Pelvic Pain in Women | Causes and Treatment | Patient
18 hours ago · If the abdominal organs are impaired due to normal processes or illness, this can result in pelvic pain. Infection and inflammation of the appendix. Constipation and gas. Intestinal contractions: The intestines … >> Go To The Portal
Pelvic pain might be a symptom of infection or might arise from pain in the pelvis bone or in non-reproductive internal organs. In women, however, pelvic pain can very well be an indication that there might be a problem with one of the reproductive organs in the pelvic area (uterus, ovaries, fallopian tubes, cervix, and vagina).
Full Answer
What are the symptoms of pelvic pain?
What are the symptoms of pelvic pain? Type of pain Possible cause Localized pain May be due to an inflammation Cramping May be caused by spasm in a soft organ, ... Sudden onset of pain May be caused by a temporary deficiency ... Slowly-developing pain May be due to inflammation of the append ... 2 more rows ...
Where did the pelvic pain report come from?
It arose from Australia’s National Pain Summit of 2010, where the needs of girls and women with pain had not specifically been addressed. The Pelvic Pain Report investigated the human and fiscal burden of pelvic pain in Australia, interviewed widely, and formulated recommendations for improved services.
What is the most commonly used questionnaire for pelvic pain assessment?
It is the most commonly used questionnaire for pelvic pain assessment [ 109 ]. There is also a shrunk version of SF-36, SF-12, which only examines 12 questions. EuroQoL (EQ-5D) is another reliable questionnaire [ 110 ], not disease specific, which meets internationally accepted standards.
What causes chronic pelvic pain and how is it treated?
Chronic pelvic pain can result from more than one condition. Pelvic pain can arise from your digestive, reproductive or urinary system. Recently, doctors have recognized that some pelvic pain, particularly chronic pelvic pain, can also arise from muscles and connective tissue (ligaments) in the structures of the pelvic floor.
How do you describe pelvic pain?
