Portal Hypertension: Causes, Symptoms, Diagnosis
18 hours ago Portal hypertension is an increase in the pressure within the portal vein, which carries blood from the digestive organs to the liver. The most common cause is cirrhosis of the liver, but thrombosis (clotting) might also be the cause. Appointments 216.444.7000 Appointments & Locations Contact Us Symptoms and Causes Diagnosis and Tests >> Go To The Portal
Explore
Portal hypertension is an increase in the pressure within the portal vein, which carries blood from the digestive organs to the liver. The most common cause is cirrhosis of the liver, but thrombosis (clotting) might also be the cause. Appointments 216.444.7000 Appointments & Locations Contact Us Symptoms and Causes Diagnosis and Tests
How serious is portal hypertension?
Portal hypertension is elevated pressure in your portal venous system. The portal vein is a major vein that leads to the liver. The most common cause of portal hypertension is cirrhosis (scarring) of the liver. Portal Hypertension Symptoms
Is it okay to travel by flight with portal hypertension?
The initial mechanism in the genesis of portal hypertension is an increase in vascular resistance that can occur at any level within the portal venous system. Portal hypertension is therefore classified as prehepatic (portal or splenic vein thrombosis); intrahepatic (cirrhosis), and posthepatic (Budd-Chiari syndrome).
What is the prognosis for portal hypertension?
Portal hypertension is difficult to treat or cure. For that reason, your doctor will focus on preventing and managing complications and trying to reduce the pressure in your portal vein. The main complication of portal hypertension is bleeding from the varices, and many of the treatment options aim to manage the bleeding.
Why is Propranolol used for portal hypertension?
Patients with portal hypertension are at increased risk of infection and even mundane infections can cause multiorgan system failure and death. Renal failure can be the direct result of portal...
What happens when you have portal hypertension?
What is portal hypertension signs and symptoms?
What is the most common complication of portal hypertension?
How do you treat portal hypertension?
How is portal hypertension diagnosed?
Is portal hypertension serious?
How long can you live with portal hypertension?
What stage of liver disease is portal hypertension?
What are the 4 stages of cirrhosis of the liver?
- Stage I: Steatosis. The first stage of liver disease is characterized by inflammation of the bile duct or liver. ...
- Stage II: Scarring (fibrosis) of the liver due to inflammation. ...
- Stage III: Cirrhosis. ...
- Stage IV: Liver failure or advanced liver disease or hepatic failure.
Can you recover from portal hypertension?
Is portal hypertension painful?
If a large amount of fluid accumulates in the abdomen, the abdomen swells (distends), sometimes noticeably and sometimes enough to make the abdomen greatly enlarged and taut. This distention can be uncomfortable or painful.
Can hypertension cause liver damage?
Can portal hypertension be diagnosed?
For patients with end-stage liver disease who present with ascites and varices, the doctor may not need to perform any diagnostic tests and can confirm a diagnosis based on symptoms.
What is the best way to diagnose portal hypertension?
Endosco pic Diagnosis. Endoscopy is another way to diagnose varices, which are large vessels associated with portal hypertension. An endoscopy can provide a definitive diagnosis of the varices and allow your doctor to treat and reduce the risk of bleeding or active bleeding. During a gastrointestinal endoscopy, your doctor can see ...
How to tell if you have ascites?
Ascites is excess fluid in your abdominal cavity. Patients with chronic liver disease often develop ascites, though it may be caused by other factors. Symptoms of ascites include: 1 Early feeling of fullness 2 Increase in size of abdomen 3 Feeling out of breath (if the fluid begins pushing on your lungs)
How to do an endoscopy?
During an upper endoscopy: 1 You receive an anesthetic to help relax your gag reflex. You will also receive pain medication and a sedative. 2 You lie on your left side, referred to as the left lateral position. 3 Your doctor inserts the endoscope (a thin, flexible, lighted tube with a camera) through your mouth and pharynx, into the esophagus. 4 Your doctor can visualize the esophagus, stomach and duodenum with the endoscope.
Can cirrhosis cause portal hypertension?
If you have an advanced liver disease, such as cirrhosis, you have an increased risk of developing portal hypertension. Be aware of unusual symptoms and report them to your doctor right away. Symptoms and signs of portal hypertension include:
What is a Doppler ultrasound?
A Doppler ultrasound uses sound waves to see how the blood flows through your portal vein. The ultrasound gives your doctor a picture of the blood vessel and its surrounding organs, as well as the speed and direction of the blood flow through the portal vein.
