What Therapists Are Legally Obligated To Report Despite …
2 hours ago Medical care is a service, and as the consumer of that service, you have the right to make your voice heard if you have a complaint. AHRQ has compiled some useful resources to help you better communicate with your health provider, and to learn how to file a complaint should it become necessary. You can also contact your state’s medical ... >> Go To The Portal
Can a therapist be forced to report a patient who threatens someone?
A therapist may be forced to report information disclosed by the patient if a patient reveals their intent to harm someone else. However, this is not as simple as a patient saying simply they “would like to kill someone,” according to Jessica Nicolosi, a clinical psychologist in Rockland County, New York.
How do you report a reportable disease?
Reportable diseases are divided into several groups: Mandatory written reporting: A report of the disease must be made in writing. Mandatory reporting by telephone: The provider must make a report by phone. Report of total number of cases. Cancer.
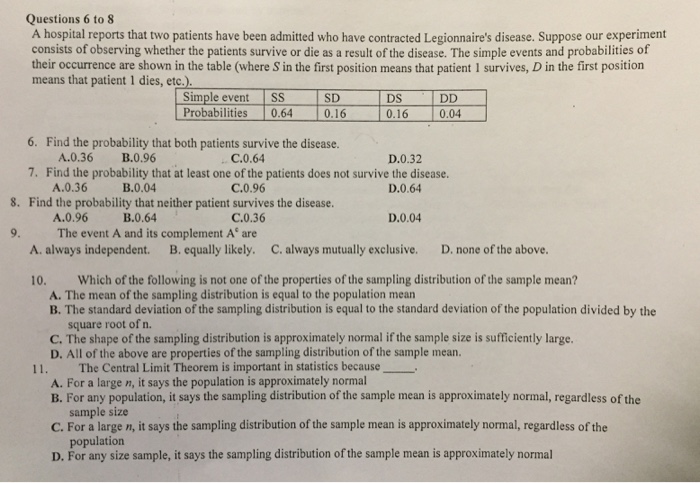
What are the reporting laws for therapists?
Laws in all 50 states require a therapist to contact authorities if a patient is a danger to him/herself, to others, and/or if the therapist suspects that a known child is being abused. These reporting laws, as they are applied in your state, are explained to all adults and to guardians of children who seek professional counseling for any reason.
What should a doctor do before reporting suspected violence or abuse?
Before reporting suspected violence or abuse, the Code says physicians should: Inform patients about requirements to report. Obtain the patient’s informed consent when reporting is not required by law.
What to consider before reporting suspected violence?
What to consider before reporting. Before reporting suspected violence or abuse, the Code says physicians should: Inform patients about requirements to report. Obtain the patient’s informed consent when reporting is not required by law.
How many victims of trafficking had contact with a health professional?
The authors noted research showing that 88% of victims had contact with a health professional while being trafficked, but none were identified or offered help in getting out of their situation during the medical encounter.
What is the abuse in the exam room?
Patients in your exam room may be experiencing one of a number of forms of abuse—domestic violence, human trafficking or other violence— and identifying those being abused can sometimes be tough.
Can a physician make exceptions to patient privacy?
Exceptions can be made if a physician reasonably believes that a patient’s refusal to authorize reporting is coerced and therefore does not constitute a valid informed treatment decision. Physicians should also protect patient privacy when reporting by disclosing only the minimum necessary information.
Do you have to see one on one for a trafficked patient?
Dr. Ravi said it is also important to establish a policy—even putting it in writing in the exam and waiting rooms—that says a patient needs to be seen one-on-one for part of the visit. Trafficked patients may come in with a man or woman who is trafficking them; sometimes that person could even be a relative.
Why is mandatory reporting required?
Mandatory reporting of persons believed to be at imminent risk for committing violence or attempting suicide can pose an ethical dilemma for physicians, who might find themselves struggling to balance various conflicting interests. Legal statutes dictate general scenarios that require mandatory reporting to supersede confidentiality requirements, but physicians must use clinical judgment to determine whether and when a particular case meets the requirement. In situations in which it is not clear whether reporting is legally required, the situation should be analyzed for its benefit to the patient and to public safety. Access to firearms can complicate these situations, as firearms are a well-established risk factor for violence and suicide yet also a sensitive topic about which physicians and patients might have strong personal beliefs.
How does a firearm affect a physician?
Depending on their personal experience with guns, physicians might have varying levels of concern about or comfort with the implications of a firearm’s involvement in a given case . They might also be hesitant to question a patient further on the topic, as they might be concerned about offending the patient by asking about what many perceive to be a private issue. However, ascertaining the types of guns owned, how they are stored, and if the patient has any intentions of using them are important components of risk assessment.
Why did Thomas struggle to sleep?
After a painful breakup with his long-time girlfriend, Thomas struggled to get over feeling angry about his girlfriend’s decision to end their relationship. Specifically, Thomas was unable to sleep well, despite trying numerous over-the-counter sleep aids. He decided to make an appointment with Dr. B to get a prescription for something that might help.
Can a physician tell a patient that the information will be shared with another party?
In many cases, physicians might choose to tell the patient, as Dr. B did, that the information will be shared with another party.
Do medical laws fit into real life cases?
