Osteoporosis: Diagnosis, Treatment, and Steps to Take
23 hours ago The Osteoporosis Report is an excellent source of timely news and valuable information about how to help prevent osteoporosis and maintain strong, healthy bones. On a quarterly basis, patients, caregivers and anyone interested in good bone health can learn about BHOF’s latest projects/programs, consumer-friendly tips on diet, exercise/safe movement, recent advocacy … >> Go To The Portal
Common tests & procedures
Who is at risk of developing osteoporosis?
- Gender. Osteoporosis can happen in both males and females, but women are more likely to develop it than men.
- Age. Women over 50 years old, postmenopausal women, and men over 70 years old are at greatest risk of developing osteoporosis.
- Body size. ...
- Race. ...
- Family history. ...
- Hormonal changes. ...
- Diet. ...
- Medical conditions. ...
- Pregnancy and lactation. ...
- Medications. ...
What are your chances of developing osteoporosis?
Research trends in osteoporosis in Asian countries and regions in the last 20 years
- Abstract. Asian countries have made great progress in the osteoporosis research over the past 20 years. ...
- Introduction. Osteoporosis is a globally huge and growing public health problem [ 1 ]. ...
- Materials and methods. ...
- Results. ...
- Discussion. ...
- Conclusion. ...
- Abbreviations. ...
- References. ...
- Funding. ...
- Author information. ...
What country has the most osteoporosis?
- Sex hormones - Reduced estrogen levels due to menopause or absent menses can cause osteoporosis in women. ...
- Anorexia nervosa (eating disorder) - can cause osteoporosis.
- Calcium and vitamin D intake - A diet deficient in calcium and vitamin D increase risk of osteoporosis
- Medications - Some medicines such as steroids increase osteoporosis risk
What are facts about osteoporosis?
Some risk factors for osteoporosis are out of your control, including:
- Your sex. Women are much more likely to develop osteoporosis than are men.
- Age. The older you get, the greater your risk of osteoporosis.
- Race. You're at greatest risk of osteoporosis if you're white or of Asian descent.
- Family history. ...
- Body frame size. ...
What are the risk factors/ causes of developing osteoporosis?

How do you assess a patient with osteoporosis?
To diagnose osteoporosis and assess your risk of fracture and determine your need for treatment, your doctor will most likely order a bone density scan. This exam is used to measure bone mineral density (BMD). It is most commonly performed using dual-energy x-ray absorptiometry (DXA or DEXA) or bone densitometry.
What is the common presentation of a patient with osteoporosis?
But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include: Back pain, caused by a fractured or collapsed vertebra. Loss of height over time. A stooped posture.
What is the hallmark appearance of a patient with osteoporosis?
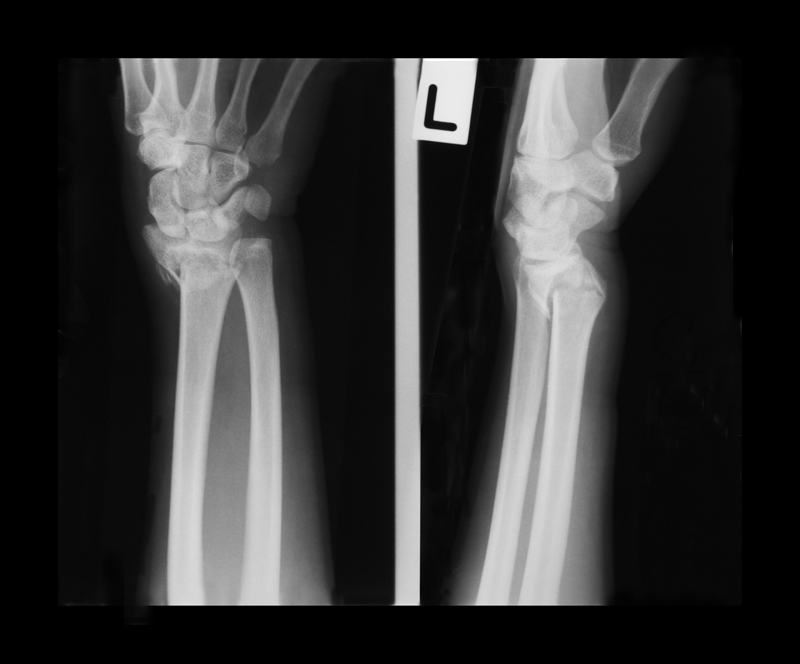
Osteoporosis is defined as a reduction in bone mass and disruption of bone architecture, resulting in reduced bone strength and increase of bone fractures. Fragility fractures are the hallmark of osteoporosis and are particularly common in the spine, hip and forearm but may also affect other sites (1).
What should I ask a patient with osteoporosis?
10 Osteoporosis Questions to Ask Your DoctorAre there ways to keep osteoporosis from worsening?Can medications taken for other illnesses cause bone loss?How can I prevent fractures?How frequently should I have a bone density test?More items...•
What is description of osteoporosis?