Women describe pelvic pain in many ways. Pelvic pain can be steady, or it can come and go. It can be a sharp and stabbing pain felt in a specific spot, or a dull pain that is spread out. Some women have pain that occurs only during their menstrual periods.
How do you assess for pelvic pain?
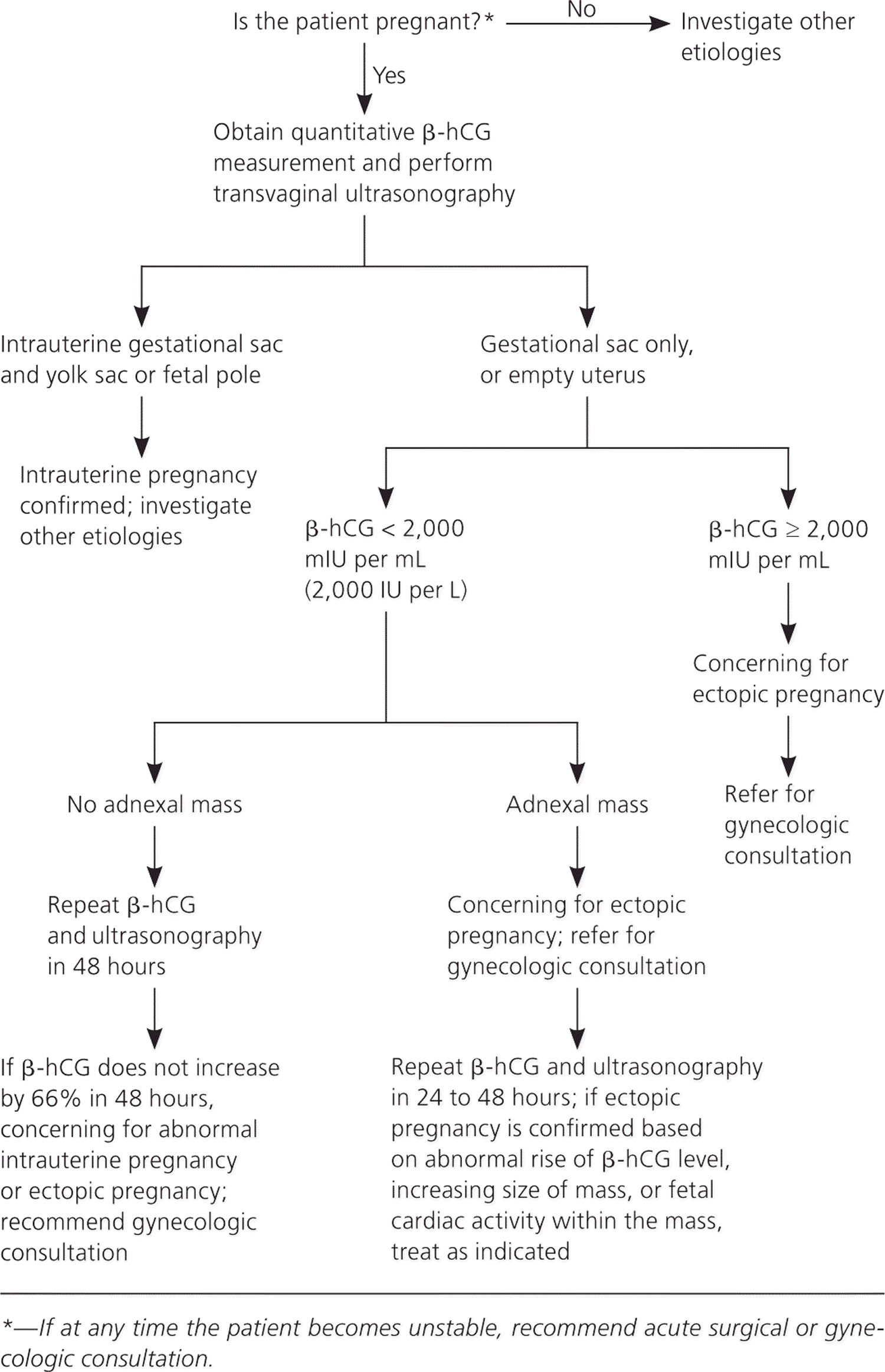
Transvaginal ultrasonography is the imaging modality of choice in the initial evaluation of pelvic pain. Cervical motion, uterine, or adnexal tenderness should place pelvic inflammatory disease high in the differential diagnosis of pelvic pain when no other etiology exists.
What causes pain on the pelvic area?
Pelvic pain can happen in both men and women and might stem from infections, abnormalities in internal organs, or pain from the pelvic bones. In women, pelvic pain might be related to the reproductive system. Treatment depends upon the cause.
Where do you experience pelvic pain?
Pelvic pain is pain in the lowest part of your abdomen and pelvis. Pelvic pain might refer to symptoms arising from the reproductive, urinary or digestive systems, or from muscles and ligaments in the pelvis.
When do you see pelvic pain?
Sudden and severe pelvic pain could be a medical emergency. Seek prompt medical attention. Be sure to get pelvic pain checked by your doctor if it's new, it disrupts your daily life, or it gets worse over time.
What can you do for pelvic pain?
Pain relievers. Over-the-counter pain remedies, such as aspirin, ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others), may provide partial relief from your pelvic pain. Sometimes a prescription pain reliever may be necessary.
Where is the pelvis?
The pelvis is the lower part of the torso. It's located between the abdomen and the legs. This area provides support for the intestines and also contains the bladder and reproductive organs.
Why do I have pelvic pain and lower back pain?
Fibroids are benign (non-cancerous) growths in the uterus. They can cause pain throughout the pelvis and lower back. Fibroids can also cause rectal or bladder pressure and the feeling of needing to go to the bathroom more often. PID is an infection that occurs in the female reproductive structures.
What is the pelvis?