Despite their attempts at specificity, these laws often do not fit neatly onto real-life patient cases. In some jurisdictions, the statements made by the patient can meet the threshold at which a physician is mandated to report in order to warn or protect a potential victim.
What is a reportable disease?
Reportable diseases are diseases considered to be of great public health importance. In the United States, local, state, and national agencies (for example, county and state health departments or the United States Centers for Disease Control and Prevention) require that these diseases be reported when they are diagnosed by doctors or laboratories.
Why is reporting important?
Reporting allows for the collection of statistics that show how often the disease occurs. This helps researchers identify disease trends and track disease outbreaks. This information can help control future outbreaks.
What is mandatory reporting?
Mandatory written reporting: A report of the disease must be made in writing. Examples are gonorrhea and salmonellosis. Mandatory reporting by telephone: The provider must make a report by phone. Examples are rubeola (measles) and pertussis (whooping cough). Report of total number of cases.
What are some examples of diseases reported to the CDC?
Examples are chickenpox and influenza. Cancer. Cancer cases are reported to the state Cancer Registry. Diseases reportable to the CDC include: Arboviral diseases (diseases caused by viruses spread by mosquitoes, sandflies, ticks, etc.) such as West Nile virus, eastern and western equine encephalitis.
Why do therapists need specific information?
Therapists need specific information in order to contact authorities. Most of the time professionals need specific information about a particular child who is at risk or who has been already harmed along with information about who is being abusive in order to take the step of filing a report.
What form do you need to read before you start therapy?
Before beginning therapy clients or guardians (if the client is a minor) should be asked to read and sign a consent form that explains the circumstances under which your therapist must break confidentiality. If the client is a minor then the information should be clearly explained to the parent or guardian.
Do therapists have to inform clients of a report?
In addition, the therapist may not be required to inform a client or their family that a report is being made. You can ask ahead of time about how this would be handled should the therapist consider filing.
Is everything you share with a therapist confidential?
Not everything you share with a therapist can be kept confidential. What an individual tells his or her therapist is confidential; however, there are limitations to the confidentiality between a therapist and a client. Laws in all 50 states require a therapist to contact authorities if a patient is a danger to him/herself, to others, ...
Who must report child abuse?
If a counselor believes an adult client has abused or neglected a child, dependent adult or elder person, the therapist must report the crime. He also must report anyone he reasonably suspected to have viewed or downloaded child pornography.
What happens if a therapist tells his therapist he can't stop thinking about raping
But if he told his therapist that he can’t stop thinking about raping the teenage girl next door, she is legally required to report the crime to the girl’s parents or the police. These kind of limits to therapist confidentiality in criminal cases are not limited to the informed parties either.
What is confidentiality in a therapist?
Therapist Confidentiality: Crimes Involving a Psychologist. Additionally, the limits to therapist/patient confidentiality mean that a mental health professional is not required to keep discussions confidential if a patient tries to use them in order to commit a crime.
Do therapists have to report crimes?
While therapists do not need to report crimes that have already happened in most cases, there are exceptions when it comes to therapist confidentiality in crimes involving crimes against children, the disabled or the elderly. This applies to both adult clients who may have committed crimes against their children or clients under 16 who have had ...
Can a psychiatrist tell if a patient has ADHD?
For example, if a patient tells her psychiatrist that she has ADHD and needs a prescription for Ritalin, but the psychiatrist can tell she is lying simply in order to obtain pills to get high, the doctor is no longer restricted by patient/doctor confidentiality laws.
Can a therapist break confidentiality?
If the patient is a minor under 16 and the therapist has reason to believe that she has been the victim of a crime and the therapist believe s it is in her best interest to report the crime, the therapist can choose to break patient confidentiality.
Do psychologists have to break confidentiality?
The most famous limits to therapist confidentiality and criminal situations is when a therapist is legally required to break confidentiality if he or she believes the patient may hurt himself or someone else. While the most obvious example of this is the mandatory institutionalization of someone who is likely to commit suicide, psychologists are also require to report patients to the police or victim if the patient indicates he or she will commit a crime against someone else.
What to do if you feel your treatment is abusive?
If you feel your treatment, verbal or physical, was abusive, and it could have a negative effect on other patients, then you may want to file a more formal, written complaint to authorities who license or hire the doctor. Respectful communication is required in all healthcare interactions. Don't settle for anything less.
What is an insulted person?
The insulted party is the person who receives the insult, the person who hears, sees, or experiences it and takes offense.
Case
Commentary
Disclosing Protected Health Information
Counseling Patients About Firearm Safety
When Is Reporting Required?
- Physicians also face the difficult task of deciding whether or not the situation constitutes enough of a risk to breach the patient’s confidentiality. In many cases, physicians might choose to tell the patient, as Dr. B did, that the information will be shared with another party. However, in situations in which this information might further agitat...
Conclusion
Popular Posts:
- 1. patient portal texas neurology
- 2. towne lake primary care patient portal
- 3. jefferson patient portal sigin
- 4. aarp medicare complete patient login
- 5. klamath orthopedic patient portal
- 6. patient healthcare portal ims care portal
- 7. spanish peaks family clinic patient portal pin number
- 8. women's physicians of jacksonville patient portal
- 9. one source patient portal
- 10. smhc physician services patient portal access information