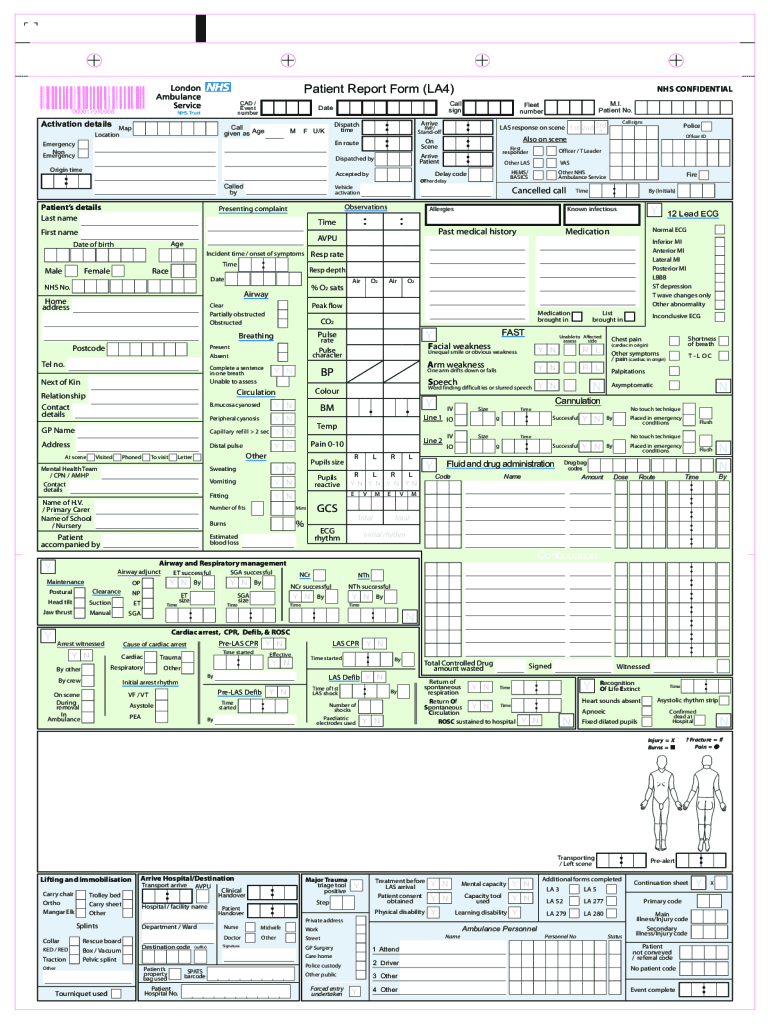
FREE 14+ Patient Report Forms in PDF | MS Word
18 hours ago · A patient incident report is a form that provides a detailed account of an incident that takes place in a healthcare setting, such as a hospital. Generally, a nurse will complete this report, which might outline the events leading up to a fall or a different kind of threat to a patient’s safety. >> Go To The Portal
What is a patient report form?
Report Forms FREE 14+ Patient Report Forms in PDF | MS Word Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results).
What is a nursing report template?
A nursing report focuses on providing accurate details of nursing by developing conducted research understood to the complete level of practicing nurses, educators, and interested members of the public. The sample report templates act as a huge help when it comes to constructing a precise nursing report.
Do nurses use report sheets?
Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them. Nurses who use them tend to keep them folded in their scrub pocket or on their clip board for easy access. Always make sure to get a good report on your patients before starting a new shift.
What is the first section of a nursing report?
General Information – The General Information section is the first section to be present in the Nursing Report. This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient. Patient Report – Next on the report, is the Patient Report section.

How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What is a report form in nursing?
Patient Progress Report A progress report is a written document that is vital in health care settings because this is where the health care practitioner will base their next plan of treatment. A good health progress report follows the ADPIE (Assessment, Diagnosis, Planning, Intervention, Evaluation) format.
How do you organize a nursing report sheet?
0:1210:04Nurse Brain Sheet | ORGANIZE YOUR NURSING SHIFT | Nursing ReportYouTubeStart of suggested clipEnd of suggested clipOrganization tips for you to be successful during your nursing shift the main one being a reportMoreOrganization tips for you to be successful during your nursing shift the main one being a report sheet and this is what people call their nurse brains.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What are 4 components of correct nursing documentation?
For documentation to support the delivery of safe, high-quality care, it should: Be clear, legible, concise, contemporaneous, progressive and accurate.
What should be included in a patient incident report?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
How many types of nursing reports are there?
There are different types of nursing reports described in the literature, but the four main types are: a written report, a tape-recorded report, a verbal face-to-face report conducted in a private setting, and face-to-face bedside handoff.
How do I create a report sheet?
0:5111:10How to Organize a Nursing Report Sheet - YouTubeYouTubeStart of suggested clipEnd of suggested clipName I always do their last name first followed by their first name since that's how all the medicalMoreName I always do their last name first followed by their first name since that's how all the medical documents always have it and I usually capitalize.
How do you give a good report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What is SBAR report?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
What should a nursing handoff report include?
Nurses complete their handoff report with evaluations of the patient's response to nursing and medical interventions, the effectiveness of the patient-care plan, and the goals and outcomes for the patient. This category also includes evaluation of the patient's response to care, such as progress toward goals.