The pelvis is the area of the body below the abdomen that is located between the hip bones and contains the bladder and rectum. In females, it also contains the vagina, cervix, uterus, fallopian tubes, and ovaries. In males, it also contains the prostate and seminal vesicles.
What is pelvic pain?
Symptoms of pelvic pain. The "pelvis" refers to your hip bones and all of the organs and structures contained within them. This includes your reproductive and urinary tracts; your large and small intestines; and the muscles, tendons, and ligaments inside your pelvis. Pain and other symptoms can arise from any of those locations, ...
Why does my pelvic area hurt?
If the abdominal organs are impaired due to normal processes or illness, this can result in pelvic pain. Infection and inflammation of the appendix. Constipation and gas. Intestinal contractions: The intestines may be contracting too strongly or too slowly, causing pain and discomfort either way.
Why do women have pelvic pain more often than men?
Women have pelvic pain more often than men. This is because the female pelvis is complex and designed for rapid change during pregnancy.
Why does my pelvis hurt during pregnancy?
During a pregnancy and in the weeks of recovery that follow: Even with a normal pregnancy, some pelvic pain and discomfort is common due to hormones which relax the ligaments for birth .
What is the term for the condition where the lining of the uterus grows on the outside of the o?
Endometriosis . Endometriosis is a condition where the tissue that normally forms the lining of the uterus – the endometrium – also begins growing on the outside of the ovaries and fallopian tubes. This out-of-place endometrium still thickens and bleeds each month, causing pain, scar tissue, and adhesions.
What causes discharge from the penis?
In men: Sexually transmitted diseases will cause a discharge from the penis as well as pelvic pain symptoms during urination and sexual activity.
What is the definition of pain?
The pain can fit almost any description: Dull, cramping, sharp, on-and-off, constant, mild, or severe
What is pelvic pain?
Pelvic pain is a common problem among women. Its nature and intensity may fluctuate, and its cause is often unclear. In some cases, no disease is evident. Pelvic pain can be categorized as either acute, meaning the pain is sudden and severe, or chronic, meaning the pain either comes and goes or is constant, lasting for a period of months or longer. Pelvic pain that lasts longer than 6 months and shows no improvement with treatment is known as chronic pelvic pain. Pelvic pain may originate in genital or other organs in and around the pelvis, or it may be psychological. This can make pain feel worse or actually cause a sensation of pain, when no physical problem is present.
What to do if pelvic pain is not a physical cause?
Specific treatment for pelvic pain will depend on the cause of the pain and will be discussed with you by your healthcare provider based on: If a physical cause can’t be found, your healthcare provider may refer you for counseling to help you better cope with chronic pain.
What is the condition called when you have pain in your pelvis?
Pelvic inflammatory disease (also called PID, an infection of the reproductive organs) Some of the conditions that can lead to chronic pelvic pain may include: Uterine fibroids (abnormal growths on or in the uterine wall) Scar tissue between the internal organs in the pelvic cavity.
Why does my pelvis hurt?
Some of the conditions that can lead to chronic pelvic pain may include: Uterine fibroids (abnormal growths on or in the uterine wall) Scar tissue between the internal organs in the pelvic cavity. Other causes may be related to problems in the digestive, urinary, or nervous systems.
What to do if physical pain is not found?
If a physical cause can’t be found, your healthcare provider may refer you for counseling to help you better cope with chronic pain. In other cases, healthcare providers may recommend a multidisciplinary treatment using a number of different approaches, including nutritional modifications, environmental changes, physical therapy, and pain management.
What are the different types of pelvic pain?
Always talk with your healthcare provider for a diagnosis. Type of pain. Possible cause. Localized pain. May be due to an inflammation. Cramping.
Where does pelvic pain come from?
Pelvic pain may originate in genital or other organs in and around the pelvis, or it may be psychological. This can make pain feel worse or actually cause a sensation of pain, when no physical problem is present.