What is the purpose of a radiologist's pressure study?
An interventional radiologist may perform a pressure measurement study to evaluate the level of pressure in the hepatic (liver) vein. This can be done as an outpatient, where a radiologist will access one of your veins, usually via internal jugular vein.
What is the mechanism of portal hypertension?
The initial mechanism in the genesis of portal hypertension is an increase in vascular resistance that can occur at any level within the portal venous system. Portal hypertension is therefore classified as prehepatic (portal or splenic vein thrombosis); intrahepatic (cirrhosis), and posthepatic (Budd-Chiari syndrome).
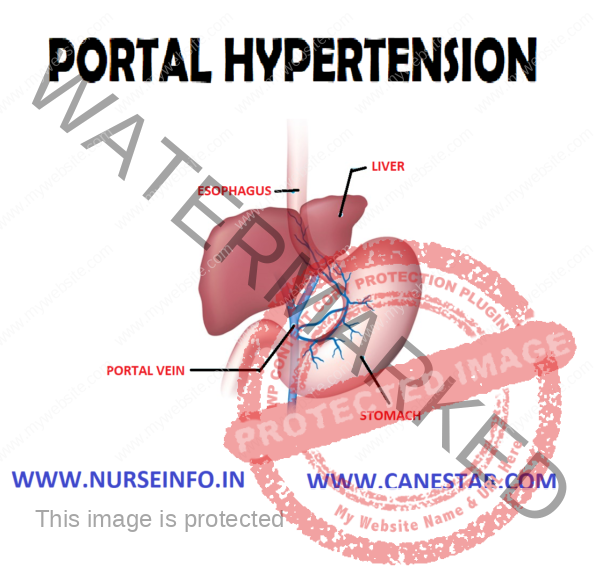
What is the portal vein?
Anatomically, the portal vein is formed by the union of the superior mesenteric vein and the splenic vein. The mesenteric vein collects blood from the splanchnic circulation. Thus, portal venous inflow is determined by the state of constriction or dilatation of splanchnic arterioles.
Is HVPG safe?
Pharmacologic therapies should thus be ideally tailored to a target decrease in HVPG. Even though the HVPG procedure is simple and safe, its use is not widespread in the United States because it is invasive and because it has not been appropriately standardized.17. Pharmacologic Therapy for Portal Hypertension.
What is terlipressin analogue?
Terlipressin is a synthetic vasopressin analogue that releases its active form, lysine vasopressin, after 3 glycyl residues are cleaved by endogenous proteases. Because this is a gradual process, the hormone is released slowly, in a sustained manner, minimizing the rate and severity of side effects.
Is carvedilol a vasodilator?
However, these combinations are associated with more side effects, specifically fluid retention and/or symptomatic hypotension. Carvedilol is a nonselective β-blocker with weak anti-α1adrenergic (vasodilator) activity and therefore acts as a combination of NSBB and vasodilator.
What are the side effects of NSBB?
The most frequent side effects related to NSBB reported in cirrhosis are lightheadedness, fatigue, and shortness of breath. Some of them disappear with time or after dose reduction. In clinical trials, side effects have led to the discontinuation of NSBB in approximately 15% of the patients.
What is portal hypertension?
Portal hypertension is a pressurein the portal venous system that is at least 5 mm Hg higher than the pressure in the inferior vena cava. This increased pressureresults from a functional obstruction to blood flow from any point in the portal system's origin (in the splanchnic bed) through thehepatic veins (exit into the systemic circulation) or from an increase in blood flow in the system.
Is portal venous hypertension life threatening?
Complications secondary to portal venous hypertension can be life threatening and are often the main indication for transplantation in patients with advanced liverdisease. Although there are several collaterals between portal and systemic venous circulation, those at the junction of the stomach and esophagus are particularlyimportant. The dilated portosystemic collaterals at the junction of the stomach and esophagus are termed varices (Figure 20).
What is the most common cause of portal hypertension?
Cirrhosis is the most common cause of portal hypertension, and chronic viral hepatitis C is the most common cause of cirrhosis in the United States. Alcohol-inducedliver disease and cholestatic liver diseases are other common causes of cirrhosis. Less common causes include hemochromatosis, alpha 1-antitrypsin deficiency,drug-induced liver disease, and (in Eastern countries) hepatitis B. Portal hypertension is considered an advanced complication of cirrhosis. Once it has developed, theterm "decompensated cirrhosis" is used (Figure 5).
