FREE 14+ Patient Report Forms in PDF | MS Word
22 hours ago Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physicians, nurses, and doctors of medicine. It also includes the psychiatrists, pharmacists, midwives and other employees in the allied health. >> Go To The Portal
Patient medical reports serve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not. These reports are mandatory for the individual patient.
Full Answer
What reports are available for my practice?
Service Code and Type Productivity Reports Service Productivity Reports will show your practice production by service category and coding. These reports will show how many were charged out for the month/year, this year average fee and the productivity total for the current month and year to date. 6. Detailed Treatment Plans Report
What is a patient medical report?
A patient medical report is a comprehensive document that contains the medical history and the details of a patient when they are in the hospital. It can also be given as a person consults a doctor or a health care provider. It is a proof of the treatment that a patient gets and of the condition that the patient has.
Where can I get a sample patient report?
Sample Patient Report 1875 N. Lakes Place • Meridian, Idaho • 83646 • USA • 208-846-8448 • www.acugraph.com Note: This packet contains a sample patient report, printed from AcuGraph 4. Weʼve also included a few notes about how to read the reports.
Who has the access to the patient medical report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must.
How do you write a patient report?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
What should be included in a patient report?
A structured format incorporating elements of background information, medical history, physical examination, specimens obtained, treatment provided and opinion is suggested.
What are practice management reports?
Running practice management reports on a regular basis is a key factor in maintaining a healthy revenue cycle. Reports provide practice oversight by identifying areas where you may be unknowingly losing income. There are many types of reports, each providing a different lens through which to view your practice.
What is a patient report?
A patient report is a medical report that is comprehensive and encompasses a patient's medical history and personal details. It's often written when they go to a health service provider for a medical consultation. Government or health insurance providers may also request it if they need it for administration reasons.
Why is patient report important?
'It is vital to collate and monitor how drugs affect patients to help improve the efficacy of medicines and reduce mishaps and harm from wrong dose levels or by identifying patient groups who are particularly vulnerable.
What is the primary purpose of a patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool.
What is the purpose of practice management?
The American Medical Association defines the goal of healthcare practice management as enhancing practice efficiency, professional satisfaction and the delivery of patient care.
What is PM system in healthcare?
A medical practice management system is a type of healthcare software that manages the day-to-day operations of a clinic, such as appointment scheduling, billing and other administrative tasks.
What is the function of the practice management system?
Practice management software (PMS) is a type of software program used to operate medical and healthcare practices. Its core purpose is to help organize administrative tasks, streamline appointment bookings, simplify invoice creation and billing, and manage client or patient medical records.
What is a patient summary?
A Patient Summary is a standardized set of basic clinical data that includes the most important health and care related facts required to ensure safe and secure healthcare.
What are types of medical reports?
Medical records can be found in three primary formats: electronic, paper and hybrid.
What is a patient safety report?
Patient Safety Reporting (PSR) gives military treatment facility personnel the ability to anonymously report medical events that impact the safety of patients.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
What is a Patient Medical Report?
A patient medical report is a comprehensive document that contains the medical history and the details of a patient when they are in the hospital. It can also be given as a person consults a doctor or a health care provider. It is a proof of the treatment that a patient gets and of the condition that the patient has. It has the complete diagnosis on the patient, clearly stating the disease that should be treated. Through a patient medical report, anyone can analyze the health condition of a person. It sometimes contain a patient chart where the demographic profile of the patient is introduced. All types of medical records need a medical report. Patient medical records are simple data about the patient while a patient medical report is more elaborate and comprehensive. Though the importance of medical records and the purpose of medical records are almost the same with a patient medical report, the patient medical report is more beneficial. It has a complete summary of the diagnosis on the patient and have some recommendations for the health of the patient.
What should be documented in a patient's medical report?
One thing that a doctor should have documented in the patient medical report is the medical diagnosis that he has found in the patient. Whatever disease that a patient has should be clearly stated in the medical report. The name of the disease should be clearly written and some explanations about the current condition of the patient.
Why should a patient's medical report include lab results?
It is also needed because sometimes the laboratory and the test results are the proof of the sickness of the patient. For example, if the patient has a blood cancer, it can be seen with the blood tests. If the patient has a brain tumor, it can be seen through a brain CT scan. A CT scan for the body can also tell whether we have a fracture or not.
Why should medication be documented in a medical report?
The treatments or medications should also be documented because it can provide a good information about the medical history of a patient. Put the names of the medicines and tell how often did the patient takes it. You can also document its effect and tell whether it is effective for them.