Why does my pelvis hurt?
Pelvic pain might also be caused by irritation of nerves in the pelvis.
Can pelvic pain be caused by a digestive system?
Chronic pelvic pain can result from more than one condition. Pelvic pain can arise from your digestive, reproductive or urinary system. Recently, doctors have recognized that some pelvic pain, particularly chronic pelvic pain, ...
How long does pelvic pain last?
To qualify for this diagnosis, you need to have had pelvic pain for at least 3 months. Anywhere from 3 to 6 percent of men have chronic pelvic pain syndrome.
What is the pelvis?
The pelvis is the area below your belly button and above your thighs. Both men and women can get pain in this part of the body. Pelvic pain may signal a problem with your urinary tract, reproductive organs, or digestive tract. Some causes of pelvic pain — including menstrual cramps in women — are normal and nothing to worry about.
What is the German word for middle pain?
10. Mittelschmerz. Mittelschmerz is the German word for “middle pain.”. It’s pain in the lower belly and pelvis that some women get when they ovulate. Ovulation is the release of an egg from the fallopian tube that occurs halfway through your menstrual cycle — hence the word “middle.”.
What is the name of the inflammation of the bladder that causes pain and pressure in the pelvis and lower belly?
Cystitis is an inflammation of the bladder that’s usually caused by an infection of the urinary tract. It causes pain or pressure in your pelvis and lower belly.
What causes pain in the back of the kidney?
A kidney infection may develop if bacteria gets into your kidneys. This can also cause pain in your back, side, lower abdomen, and groin. Sometimes people with kidney stones also have a kidney infection. Other symptoms of a kidney stone or infection include: blood in your urine, which may be pink, red, or brown.
Why does my testicle hurt after a vasectomy?
This is called post-vasectomy pain syndrome. It can be caused by damage to structures in the testicle, or pressure on nerves in the area , among other factors. The pain can be constant, or come and go. Some men also have pain when they get an erection, have sex, or ejaculate.
Why does my kidney stone hurt?
Because the tubes are small and inflexible, they can’t stretch to move the stone through, and this causes pain.
What is pain in the pelvis?
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage [ 1 ]. Chronic Pelvic Pain (CPP) is defined by the European Association of Urology (EAU) as “chronic or persistent pain perceived in structures related to the pelvis of either men or women. It is often associated with negative cognitive, behavioural, sexual and emotional consequences as well as with symptoms suggestive of lower urinary tract, sexual, bowel, pelvic floor or gynaecological dysfunction. In the case of documented nociceptive pain that becomes chronic/persistent through time, pain must have been continuous or recurrent for at least 6 months. If non-acute and central sensitization pain mechanisms are well documented, then the pain may be regarded as chronic, irrespective of the time period” [ 2 ]. The American College of Obstetricians and Gynaecologists similarly defines CPP as “non-cyclic pain lasting for 6 or more months, that localizes to the anatomic pelvis, anterior abdominal wall at or below the umbilicus, the lumbosacral back, or the buttocks and is of sufficient severity to cause functional disability or lead to medical care” [ 3 ]. The EAU further defines Chronic Pelvic Pain Syndrome (CPPS) as “the occurrence of CPP when there is no proven infection or other obvious local pathology that may account for the pain. It is often associated with negative cognitive, behavioural, sexual or emotional