Reporting Patient Safety Events | PSNet
29 hours ago · Background and Significance. A patient safety event is defined as any process, act of omission, or commission that results in hazardous healthcare conditions and/or unintended harm to the patient [ 1].Reporting patient safety events is a useful approach for improving patient safety [ 2].The mechanism of event reporting was first introduced in the high-risk industries … >> Go To The Portal
Patient safety events may be categorized as reportable events with outcome assessed by harm scale, reportable events resulting in permanent patient harm, intervention to sustain life, or patient death; and reportable events referenced by other reporting rules.
What is patient safety data reporting?
Reporting patient safety events is the main way we identify and address patient safety issues We can’t fix what we don’t know about Reporting helps us to learn about safety problems so that we can fix them
What is a patient safety reporting program?
The Patient Safety Reporting System (PSRS) is a non-punitive, confidential, and voluntary program which collects and analyzes safety reports submitted by healthcare personnel. Staff can report close calls, suggestions, and incident / event related information and data to improve patient safety.
What is a patient safety event?
We don’t understand well enough the preconditions and root causes of adverse events, making it difficult to prevent ... each with a fraction of the responsibility for patient and health care worker safety, did not serve us well during this pandemic ...
What is a patient safety report?
Patient safety; Report a patient safety incident; Report a patient safety incident. Patient safety incidents are any unintended or unexpected incident which could have, or did, lead to harm for one or more patients receiving healthcare. Reporting them supports the NHS to learn from mistakes and to take action to keep patients safe.
What is safety event report?
Despite its flaws, safety event reporting is an important tool for identifying system hazards and aggregate data, and sharing lessons within and across organizations. Systems can share known fail points in care, which allow other systems to identify that as a potential risk within their own organization.
What are patient safety reports?
Patient Safety Reporting (PSR) gives military treatment facility personnel the ability to anonymously report medical events that impact the safety of patients.
What types of events should be reported in a safety report?
Events that affect staff safety should be reported as well. Staff can also report “near miss” or potential events, things that were caught before patients or family members were impacted but that could have been a problem if the staff had not noticed in time.
Are sentinel events required to be reported?
Self-reporting a sentinel event is not required and there is no difference in the expected response, time frames, or review procedures whether the hospital voluntarily reports the event or The Joint Commission becomes aware of the event by some other means.
What is a report of an event?
An event report, also known as a post-event report or event summary, is a document that gathers all the success metrics and other data that illustrate the performance of your event.
What is an incident report?
An incident report is a tool that documents any event that may or may not have caused injuries to a person or damage to a company asset. It is used to capture injuries and accidents, near misses, property and equipment damage, health and safety issues, security breaches and misconducts in the worksite.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What is an event report healthcare?
The Event Reporting System (EVR) shall be used to report any occurrence that is not consistent with routine operations that may potentially or actually result in injury, harm, or loss to any patient or visitor at UCLA Health System and outpatient clinics.
What is a safety event?
A Safety Event is a situation where best or expected practice does not occur. If this is followed by serious harm to a patient, then we call it a “Serious Safety Event (SSE)”.
What is a major reason sentinel events should be reported quickly?
What is a major reason sentinel events should be reported quickly? So that the issue can be corrected and patient safety and comfort can be re-established.
What should be reported to The Joint Commission?
Quality Reports include:Accreditation decision and date.Programs and services accredited by The Joint Commission and other bodies.National Patient Safety Goal performance.Hospital National Quality Improvement Goal performance.Special quality awards.
What is a sentinel event alert?
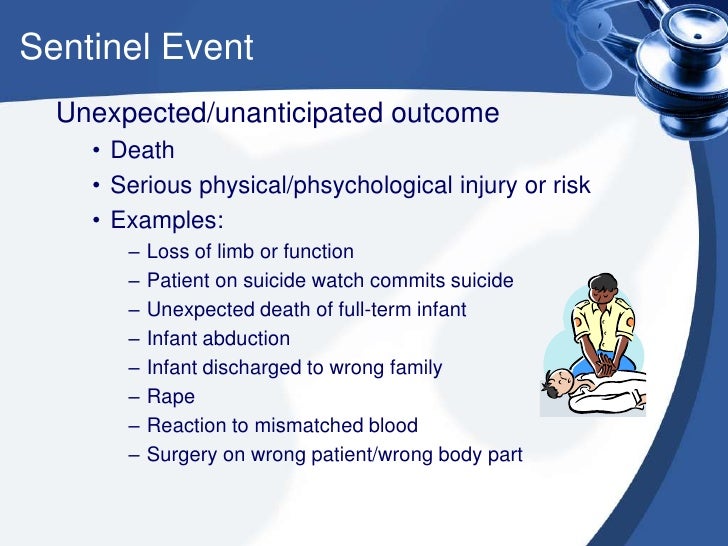
Since 1998, The Joint Commission has issued sentinel event alerts in response to unexpected incidents involving death or serious physical or psychological injury (or risk thereof). These events are identified as sentinel due to the gravity of the injury and the need for immediate investigation and response.