What is a recommendation statement?
These are statements about the recommendations of the doctor. They are statements whether a patient can do a particular thing or not. It tell limitations on thing that they should not do for a while and it tell the abilities that they, of course, have. This is necessary so that the sickness will not get worse.
Is a medical report a legal document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patient is under your care. Thus, it can be used in court as an essential proof. So, keep a patient medical report because you may need it in the future.
Do health care providers have access to patient medical records?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report. It can be a proof if there is any doctor withholding treatments. So, to avoid conflict, the patient medical report should be shown to the patients. HIPAA (Health Insurance Portability and Accountability Act) has been passed in the Congress of United States. Passed in 1996, it specifies who can have an access to all the health information. You can research for that law, so you can have the exact details to who can have an access to a patient medical report. It is better because you can have a legal source. It can tell you all the things that you need to know about it.
What is patient case report?
Patient case reports are valuable resources of new and unusual information that may lead to vital research.
What should be included in the abstract of a patient case report?
The abstract of a patient case report should succinctly include the four sections of the main text of the report. The introduction section should provide the subject, purpose, and merit of the case report.
What do you write in a medical report?
Who should write the report, The name and preferably the date of birth of the patient concerned; The time and date of any incident; The purpose of the report; Any specific issues that need to be addressed.
What is a medical summary report?
The Medical Summary Report (MSR) is SOAR's signature tool and key to a successful application. It provides a succinct, comprehensive summary of the applicant's personal and treatment history and its impact on his or her life. It also clearly describes the factors affecting functioning and ability to work.
Why are patient forms at hospitals such a pain to fill out?
Usually there is a one or maybe a two-page form. I don't think they are that difficult to fill out. They copy my insurance card and that's it. Generally they include a brief list of history questions and current symptom questions. If it is a current doctor, only the current symptom questions. As I am not the one with the medical degree, I hope they use those answers to put two and two together in case my sore throat, indigestion, headache or fever is part of a bigger picture of something more seriously wrong. The HIPAA form is long to read, but you only need to do that once (although you'll be expected to sign the release each time you see a new doctor or visit a new clinic or hospital).
Why do patients have to fill out forms when visiting a doctor? Why isn't there a "Facebook connect" for patient history/information?
There are many (many) reasons - so I'll list a few of the ones that I can think of off-hand.Here in the U.S. - we have a multi-party system: Provider-Payer-Patient (unlike other countries that have either a single payer - or universal coverage - or both). Given all the competing interests - at various times - incentives are often mis-aligned around the sharing of actual patient dataThose mis-aligned incentives have not, historically, focused on patient-centered solutions. That's starting to change - but slowly - and only fairly recently.Small practices are the proverbial "last mile" in healthcare - so many are still paper basedThere are still tens/hundreds of thousands of small practices (1-9 docs) - and a lot of healthcare is still delivered through the small practice demographicThere are many types of specialties - and practice types - and they have different needs around patient data (an optometrist's needs are different from a dentist - which is different from a cardiologist)Both sides of the equation - doctors and patients - are very mobile (we move, change employers - doctors move, change practices) - and there is no "centralized" data store with each persons digitized health information.As we move and age - and unless we have a chronic condition - our health data can become relatively obsolete - fairly quickly (lab results from a year ago are of limited use today)Most of us (in terms of the population as a whole) are only infrequent users of the healthcare system more broadly (cold, flu, stomach, UTI etc....). In other words, we're pretty healthy, so issues around healthcare (and it's use) is a lower priorityThere is a signNow loss of productivity when a practice moves from paper to electronic health records (thus the government "stimulus" funding - which is working - but still a long way to go)The penalties for PHI data bsignNow under HIPAA are signNow - so there has been a reluctance/fear to rely on electronic data. This is also why the vast majority of data bsignNowes are paper-based (typically USPS)This is why solutions like Google Health - and Revolution Health before them - failed - and closed completely (as in please remove your data - the service will no longer be available)All of which are contributing factors to why the U.S. Healthcare System looks like this:===============Chart Source: Mary Meeker - USA, Inc. (2011) - link here:http://www.kpcb.com/insights/usa...