consequences, as well as with symptoms suggestive of lower urinary tract, sexual, bowel or gynaecological dysfunction. CPPS is a subdivision of CPP. ] Pain perception in CPPS may be focused within a single organ, more than one pelvic organ and even associated with systemic symptoms such as Chronic Fatigue Syndrome (CFS), Fibromyalgia (FM) or Sjögren's Syndrome. When the pain is localized to a single organ, some specialists may wish to consider using an end organ term such as Bladder Pain Syndrome (BPS). The use of such a phrase with the terminology ‘syndrome' indicates that, although peripheral mechanisms may exist, CNS neuromodulation may be more important and systemic associations may occur. When the pain is localized to more than one organ site, the term CPPS should be used.” [ 2 ]. “End organ” terminology reflects the site in which pain presents, and therefore specific terms for the involved organ (such as Bladder Pain Syndrome and Prostate Pain Syndrome) are classified in EAU guidelines. In more detail, the guidelines distinguish Urological, Gynaecological, Gastrointestinal, and Musculoskeletal Pain Syndromes [ 2 ]. Urological Pain Syndromes include Bladder Pain Syndrome, which is often termed as “Interstitial Cystitis” by several authors, and Prostate Pain Syndrome, which is often termed “Chronic Prostatitis/Chronic Pelvic Pain Syndrome” instead by many authors according to the NIH Classification of Chronic Prostatitis [ 4 ]. Moreover, Scrotal Pain Syndrome, Testicular Pain Syndrome, Epididymal Pain Syndrome, Postvasectomy Scrotal Pain Syndrome, Penile Pain Syndrome, and Urethral Pain Syndrome are all classified as Urological Pain Syndromes. Again, in many articles authors refer to these syndromes as “Chronic Orchialgia” or “Chronic Scrotal Syndrome” [ 5, 6 ]. Gynaecological Pain Syndromes include Vulvar Pain Syndrome (also termed “Vulvodynia”), Vestibular Pain Syndrome, Clitoral Pain Syndrome, Dysmenorrhea, and Endometriosis-Associated Pain Syndrome. Irritable Bowel Syndrome and Pelvic Floor Muscle Pain Syndrome are the most widespread Gastrointestinal and Musculoskeletal Pain Syndromes, respectively.
What are pain scales and questionnaires?
Besides anamnestic interview and clinical examinations, pain scales and questionnaires are useful and reliable tools to assess pain intensity, and moreover some questionnaires also allow the distinction between nociceptive and neuropathic pain in patients presenting with more complex painful syndromes. Notably, several scales and questionnaires have been developed over years and the choice for the proper one depends on clinical settings; patient's gender, age, and education; and physician's personal experience. We also will review some QoL and psychological assessment questionnaires, as CPP and CPPS often have a detrimental impact on patients' daily activity and represent a considerable burden on emotional and psychological processing. Moreover, as discussed above, patients presenting with associated psychological features besides CPP/CPPS often have poorer pain control and worse clinical course than patients without these features. Recently, some criteria for the reevaluation of scales and questionnaires in chronic pain patients have been proposed [ 65 ]. The proposed criteria are content validity (scales should really measure the most important symptoms associated with pathology), test–retest reliability (a patient should give the same answer concerning the same type of pain in case of repeated administration of the same test), and responsiveness (scales results and patient conditions should change in the same way). Below we will review the most widespread scales and questionnaires that might be useful for CPP/CPPS assessment and evaluation.
What is a PUF score?
