Patient Engagement in Reporting Medication Events …
14 hours ago The blood sugar after conducting tests was at 5.1, which is stable. Based on the patient’s medical history, the patient has experienced hypertension, TIA, CHF and Atrial fibrillation. Monitoring for the patients ECG was done every 48 hours. The weight of the patient was done weekly, and in case, it increased, the doctor was to be notified. >> Go To The Portal
Why do hospitals keep patient medical report?
They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report. It can be a proof if there is any doctor withholding treatments.
Who has the access to the patient medical report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must.
How can you use @healthcare report data to improve healthcare?
Healthcare report data can assist hospitals in offering information on individual patient basis. By doing so, a healthcare institution can give their patients tailored advice on how they can maintain a healthy lifestyle based on their medical data and biometric vitals.
What is a patient care report?
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.
How can you improve patient adherence to medication?
Nine Tips for Improving Medication AdherenceEducate patients about what to expect. ... Nurture relationships with patients. ... Team up with prescribers. ... Engage the staff. ... Learn about and use available technologies. ... Help patients customize their support tools. ... Schedule appointments. ... Synchronize medications.More items...•
Which strategies are helpful in preventing medication errors in nursing practice?
10 Strategies for Preventing Medication ErrorsEnsure the five rights of medication administration. ... Follow proper medication reconciliation procedures. ... Double check—or even triple check—procedures. ... Have the physician (or another nurse) read it back. ... Consider using a name alert.More items...•
How do you review a patient with a medication?
5 Steps to Prepare for a Medication ReviewList all medications you're taking, along with the intended purpose of each medication. ... Know the purpose of a prescribed medication and symptom and take note of when the symptom was last checked on. ... Know which of your medications are on the Beer's list.More items...
What is medication nonadherence?
Medication nonadherence—when patients don't take their medications as prescribed—is unfortunately fairly common, especially among patients with chronic disease. When this is the case, it is important for physicians and other health professionals to understand why patients don't take their medications.
What are the advantages of documenting medication errors?
Medication errors have significant implications on patient safety. Error detection through an active management and effective reporting system discloses medication errors and encourages safe practices.
How patients can reduce medication errors?
One way to prevent human error is by involving a second human-a pharmacist or technician (as permitted by state law)-in the dispensing process. “If I'm the one taking the prescription and entering it, then I'm not pulling the drug and counting it, because I know I have to final check it,” Leikach said.
Why is reviewing medication important?
It is important to review medication regularly to make sure it is appropriate for you. Each individual varies biologically which means different medications suit different people better. By having medication reviews we can help make sure you are benefiting well from your medicine.
What happens at a medication review?
The review will involve the doctor/pharmacist/nurse gathering information from you and from your medical record. This information will be used to check that you are taking the most appropriate medicines. You will also be able to ask any questions or raise any concerns you have about your medicines.
What are the 4 levels in a medication review?
In 'Room for Review' in 2002 they suggested four levels of medicine review – level 0 which is an ad-hoc opportunistic review; level 1 a prescription review which is a technical review of a patients list of medicines; level 2 is a treatment review which is a review of medicines with the patients full notes and level 3 ...
Why is medication nonadherence a problem?
Not taking the right dose—or abandoning treatment altogether—can exacerbate a patient's health condition, increase the risk of disease progression, and lead to prolonged hospitalization.
How common is medication nonadherence?
Medication nonadherence is widely recognized as a common and costly problem. Approximately 30% to 50% of US adults are not adherent to long-term medications leading to an estimated $100 billion in preventable costs annually.
Why are patients non compliant with medications?
The most common reasons for patient non-compliance to medications are intentional and include: high drug costs, fear of adverse events, being prescribed multiple medications, and experiencing either instant relief or medication ineffectiveness leading to self-discontinuation of medications.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
What is a patient report experience?