What is PCR in emergency care?
the aim of this audio-visual presentation is to provide clear guidance for the accurate completion of the patient care report recording pre-hospital care interventions and medications administered to patients is an essential clinical responsibility of all pre-hospital emergency care practitioners every responder and practitioner must provide clear accurate and comprehensive patient care information the PCR is a two-part pocket-sized report comprising 10 colored panels and folded in such a way that the written information flows easily from panel to panel without having to open it out on the Topkapi the following is recorded incident information patient demographic information clinical information vital observations medication treatment care management continuity of care clinical audit emergency department handover signature and additional information the second copy has four additional panels on the back for use by the practitioner to record the following out of hospital cardiac arrest
Can I esign a patient report from Gmail?
That goes for agreements and contracts, tax forms and almost any other document that requires a signature. The question arises ‘How can I eSign the patient report form app I received right from my Gmail without any third-party platforms? ’ The answer is simple - use the signNow Chrome extension.
How to write a case report?
Step 1: Identify the Category of Your Case Report. ... Step 2: Select an Appropriate Journal. ... Step 3: Structure Your Case Report According to the Journal Format. ... Step 4: Start Writing.
What are the symptoms of a rib infection?
Indications: Diseases of the chest and ribs--cardiac pain, palpitations, vomiting, acid reflux, plumpit qi ( the sensation of a foreign object in the throat); stomach pain; mania and depression; pain and weakness of the elbow and arm; malarial disease; red face and eyes; palpable abdominal masses; wind strike--epilepsy.
Why not needle perpendicularly?
Do not needle perpendicularly due to risk of pneumothorax.
Where is the 1.5 cun lateral to the lower border of the spinous process of T9?
1.5 cun lateral to the lower border of the spinous process of T9, at the highest visible point of the paraspinal muscles.
What is a patient visit summary?
The Patient Visit Summary is an “end-of-visit” clinical summary report. It details everything that happened during an appointment or other encounter. The report optionally includes an overview of other patient medical information. You can also customize what appears on the report and configure special components which will include patient instructions and other information.
Why would you record that a family declined the patient visit summary?
Why Would You Record That a Family Declined the Patient Visit Summary?: In order to meet Meaningful Use benchmarks or other mandate programs , your practice mght offer a Patient Visit Summary for each visit. Since the family may say, “no thanks”, you can click “Decline” to record their refusal and save the paper and ink for the report. PCC EHR will record the act of declining the report in the chart’s background event log. Your results on the Meaningful Use report will indicate that the family was offered the report.
Do allergies appear on patient visit summary?
For example, your practice may want future appointments and orders to appear, but you may decide that allergies and care plan information should not appear on the default Patient Visit Summary. Also, if your practice uses the Patient Visit Summary as a lab requisition form, or to communicate encounter information with other third-parties, you may want to check the “Display ICD-10” checkbox.
Can you add chart notes to patient visit summary?
You can add or remove any chart note components that you would like to appear on the Patient Visit Summary report as Chief Complaint or as Clinical Instructions. When you generate the report, PCC EHR will use any information it finds in the assigned components for the visit.
Can you record a patient visit report?
You can record when a patient or guardian declined to receive a Patient Visit Summary report for the day’s appointment.
Can you see hidden diagnoses in patient chart?
Hidden Diagnoses in the Patient Chart: Any diagnoses that are hidden or “locked” will not display in the Patient Visit Summary. To get a report that contains these diagnoses, use the Summary of Care Record.
What is a referral report?
Referral reports will aid in tracking how your new patients were referred to your practice. Review these reports on a monthly basis: Referral Productivity – Detailed and Summary and Top Referral Sources. Patients Currently Referred Out gives your office detail on patients that have been referred out to a specialty practice that may not have returned to your office after a referral.
What is the path of a practice?
The path on which your practice is headed is a key factor for tracking the “health” of your business and once you know where you are headed, it lets you know if you should continue on the current path, or evaluate and make a change. Regular use of these reports can make a difference in your practice success and the overall experience you provide for your patients.
What to do with overdue recall report?
Review your hygiene recare. Evaluating your overdue recall report processed with your Recall Wizard can assist with tracking your practice hygiene retention. Use these crucial reports for re-activating your hygiene patients.
What is service productivity report?
Service Productivity Reports will show your practice production by service category and coding. These reports will show how many were charged out for the month/year, this year average fee and the productivity total for the current month and year to date.