Lowell Parsons for the study and diagnosis of Interstitial Cystitis (IC/PBS: Interstitial Cystitis/Painful Bladder Syndrome). It examines both a symptom score (which measures how often a patient experiences problems) and a bother score (how much symptoms bother the patient); combination of both scores is the total PUF score. Score range is between 0 and 35 and a score equal to or greater than 12 is suggestive for the disease in question even if further diagnostic urological, gynaecological, or urogynaecological evaluations are needed. It was, in fact, demonstrated that high scores may be compatible with different diagnoses such as urinary tract infections or overactive bladder syndrome [ 84 ]. To date, however, the PUF questionnaire is mainly used in the followup of patients already being treated for urological disorders. Several other scales and questionnaires have been developed in order to assess and evaluate Interstitial Cystitis/Painful Bladder Syndrome patients. One of the most widespread is the O'Leary-Sant Interstitial Cystitis Symptom Index and Problem Index [ 85] which consist in two self-administrable indices that measure pain and urinary symptoms and their impact (the problem index) on overall QoL and daily activities. Psychometric performance of both the indices was reported to be good, with the symptom index being able to distinguish between patients' and controls' characteristics [ 86 ]. The indices also showed good responsiveness [ 87 ]. Both indices should be useful in the evaluation and management of patients with IC/PBS; accordingly, they were able to predict treatment outcomes in clinical trials [ 88 ]. Similarly, the Bladder Pain/Interstitial Cystitis Symptom score, developed by Humphrey and colleagues [ 89 ], was validated in order to properly evaluate IC/PBS patients and correctly allocate them in clinical trials. The examined items are focused on bladder and urinary issues: bladder pain, persistent urge to urinate, and high urinary frequency. The University of Wisconsin Interstitial Cystitis Scale [ 90] is a symptom scale originally developed for women with Interstitial Cystitis. The scale contains 7 questions directly related to bladder symptoms (bladder pain, bladder discomfort, burning bladder sensation, nycturia, sleep difficulties due to nycturia, polyuria, and urinary urgency) in the last 24 hours. The Pelvic Pain Assessment Form is another gender-specific scale designed for women and developed by the International Pelvic Pain Society [ 91] and is composed of two parts: the first should be filled out by the patient and the last by the physician. The form allows complete registration of information about the patient's pain (causes, duration of pain, Visual Analogue Scale score, pain medications, and pain distribution maps), patient's past and recent clinical history (including surgical, obstetrical, family, medical, menstrual, and gastrointestinal history; eating and health habits; genitourinary symptoms; coping mechanisms; sexual and physical abuse history), and eventual former evaluations performed by other physicians. The form also includes a short form of Mc Gill Pain Questionnaire and a section dedicated to a pelvic varicosity pain syndrome specific questionnaire. The physician will also provide a physical examination, a gynaecological examination, and lastly a diagnostic and therapeutic plan. Notably, this form does not have a diagnostic value. The National Institute of Health Chronic Prostatitis Symptom Index (NIH-CPSI) Questionnaire [ 92] is a 13-item index developed to assess symptoms and quality of life in men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) [ 93 ]. It has demonstrated good reliability, validity, and responsiveness to change [ 94 ], and it has been used as the primary outcome variable in multiple large-scale studies of CP/CPPS treatments. It has also been translated into multiple languages for international use [ 95, 96 ]. It is indicated for patients complaining of CPP, probably caused by Chronic Prostatitis or CPPS. Pain, voiding symptoms, and any interference of the symptoms with the quality of life are evaluated. The Genitourinary Pain Index (GUPI) is a more recent symptom index developed from NIH-CPSI [ 97] in order to assess genitourinary pain in both men and women. The GUPI included items dealing with urinary symptoms, localization and intensity of pain symptoms, and overall quality of life. Total scores range from 0 to 45; individual scores for the domains of pain, urinary symptoms, and quality of life impact can also be derived. Similarly, another questionnaire, the CPPQ-Mohedo, has been developed by Díaz Mohedo and colleagues [ 98 ]. It is also derived from NIH-CPSI score for male patients, with the purpose of editing a feasible questionnaire for both male and female patients with the same analysed items.
What is a monodimensional pain scale?