Patient report experiences through the use of PREMs, such as satisfaction scales, providing insight into the patients’ experience with their care or a health service. There is increasing international attention regarding the use of PREMS as a quality indicator of patient care and safety.
What is indicator in healthcare?
Indicators are a type of metric that identifies issues requiring further investigation (eg, increase in number of falls) (NHS Institute for Innovation and Improvement/Public Health Observatories, 2007) and reflects how effectively an organization is performing on a set of metrics.
Why are proms important?
The use of PROMs continues to expand beyond clinical research in recognition of its potential to transform health care, as well as improve quality and safety by placing the patients at the center of decision-making.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
Why is it so difficult to link patient-reported outcomes to particular treatments?
Another major reason is that, generally, clinicians are not able to bill for time spent fielding outcomes surveys or interpreting such data. It's also difficult to link patient-reported outcomes to particular treatments since many factors—including patients' compliance and social factors—influence outcomes.
What is the Office of the National Coordinator for Health Information Technology?
The Department of Health and Human Services' Office of the National Coordinator for Health Information Technology also plans to incorporate PROMs into meaningful use standards, which is likely to prompt more widespread use.
What is a prom in clinical practice?
Use of PROMS in Clinical Practice. In the U.S., PROMs are in the early stages of development for use in clinical practice, as opposed to research. They have been most widely used to monitor conditions that rely on patients' reports (rather than diagnostic tests), such as depression or certain gastrointestinal disorders.
What is the goal of joint replacement?
The goals of the endeavor are to improve patient safety and clinical outcomes by providing information on the comparative effectiveness of different joint replacement techniques and procedures, and to inform patient decision-making.
Why do I lose my prescription form?
Losing a prescription form or a vial of medications may result from the occasional lapses that all patients may have. If this occurs only once it may not have significant medical implications, and the prescriber may choose to replace it without much concern.
Can a patient report a prescription that has been lost?
Advice: It is not unusual for a patient to report to their prescribing clinician that they have discovered that their prescription pain medication (or the written prescription) has been either lost or stolen, leading them to request a new prescription.
What are the benefits of healthcare reporting?
Here are some notable examples and benefits of using business intelligence in healthcare: 1. Preventative management.
What is patient satisfaction?
Patient satisfaction: A top priority for any healthcare organization, the patient satisfaction KPI provides a deeper look at overall satisfaction levels based on wait time, nutrition, care and processes. A mix of patient feedback and valuable satisfaction-based metrics will help you make all-important changes to your organization, helping you to improve satisfaction levels on a consistent basis.
What is hospital analytics?
Hospital analytics and reports give organizations the power to amalgamate clinical, financial, and operational data that determines the efficiency of their various processes, as well as the state of their patients, and the productivity of their healthcare programs.
What is a hospital performance dashboard?
By leveraging the power of clear-cut targets and pre-defined outcomes, the hospital performance dashboard offers the kind of visualizations that can significantly enhance all key areas of your healthcare institution.
Why is healthcare important?
Healthcare is one of the world’s most essential sectors. As a result of increasing demand in certain branches of healthcare, driving down unnecessary expenditure while en hancing overall productivity is vital. Healthcare institutions need to run on maximum efficiency across the board—in some cases, it’s literally a matter of life or death.
What is treatment cost?
Treatment costs: An economic management-based KPI that helps healthcare providers calculate the amount of money an average patient costs. ER waiting time: The ER waiting time KPI measures the length of time a patient arrives in the ER right through to the moment they see a physician.
