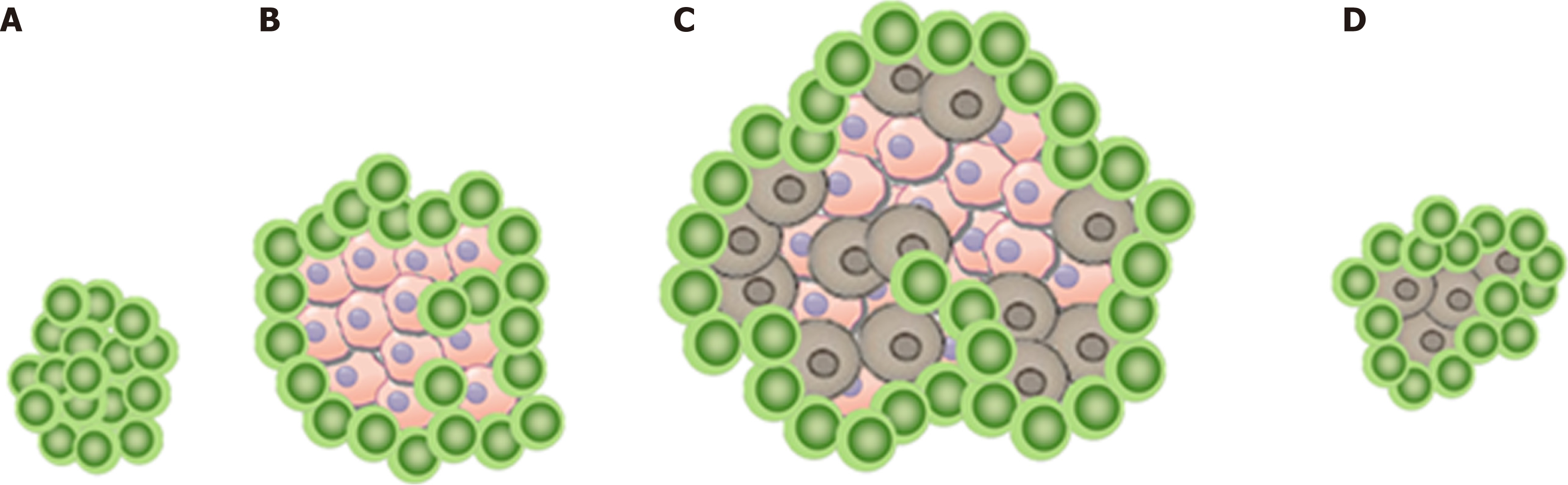
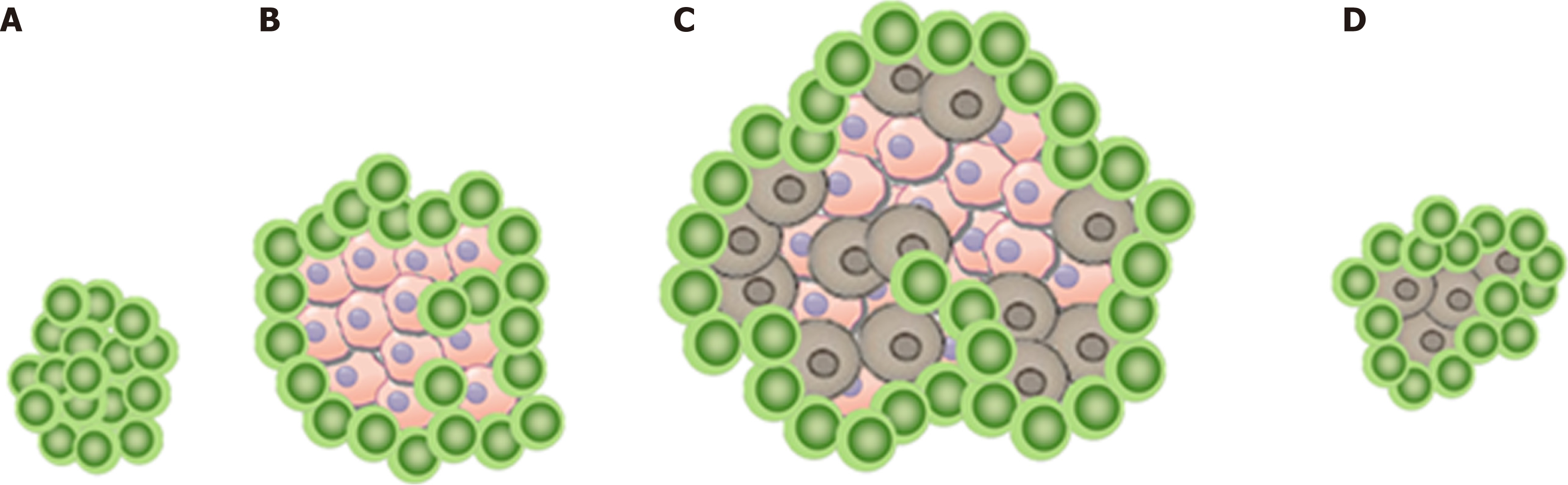
Pseudoprogression is not true tumor progression, which has been proven by histopathological biopsies that found infiltration and recruitment of various immune cells, such as T or B lymphocytes, in the tumor [9,10].