How do you give a good report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What should a handover nurse include?
What goes in to a handover?Past: historical info. The patient's diagnosis, anything the team needs to know about them and their treatment plan. ... Present: current presentation. How the patient has been this shift and any changes to their treatment plan. ... Future: what is still to be done.
How do I write a good bedside report?
5 Tips for an Effective End-of-Shift ReportGive a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
Why is it important to have an ICU nurse report?
Due to this, it is very important that nurses are able to gather the required information. To help with this situation, ICU Nursing Reports were brought into action. ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
What is a nursing report sheet?
The report sheets enable the nurses to record clear information regarding details including the diagnosis, history, allergies, consults, vital signs, lab results, and other such health-related data. Due to their excellent recording system, nursing report sheets are used by physicians, doctors, nurses and other healthcare staff all over the world. ...
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
What is the purpose of the General Information section in a nursing report?
This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient.
What is flow sheet in nursing?
A6. In simple terms, a flow sheet is a single or dual-page form, tasked with the job of gathering all important aspects of a patient’s condition. Similar to the other nursing reports, the flow sheet is tasked with gathering patient information.
What is a lab report?
Labs – Labs refers to the various patient reports which have been derived from the numerous tests conducted on the patient. The constituents of this section are Labs, Needed Labs, and Future Procedures. Completion – Completion is the final section of a nursing report template.
What is HIPAA release form?
This law was primarily passed due to proliferation of data breaches concerning health information.This HIPAA Release Form PDF Template is a standard release authorization form for disclosure of health information for healthcare and health insurance providers which the subject or person consents on disclosing his health information to a certain healthcare organization. This HIPAA Release Form PDF Template is easy to modify and flexible to use.
Why use a medical history record PDF?
Medical History Record PDF template is mostly used in order to provide significant information about the health history, care requirements, and risk factors of the patient to doctors. It is for collecting data from the patients.
What is a first aid incident report?
The First-Aid Incident Report template contains injured person's personal details and contact details, the details and visible symptoms of injury, the Glasgow Coma Scale which is a neurological scale that expects to give a dependable and target method for chronicle the condition of an individual's awareness and brief information of treatment. Also, it contains the profile of the first-aider and signature of the person who prepares the report. Plus, JotForm is HIPAA-compliant and that is gigantic in addition to for anybody in the medicinal services industry.
Why is HIPAA compliance important?
That’s why the HIPAA compliance act was put in place – To ensure the privacy of the patients’ medical records.
What is client progress report?
Client Progress Report for Psychotherapy PDF template provides the essential information that should contain in a clinical psychotherapy report such as the name of the patient, the type of session made with the patient, the date of the session, a comprehensive assessment, and treatment goals and objective for the patient/client.
What is release of information?
A Release of Information is a document signed by the authorizing person owner, allowing the recipient or holder of the information to disclose or use the information through the consent of the owner.
What is a dental health record template?
The Dental Health Record Template is easy for patients to fill out and designed to get the doctor the most important information. Patients can fill out their information on a computer or tablet using our Dental Health Record Template.
What is a nursing report sheet?
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report.
What is a nursing note?
Nursing notes to remind yourself of things you need to do for the patient or chart on. Notes to yourself on things you want to remind the next shift. Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them.
Why do nurses use report sheets?
Why Do Nurses Use Nursing Report Sheets? Nurse report sheets are very handy because they contain tidbits of vital information concerning your patient’s diagnosis, history, allergies, attending doctor,consults, things that need to be done on your shift, medication times, vital signs, lab results etc. The report sheet has other usage as well.
Why is it important to have a 6 to 7 patient load?
When you have a 6 to 7 patient load, patient diagnosis and histories can run together and you may get them confused. Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do.
Can you print a report sheet for nurses?
You can share them with other nurses as well. Simply click the picture of the report sheet you like and after you download it you can print them. Tip: for less report sheets to carry around set your printer settings so you can print on the back side.
Why is it important to have a nursing report?
It is important for good clinical communication to have a concise nursing report. A great report provides an accurate reflection of nursing assessments to support the medical team to provide great care. Objective. To provide a structured and standardized approach regarding nursing report and documentation.
What is included in a clinical report?
Any relevant clinical information is also included such as a change in condition, adverse findings or events, patient outcomes, clinical investigations, and other relevant aspects. Don’t forget to close the report with companion documents. These are patient identification, nursing assessment, and legislative compliance.
What is a nursing report?
A nursing report focuses on providing accurate details of nursing by developing conducted research understood to the complete level of practicing nurses, educators, and interested members of the public. The sample report templates act as a huge help when it comes to constructing a precise nursing report. You may also check here Report Examples
How to make a good decision in a report?
Support your decision with statistics and facts. As much as possible, keep your report short and concise. The shorter the better. You need to summarize your message and write it down on the first page. Make sure to keep the body of your report as short as possible.
You Need a Nursing Brain Sheet That Works for YOU
For the longest time I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . put at closer inspection you start to see all the details and information you have available with it. From lab values, to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experience nurse.
6. Just the Boxes
I’ll be honest . . . after a couple years of being a nurse my “brainsheet” has evolved into more of a few freehand drawing on a sheet of paper. If that sounds like you, this is probably the one for you. With little more than a few suggestions . . . this is a pretty basic organizer for nurses.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.