Monodimensional pain scales are a simple yet useful tool for a “raw” first assessment of pain. As they merely consist of a value of patient's experienced pain, they are not suitable to reveal the quality of the painful experience or to differentiate nociceptive from neuropathic features of pain. Nevertheless, they are still useful for both acute [ 15] and chronic pain evaluation, as they are quickly administrable in inpatient and/or outpatient service. The most widespread monodimensional pain scales are the Visual Analogical Scale (VAS) and the Numerical Rating Scale (NRS), which assess pain with an increasing number from 0 (no pain) to 10 (the worst pain imaginable). Another commonly used scale is the Verbal Numerical Rating Scale (VNRS), in which the patient is asked to match pain with an adjective (and a corresponding number). Since they consist in numeric values, monodimensional pain scales are still often used as an outcome measure for clinical trials [ 66 ], both for measuring treatment effectiveness [ 67] and for validating new developed diagnostic tools [ 68 ]. All the three scales are comparable in pain evaluation, although different authors may prefer one to the others [ 69 – 72 ]. Wong–Baker Faces Pain Rating Scale is instead a scale which is suitable for speechless patients, as they are asked to indicate a drawn face that is representative of the pain; the drawings are then matched again with corresponding numbers. Lastly, a pain intensity score may also be obtained with a behavioural index, which is the esteem of pain evinced from patient's behaviour. A specific behavioural index, which also included psychological and neurovegetative signs, has been designed for gynaecologic pain evaluation in emergency settings [ 15 ].
What is MRI for chronic pain?
In recent years, Magnetic Resonance Imaging (MRI) and functional MRI (fMRI) have been suggested as tools to diagnose and objectivate chronic pain, as characteristic abnormalities have been detected in several chronic pain syndromes [ 138 – 141 ].
Is pelvic pain a clinical condition?
While acute pelvic pain is considered as the fifth vital sign [ 14, 15] in the same way as other acute pain conditions, C PP is generally considered to be a description of a clinical condition [ 16] rather than a diagnosis. Nevertheless, CPP has a significant impact on women of reproductive and nonreproductive age, with a considerable burden on overall quality of life (QoL) and on psychological, functional, and behavioural status. CPP prevalence varies in a wide range, according to different cohort sampling, from 5,6% to 30,9% [ 17 – 20 ]. Notably, the reported prevalence varies according to the country in which the sample is enrolled: in a recent epidemiology-based study prevalence ranged from 6,4% in Mexico to 25,4% in New Zealand [ 21 ]. This wide range of reported prevalence may reflect sociocultural differences in the investigated countries with a possible resilience to the admission of urogynaecological troubles. The prevalence of CPP/CPPS in men is also variable in different studies, although lower than their prevalence in women; the reported prevalence of CPP symptoms in men ranges between 2% and 17% [ 19, 22 – 24 ]. Prostate Pain Syndrome/Chronic Prostatitis and Scrotal Pain/Orchialgia are the most common syndromes male patients complain of. Prostate Pain Syndrome/Chronic Prostatitis is a high prevalent syndrome (prevalence ranges between 4,5 and 9% in different cohorts, although the effective prevalence is likely underestimated) [ 25 ], which is often accompanied by psychosocial burdening symptoms, Voiding Cycle Lower Urinary Trait Symptoms and Bladder Pain [ 26 ], Postejaculatory Pain [ 27 ], Erectile Dysfunction [ 28 ], and Pelvic Floor Muscle Pathology [ 29 ]. In a recent survey regarding young Canadian and African males with age ranging from 16 to 19 years [ 30, 31 ], Chronic Prostatitis-like symptoms were assessed, and also sexual, psychological, and overall QoL features were investigated; 8–13,3% of mild symptoms and 3–5,4% of moderate to severe symptoms were identified in the two cohorts, respectively. In both the cohorts, pain, urinary, and psychological symptoms were predictive of a worsened QoL.
When will facing pelvic pain be published?
Published in 2021, Facing Pelvic Pain is a new book providing step-by-step ways to best improve from this condition, which can affect people of any age, gender or pre-existing physical condition.
What is the goal of facing pelvic pain?
The goal is to find causes, to prevent further pain as soon as possible, and to sustain good health once recovered.

Popular Posts:
- 1. insight vision patient portal
- 2. port orange imaging patient portal
- 3. elyria medical center patient login
- 4. moberly diagnostics patient portal
- 5. ecw patient portal jefferson health
- 6. baylor patient health portal
- 7. emerald patient portal
- 8. patient portal mcr
- 9. christus good shepherd patient portal deactivate
- 10. my patient reach portal