How is pseudoprogression diagnosed in melanoma?
Ultrasound (US) is a potential imaging method to detect pseudoprogression. US imaging detected pseudoprogression in metastatic melanoma patients undergoing PD-1 blockade with nivolumab by finding a decreased blood flow pattern in tumors [43]. US is superior in blood flow evaluation.
Can ICI cause pseudoprogression in cancer?
Treatment with ICI targeting PD-1 or PD-L1 may also result in pseudoprogression in other types of solid tumors, such as bladder cancer, breast cancer, colorectal cancer, esophageal cancer, gastric cancer, head and neck cancer, lung cancer, pancreaticoduodenal cancer, ovarian cancer, renal cell cancer, sarcoma, and uterine cancer [10].
Are imaging methods and biomarkers useful for pseudoprogression in immunotherapy?
These potential imaging methods and imaging biomarkers should be considered in subsequent exploration of pseudoprogression in immunotherapy. Although most of the existing studies on pseudoprogression and imaging in patients undergoing immunotherapy are preclinical, the outcomes are propitious and hopeful.
Abstract
Background Checkpoint-Inhibition has revolutionized the treatment for several entities such as melanoma and renal cell carcinoma. The first encouraging experience in ovarian cancer was reported for nivolumab, a fully humanized anti-programmed death-1 antibody.
INTRODUCTION
Cancer has different techniques to evade the immune system, one of those being Programmed death-1 (PD-1) signaling. PD-1 plays an important role in antitumor immunity as it is a vital part of a set of activating and inhibitory T cell receptors called “the immune checkpoint”.
FINAL DIAGNOSIS
A known lymph node metastasis was located in the patients’ left groin, but the lymph-node nearly doubled in size initially suggesting classic progression. But the lack of evidence for additional progression, the local inflammatory signs and the stable tumor marker CA125 made a pseudoprogression the most likely diagnosis.
TREATMENT
Because the RECIST do not provide a complete assessment of immune-therapeutic agents, ir-RECIST were defined by Wolchok et al [ 12 ]. In this adapted recommendation, the increase in tumor size or even the appearance of a new lesion, does not automatically translate to the classification as progressive disease.
OUTCOME AND FOLLOW-UP
Three weeks after the fourth cycle of nivolumab, she presented with rectal bleeding. A cysto-rectoscopy was performed, which demonstrated new tumor infiltration into the rectum. A biopsy was taken and the pathological analysis verified new relapse with infiltration into the rectum.
DISCUSSION
Nivolumab has been shown to be active in ovarian cancer, but the possibility of pseudoprogression imitating real progression remains [ 11 ].
CONCLUSION
This case illustrates not only pseudo-, but also real progression and vividly shows the main difference between the two: Only real progression has the ability to infiltrate other tissues.
What are the predictors of pseudoprogression?
Moreover, since distinguishing pseudoprogression from true tumor progression in brain tumors is a challenging task for clinicians, multiple molecular changes have been validated as potential predictors for pseudoprogression, including p53 [28], small extracellular vesicles [29] , O6-methylguanine-DNA methyltransferase methylated (MGMT) [30,31], interferon regulatory factor (IRF9), X-ray repair cross-complementing gene (XRCC1) [32], isocitrate dehydrogenase 1 (IDH1) [33], Ki67 expression [34], and CDH2 protein alone or in combination with ELAVL1 protein [35]. Despite the fact that these potential biomarkers could distinguish pseudoprogression from true progression, the actual predictive value of these markers remains unclear in immunotherapy as well as in other types of tumors, and thus, they need to be further explored.