(OS-tee-oh-puh-ROH-sis) A condition in which there is a decrease in the amount and thickness of bone tissue. This causes the bones to become weak and break more easily. Osteoporosis may be caused by older age, hormone changes, taking certain medicines, and not eating enough foods with calcium and vitamin D.
What is the first indicator of osteoporosis?
Bones that easily fracture: Bone fractures and breaks are often the earliest signs that people experience of osteoporosis. Since your bones have less strength, you are more likely to experience serious bone injuries if you suffer from a fall, or experience other bone trauma.
What are the three stages of osteoporosis?
The stages of OsteoporosisOsteoblasts vs Osteoclasts. Active Osteoblasts. ... Peak bone density and the first stages of osteopenia and osteoporosis. ... The second stage of osteopenia and osteoporosis. ... The third stage of osteopenia and osteoporosis. ... The fourth stage of osteopenia and osteoporosis.
What is a good T-score?
As shown in the table below, a T-score between +1 and −1 is considered normal or healthy. A T-score between −1 and −2.5 indicates that you have low bone mass, although not low enough to be diagnosed with osteoporosis. A T-score of −2.5 or lower indicates that you have osteoporosis.
What types of measurement can you make in clinic to assess her for osteoporosis?
Some of these tests include:Blood calcium levels.24-hour urine calcium measurement.Thyroid function tests.Parathyroid hormone levels.Testosterone levels in men.25-hydroxyvitamin D test to determine whether the body has enough vitamin D.Biochemical marker tests, such as NTX and CTX.
What are risk factors for developing osteoporosis?
Bone structure and body weight. Petite and thin women have a greater chance of developing osteoporosis. One reason is that they have less bone to lose than women with more body weight and larger frames. Similarly, small-boned, thin men are at greater risk than men with larger frames and more body weight.
What is the best way to treat osteoporosis?
Bisphosphonates are usually the first choice for osteoporosis treatment. These include: Alendronate (Fosamax), a weekly pill. Risedronate (Actonel), a weekly or monthly pill.
How likely is it to develop osteoporosis?
How likely you are to develop osteoporosis depends partly on how much bone mass you attained in your youth. Peak bone mass is somewhat inherited and varies also by ethnic group. The higher your peak bone mass, the more bone you have "in the bank" and the less likely you are to develop osteoporosis as you age.
What are the factors that increase the risk of osteoporosis?
A number of factors can increase the likelihood that you'll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
What causes a fracture in the hip?
Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.
How do you know if you have bone loss?
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include: Back pain, caused by a fractured or collapsed vertebra. Loss of height over time. A stooped posture.
How to reduce risk of falling?
Balance exercises such as tai chi can reduce your risk of falling especially as you get older. Swimming, cycling and exercising on machines such as elliptical trainers can provide a good cardiovascular workout, but they don't improve bone health. By Mayo Clinic Staff. Request an Appointment at Mayo Clinic.
What are some examples of osteoporosis?
Examples include: Sex hormones. Lowered sex hormone levels tend to weaken bone. The reduction of estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Men have a gradual reduction in testosterone levels as they age.
How many alcoholic drinks a day can cause osteoporosis?
Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
What is the nursing diagnosis of osteoporosis?
Some nursing diagnoses which might be appropriate for patients with a medical diagnosis of osteoporosis include impaired mobility if a limited range of motion is present, deficient knowledge, imbalanced nutrition, the risk for falls, the risk for injury if substantial bone loss is presently increasing the risk of fractures, and acute pain if fractures occur due to bone loss.
How to treat osteoporosis?
A healthy diet and weight-bearing exercise are important in the prevention and treatment of osteoporosis. Medical management of osteoporosis includes prescribed medication for the prevention or treatment of osteoporosis. Bisphosphonates are a major class of medications used to prevent or treat osteoporosis; alendronate and risedronate are examples. Monoclonal antibody medications are prescribed to increase bone mineral density. [4][5] Hormone-related therapy is another medication therapy for osteoporosis. One example is calcitonin traditionally prescribed to post-menopausal patients with osteoporosis; newer research is exploring the outcomes of the various newer medication therapies among post-menopausal patients.[6] Additionally, new therapies are emerging, and prescribing medications to maximize bone preservation is key. [2][7]
What is osteoporosis characterized by?
Introduction. Osteoporosis is a chronic condition characterized by excessive bone loss [1][2]. Osteoporosis may be triggered by various etiologies. For example, primary osteoporosis occurs with aging, whereas secondary osteoporosis occurs when the condition is caused by another disease or medical treatment.
What is the term for a chronic condition characterized by excessive bone loss?
Osteoporosis is a chronic condition characterized by excessive bone loss [1][2]. Osteoporosis may be triggered by various etiologies. For example, primary osteoporosis occurs with aging, whereas secondary osteoporosis occurs when the condition is caused by another disease or medical treatment. Complications of osteoporosis can include ...
Why is osteoporosis imbalanced?
In primary osteoporosis, osteoblast activity slows while osteoclast activity.[1] . Normally, these two functions are balanced but become imbalanced with aging due to changes in hormones.