What is patient safety?
Patient Safety is a health care discipline that emerged with the evolving complexity in health care systems and the resulting rise of patient harm in health care facilities. It aims to prevent and reduce risks, errors and harm that occur to patients during provision of health care.
When is World Patient Safety Day?
Recognizing that Patient Safety is a global health priority, the World Health Assembly (WHA) adopted a resolution on Patient Safety which endorsed the establishment of World Patient Safety Day to be observed annually by Member States on 17 September.
Why does patient harm occur?
For example, a patient in hospital might receive a wrong medication because of a mix-up that occurs due to similar packaging. In this case, the prescription passes through different levels of care starting with the doctor in the ward, then to the pharmacy for dispensing and finally to the nurse who administers the wrong medication to the patient. Had there been safe guarding processes in place at the different levels, this error could have been quickly identified and corrected. In this situation, a lack of standard procedures for storage of medications that look alike, poor communication between the different providers, lack of verification before medication administration and lack of involvement of patients in their own care might all be underlying factors that led to the occurrence of errors. Traditionally, the individual provider who actively made the mistake (active error) would take the blame for such an incident occurring and might also be punished as a result. Unfortunately, this does not consider the factors in the system previously described that led to the occurrence of error (latent errors). It is when multiple latent errors align that an active error reaches the patient.
How many hospitalized patients have health care-associated infections?
Health care-associated infections occur in 7 and 10 out of every 100 hospitalized patients in high-income countries and low- and middle-income countries respectively (11).
What is the WHO patient safety and risk management unit?
The Patient Safety and Risk Management unit at WHO has been instrumental in advancing and shaping the patient safety agenda globally by focusing on driving improvements in some key strategic areas through:
How many people are harmed in hospitals?
In high-income countries, it is estimated that one in every 10 patients is harmed while receiving hospital care (2). The harm can be caused by a range of adverse events, with nearly 50% of them being preventable (3).
Why is patient safety important?
Patient safety is fundamental to delivering quality essential health services. Indeed, there is a clear consensus that quality health services across the world should be effective, safe and people-centred. In addition, to realize the benefits of quality health care, health services must be timely, equitable, integrated and efficient.
What is the number to call 911?
If you are having thoughts of harming yourself, please call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255). Online: Submit a new patient safety event or concern. Online: Submit an update to your incident (You must have your incident number)
Can the Joint Commission accept medical records?
By policy, The Joint Commission cannot accept copies of medical records, photos or billing invoices and other related personal information. These documents will be shredded upon receipt. Download the form for reporting a patient safety concern by mail.
Who receives patient safety events?
Patient safety events: The Joint Commission receives reports of patient safety events from patients, families, government agencies, the public, staff employed by organizations, and the media. This information is used to help improve the quality and safety of accredited organizations. Patient safety events can be reported to the Joint Commission ’s Office of Quality and Patient Safety.
What is a patient safety collaborative?
National Patient Safety Collaborative, established in January 2018, is a voluntary collaborative of prominent, national patient safety organizations that works collectively on mutually identified safety concerns. Member organizations are: Association for the Advancement of Medical Instrumentation; ECRI Institute; Institute for Safe Medication Practices; Institute for Healthcare Improvement; and The Joint Commission.
What is sentinel event policy?
Sentinel Event Policy: Implemented in 1996, The Joint Commission’s Sentinel Event Policy was revised in 2014 to incorporate contemporary patient safety concepts and clarify Joint Commission processes. Any time a sentinel event occurs, the organization is expected to conduct thorough and credible comprehensive systematic analyses (for example, root cause analyses), make improvements to reduce risk, and monitor the effectiveness of those improvements. The analyses are expected to drill down to underlying organization systems and processes that can be altered to reduce the likelihood of a failure in the future and to protect patients from harm when a failure does occur. Sentinel events are one category of patient safety events (see below). Accredited organizations are strongly encouraged, but not required, to report sentinel events.
What is the Association for the Advancement of Medical Instrumentation Foundation?
Association for the Advancement of Medical Instrumentation Foundation works toward the development, management, and use of safe and effective healthcare technology.

Characteristics of Incident Reporting Systems
- An effective event reporting system should have four key attributes: While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic …
Limitations of Event Reporting
- The limitations of voluntary event reporting systems have been well documented. Event reports are subject to selection bias due to their voluntary nature. Compared with medical record review and direct observation, event reports capture only a fraction of events and may not reliably identify serious events. The spectrum of reported events is limited, in part due to the fact that ph…
Using Event Reports to Improve Safety
- A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require furth…
Current Context
- At the national level, regulations implementing the Patient Safety and Quality Improvement Act became effective on January 19, 2009. The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to wo…