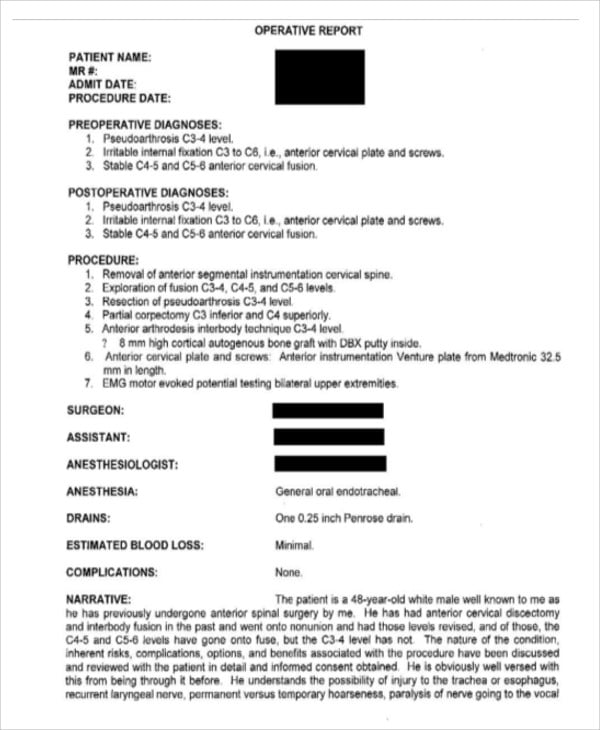
What is a Patient Medical Report?
A patient medical report is a comprehensive document that contains the medical history and the details of a patient when they are in the hospital. It can also be given as a person consults a doctor or a health care provider. It is a proof of the treatment that a patient gets and of the condition that the patient has.
What You Should Include in a Patient Medical Report
A patient medical report has some important elements that you should not forget. Include all these things and you can learn how to write a patient medical report.
Importance of a Patient Medical Report
The reason why a patient medical report is always given is because it is important. Here, you can know some of the importance of a patient medical report:
How to Write a Good Patient Medical Report
A doctor is a doctor. They are not writers. They can be caught in a difficulty on how to write a patient medical report. If this is the case, turn to this article and use these steps in making a patient medical report.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physicians, nurses, and doctors of medicine. It also includes the psychiatrists, pharmacists, midwives and other employees in the allied health.
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report.
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patient is under your care. Thus, it can be used in court as an essential proof. So, keep a patient medical report because you may need it in the future.
What is a PRO in medicine?
This chapter reviews the definition, development, and utilization of PROs for both research and clinical purposes, including developmental considerations for administration of PROs with children. Health-related quality of life measures (HRQoL) are one type of PRO, and several condition-specific PROs have been developed for a variety of pediatric respiratory diseases, including vocal cord dysfunction, asthma, cystic fibrosis, sleep-related breathing disorders, and primary ciliary dyskinesia. A substantial body of literature has demonstrated that condition-specific, rather than generic measures, are more sensitive to change and better reflect the patient's symptoms and functioning. This chapter reviews the currently available PROs for pediatric respiratory conditions, including a description of the instrument, the domains of functioning it measures, the appropriate developmental age for administration, and the psychometric properties of the instrument, including its reliability and validity. Use of PROs is becoming standard practice for both randomized clinical trials and clinical care. The current shift in medicine toward patient-centered care is consistent with development and use of PROs. These measures provide unique information about patient symptoms, level of daily functioning, and systematic response to treatment. These measures have also been shown to facilitate patient-provider communication and shared decision-making. Integration of PROs into clinical care is a critical step in promoting patient-centered, quality health care practice.
What is a PRO in clinical practice?
A patient-reported outcome (PRO) refers to an assessment of a patient’s health condition that comes directly from the individual (see Chapter 6 for further discussion). PROs are increasingly recognized as an important aspect of clinical practice and clinical trials.
Why are proms important?
PROMs can be used for different purposes: as feedback for the patient self, for the clinician to identify which patient experiences improved or deteriorated health outcome over time, in clinical research, and as an indicator in healthcare systems for assessing the performance of hospitals and clinics.
Is condition specific measure more actionable than generic measure?
Although well-developed condition-specific or individualised measures are likely to have enhanced clinical relevance than generic measures, providing information that is more actionable, appropriate education and training in the application and interpretation of PROMs is required.