How is pseudoprogression diagnosed?
Currently, pseudoprogression is diagnosed using retrospective imaging data , which critically impedes the optimal application of immune checkpoint inhibitors because clinicians cannot accurately evaluate the treatment. At the rate at which immunotherapeutics are widely being utilized to treat tumor patients, determining how to accurately discriminate pseudoprogression from true progression is quite important for helping clinicians to avoid premature cessation of immunotherapeutic treatment and initiation of alternative treatments. Several studies have elucidated that some potential methods and factors were able to predict pseudoprogression. Therefore, this review summarizes the existing studies on pseudoprogression in immunotherapy that aimed at determining earlier and more accurate methods of identifying pseudoprogression in patients receiving immunotherapeutics.
What biomarker is used to evaluate the efficacy of immunotherapy?
Chromosomal instability quantification of cfDNA is an effective indicator to evaluate the efficacy of immunotherapy [25]. Previous studies have reported cases of pseudoprogression that have manifested in decreased chromosomal instability quantification or genome instability number of cfDNA [25,26]. It is not surprising that an index for the evaluation of immunotherapy may also be a biomarker to identify pseudoprogression, and further studies are needed to explore this association. Interleukin-8 (IL-8) levels were reduced and maintained lower than baseline in three tumor patients who had partial responses after first exhibiting increases in tumor burden [27]. The level of IL-8 is not only an important clinical marker of pseudoprogression but also a biomarker to monitor the clinical benefit of immune checkpoint inhibitors. Thus, all biomarkers that are capable of assessing the efficacy of immunotherapeutics may also be utilized to identify pseudoprogression. Consequently, oncologists ought to pay more attention to these biomarkers in future studies and assessments of patients.
What is immunotherapy for cancer?
Over the last few years, immunotherapy, which induc es a persistent antitumor response in patients by stimulating immune recognition of tumors , has emerged as a promising treatment strategy for advanced tumors [1-3]. Immune checkpoint inhibitors (ICI), such as blockades that target programmed death-1 (PD-1), programmed death-ligand 1 (PD-L1), and cytotoxic T-lymphocyte associated antigen (CTLA-4), are one of the most powerful tools in the immunotherapy armamentarium and offer a beneficial immunotherapeutic regimen to patients with various types of cancers [4-8]. The emergence and wide use of ICI has resulted in a dramatic breakthrough in cancer immunotherapy.
What is hyperprogression in immunotherapy?
Hyperprogression is characterized as accelerated tumor progression and usually results in deterioration of disease following immunotherapy. Of note, a new pattern of progression, hyperprogression, is correlated with some predictive factors, including older age (more than 65 years old) [56], more than 2 metastatic sites [57], alterations of EGFR, MDM2/4 and DNMT3A [58], Pre-ICI dNLR, LDH, and concurrence of STK11 and KRAS mutations [59], but these predictive factors are poor at predicting hyperprogression.
Is pseudoprogression a clinical phenomenon?
Immunotherapy has achieved unprecedented clinical efficacy in patients with various types of advanced tumors; however, some patients experience delayed tumor shrinkage following an increase in tumor burden after such a therapeutic method. This phenomenon is called pseudoprogression and can lead to premature cessation of efficacious immunotherapeutic agents. Consequently, we summarized the available data on methods to differentiate pseudoprogression from true progression in patients who have been treated with immunotherapy including biomarkers, medical imaging techniques and biopsy. We also introduce hyperprogression and special pseudoprogression for improved evaluation of immunotherapy.
Is pseudoprogression continuous?
Pseudoprogression can also be continuous. In a patient with malignant melanoma, when their liver metastasis was shrinking, a new peritoneal nodule appeared that had a subsequent remission [53]. According to a case report by Curioni-Fontecedro et al. [54], diffuse pseudoprogression appeared in a NSCLC patient taking Nivolumab, manifesting as multiple enlargements and metastases of tumors with an improved general condition. Pseudoprogression is generally accompanied with an improved general condition, whereas a deteriorating general condition may indicate true progression or even hyperprogression [55].