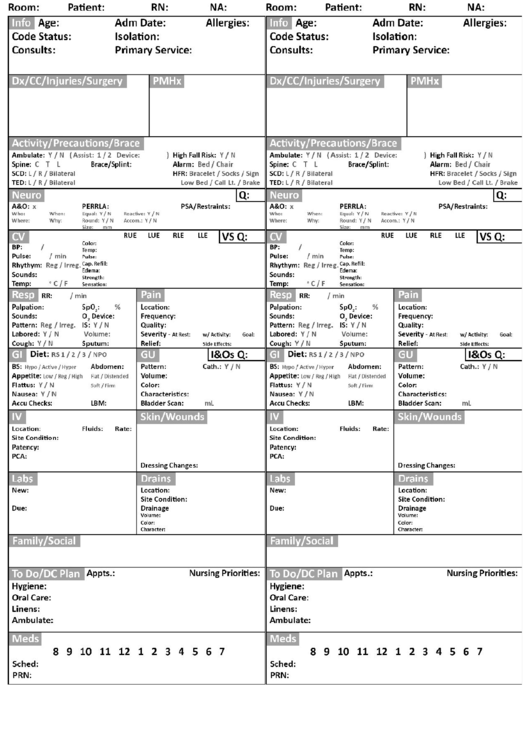
Why do nurses need a report sheet?
A nursing report sheet enables these nurses to keep a track of the tasks that they have to perform. This allows them to go through their activities, in an untroubled manner and without missing out on any of the tasks.
What is the first section of a nursing report?
General Information – The General Information section is the first section to be present in the Nursing Report. This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient. Patient Report – Next on the report, is the Patient Report section.
What is an ICU nursing report?
ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
What is patient monitoring?
Patient Monitoring: Vital Signs – The Patient Monitoring section contains the vital signs that have been recorded at some particular time during their stay at the healthcare center. A few of the most important characteristics which are present in all the nursing reports are the Time Check, Blood Pressure details, Heart Rate, Temperature, Oxygen Saturation Levels, Oxygen, Respiratory Rates, Pain (if any, that has been inflicting the patient), Blood Sugar Details, Details of Dispensed Medications and Medicine Administration Timing.
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
Why are nursing report sheets important?
These report sheets are highly beneficial in helping the medical staff to obtain information efficiently.
Why do physicians use EHR?
Most physician-owned practices adopted EHR to avoid government penalties and installed practice management program to run their business. But EHR and PM systems can work together when implemented correctly; enabling patient registrations become patient health records, for example. Similarly, diagnoses entered in the EHR can translate into properly coded insurance claims for faster payment.
Can a practice use all the features of their system?
Unfortunately, many practices don’t use all the features their system offers. Physicians and office managers may not know about their system’s more sophisticated capabilities, or they might lack the training to maximize the software’s potential.
What is a patient case study?
Writing Your Patient Case Study. Since patient case studies are generally descriptive, they are under the a phenomenological principle. This means that subjectivity is entertained and allowed in research design. The medical scenarios are open to the researcher’s interpretation and input of insights.
Why do medical practitioners use case studies?
Medical practitioners use case studies to examine a medical condition in the context of a research question. They perform research and analyses that adhere to the scientific method of investigation and abide by ethical research protocols. The following are case study samples and guides on case presentation.
What is case study in medical?
It is a well-established empirical research approach that illuminates a stand-out case of a subject or a group of subjects. In the end, it seeks to introduce new information for the understanding of the nature of a disease or medical condition in the context of someone who has lived it. Patient case studies make a difference in the medical arena by reporting clinical interactions that can improve medical practices, suggest new health projects, as well as provide a new research direction. By looking at an event as it exists in the natural setting, case studies shed understanding on a complex medical phenomenon.
How do case studies make a difference in the medical arena?
Patient case studies make a difference in the medical arena by reporting clinical interactions that can improve medical practices, suggest new health projects, as well as provide a new research direction. By looking at an event as it exists in the natural setting, case studies shed understanding on a complex medical phenomenon.
Should you look into all possible explanations for a medical condition?
You should look into all of the possible explanations for the medical condition at hand. If a plight can be explained by more than one reason , then you have to look into the less obvious but similarly compelling explanations. Make your case study as informative as possible.
Can you have multiple participants in a case study?
You can have one or multiple case participants. While other research methods boast of data credibility and generalizability, the small number of subjects in a case study is working for its advantage. The researcher is more attentive about his or her participants, and in-depth treatment of the study will not be very difficult. What case studies lack in generalized conclusions, they make up for thorough analysis of a subject matter.
Can you generalize a population using one case study?
You cannot generalize a population using one case study. However, multiple case study contains two or more cases under the point of interest can give you a replicated result. When the findings remain true for several cases under this research method, your case study’s results become more reliable.