What is the purpose of shunting in portal hypertension?
The aim of surgical shunting in portal hypertension is threefold: 1) to reduce portal venous pressure, 2) to maintain hepatic and portal blood flow, and 3) to try toreduce or not complicate hepatic encephalopathy ( Figure 16). Currently, there is no procedure that reliably and consistently fulfills all of these criteria.
What is the normal portal vein pressure?
Venous pressure morethan 5 mm Hg greater than the inferior vena cava pressure is defined as portal hypertension. Clinically it may be difficult to detect portal hypertension until pressuresare much higher. There are many causes of portal hypertension including etiologies above the liver, within the liver, and below the liver.
Is portal pressure measurement invasive?
Clinically it is used toassess the efficacy of pharmacological agents or shunting procedures. Most approaches to portal pressure measurement are relatively invasive, with the exception of newer endoscopic techniques.
What is the standard diagnostic approach in patients with acute gastrointestinal hemorrhage after initial resuscitation
Endoscopy is the standard diagnostic approach in patients with acute gastrointestinal hemorrhage after initial resuscitation. In most patients with cirrhosis (60–80%)bleeding is related to esophageal varices. In addition to making a definitive diagnosis, endoscopic therapy may be indicated for bleeding. Endoscopic examinationmay require endotracheal intubation in patients who have significant alteration in mental status as a result of severe hepatic decompensation.
What are the symptoms of portal hypertension?
Gastrointestinal bleeding with a low platelet count may be the first symptom of portal hypertension. Depending on the severity of liver disease, symptoms may also include ascites (fluid collection in the abdominal cavity), jaundice, hepatic encephalopathy, coagulopathy (slow clotting), or spider angiomata.
Is portal hypertension invasive?
Pressure measurement of the portal system is possible, but it is invasive and usually not practical. Portal hypertension is a term for elevated pressures in the blood vessels that drain the intestinal tract and spleen into the liver (portal circulation).
What causes hypertension in the liver?
Any condition or abnormality that changes the blood flow, and therefore the pressure within the vessels, can cause hypertension. The cause of the increased pressure in the portal venous system may be above the liver (suprahepatic), within the liver (hepatic) or below the liver (infrahepatic), and may include cardiac disease, hepatic vein thrombosis (Budd-Chiari syndrome), cirrhosis and arteriovenous malformations (AVMs) within the splenic vasculature.
Is Doppler Ultrasonography invasive?
Magnetic resonance imaging (MRI) and computed tomography (CT) may also provide valuable information. Pressure measurement of the portal system is possible, but it is invasive and usually not practical.
Where do varices develop?
Depending on the severity of liver disease and/or portal hypertension, varices may develop in the esophagus and in the stomach. What are varices? +. Varices are blood vessels that have dilated due to higher pressure.
Why do varices bleed?
They appear similar to varicose veins. These dilated and out-pouched vessels are prone to bleeding because the vessel walls are weakened from increased pressure. Larger varices have thinner walls and are more prone to bleed.
What is a shunting procedure?
Shunting or stenting procedures may be performed to change the blood flow and thereby decrease portal pressure. Transjugular intrahepatic portal systemic shunting is a nonsurgical, radiological procedure. Surgical shunts may also be used to reduce venous pressure and to maintain hepatic and portal blood flow.
WHAT YOU NEED TO KNOW
Portal hypertension is high blood pressure in the portal vein of your liver. Your portal vein is the main blood supply for your liver. Follow-up care is important, because this condition can be life-threatening. Talk to your healthcare provider if you need help to stop drinking alcohol. Ask which medicines you should not take with this condition.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
Medicines
Beta-blockers lower the blood pressure in your portal vein. This is done by slowing your heart rate and making your blood vessels wider. This may prevent damage to your liver and help prevent bleeding.
Monitoring
Your healthcare provider will monitor you to check for signs that you are developing esophageal varices or hepatic encephalopathy. Ask your him or her for more information on these and other conditions you may develop from portal hypertension.
Tests
Blood tests will be done to show how well your liver is working, or if you have problems with blood clotting.
RISKS
You may develop swollen veins in your esophagus. These are called esophageal varices. These veins may start to bleed, and cause severe blood loss. Your brain may become damaged if your liver can no longer filter toxins from your blood. Blood pressure and fluid may build around your lungs and abdomen. This may make it hard to breathe.
CARE AGREEMENT
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.