What should a nurse do for osteoporosis?
Nurses should assess the patient’s knowledge of osteoporosis and provide education regarding dietary intake (such as increasing calcium and vitamin D intake, recognizing foods high in calcium, and limiting sodas or colas, which are usually high in phosphorus), and exercise.
What is the expected outcome of osteoporosis?
An expected outcome for patients with osteoporosis is that the patient maintains ranges of motion in their joints. Patient t-scores and z-scores can also help monitor outcomes and the effectiveness of interventions.
How to contact the National Osteoporosis Foundation?
301-565-2966 (TTY ) niamsinfo@mail.nih.gov. www.niams.nih.gov. National Osteoporosis Foundation. 800-231-4222 (toll-free) info@nof.org. www.nof.org. This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
What are the risk factors for osteoporosis?
Low levels of testosterone, too much alcohol, taking certain drugs, and smoking are other risk factors. Older men who break a bone easily or are at risk for osteoporosis should talk with their doctors about testing and treatment.
What is a bone mineral density test?
A bone mineral density test compares your bone density to the bones of an average healthy young adult. The test result, known as a T-score, tells you how strong your bones are, whether you have osteoporosis or osteopenia, and your risk for having a fracture.
Why is osteoporosis considered a silent disease?
Osteoporosis is called a “silent disease” because you may not notice any changes until a bone breaks. All the while, though, your bones had been losing strength for many years. Bone is living tissue. To keep bones strong, your body breaks down old bone and replaces it with new bone tissue.
How old do you have to be to have a bone density test?
You can have a bone density test to find out how strong your bones are. The U.S. Preventive Services Task Force recommends that women aged 65 and older be screened (tested) for osteoporosis, as well as women under age 65 who are at increased risk for an osteoporosis-related fracture.
What happens to the bones in your 40s?
As people enter their 40s and 50s, more bone may be broken down than is replaced. A close look at the inside of bone shows something like a honeycomb. When you have osteoporosis, the spaces in this honeycomb grow larger, and the bone that forms the honeycomb gets smaller. The outer shell of your bones also gets thinner.
How long does it take for a woman to lose bone?
Have a small body frame. The risk of osteoporosis grows as you get older. At the time of menopause, women may lose bone quickly for several years. After that, the loss slows down but continues. In men, the loss of bone mass is slower. But, by age 65 or 70, men and women are losing bone at the same rate.
What to talk about with a doctor about bone health?
Together you can evaluate your risks. Some things to discuss include your current health, your diet and physical activity levels, and your family background.
How to prevent bone loss in elderly?
Physical activity and diet are vital to bone health in older adults. Calcium, together with vitamin D, helps reduce bone loss . Activities that put stress on bones keep them strong. Find time for activities like walking, dancing, and gardening. Strengthening your body helps prevent falls. Protecting yourself against falls is key to avoiding a broken hip or wrist. All women over age 65 should have a bone density test.
How to prevent fractures?
At all ages, a diet with enough calcium and vitamin D, together with weight-bearing and resistance exercises, can help prevent problems later. You can work with your doctor to check out warning signs or risk factors.
What is the measure of how strong bones are?
The amount of calcium that makes up your bones is the measure of how strong they are. But your muscles and nerves must also have calcium and phosphorus to work. If these are in short supply from foods you eat, your body simply takes them from your bones. Each day calcium is deposited and withdrawn from your bones.
Why are bones important?
Strong bones support us and allow us to move. They protect our heart, lungs, and brain from injury. Our bones are also a storehouse for vital minerals we need to live. Weak bones break easily, causing terrible pain. You might lose your ability to stand or walk. And as bones weaken, you might lose height.
How can parents help kids with bone health?
While children and young adults rarely get bone diseases, kids can develop habits that endanger their health and bones. Parents can help by encouraging kids to eat healthful food and get at least an hour of physical activity every day.
How to review your medicine?
Ask a health care professional to review your medicines. Ask your doctor, nurse, pharmacist, or other health care professional to review all the medicines you are taking. Make sure to mention over-the-counter medicine, such as cold medicine. As you get older, the way some medicines work in your body can change.
What are the rights of osteoporosis?
These rights include access to timely diagnosis; effective intervention and care; involvement and choice in management plans; and support to ensure active, independent living.
Why is osteoporosis important?
Osteoporosis is a disease which makes bones weak and fragile. This greatly increases the risk of breaking a bone even after a minor fall or bump. The disease has no obvious symptoms, so many people don’t know they have osteoporosis until they suffer a fracture. Fractures can be life-altering, causing pain, disability and loss of independence. That’s why it’s important to prevent osteoporosis!
When is World Osteoporosis Day?
World osteoporosis day. World Osteoporosis Day (WOD), marked on October 20, is an annual campaign dedicated to raising global awareness of bone health and the prevention, diagnosis and treatment of osteoporosis and related fragility fractures.
What is the condition that makes bones weak and fragile?
Osteoporosis is a disease which makes bones weak and fragile. This greatly increases the risk of breaking a bone even after a minor fall or bump. The disease has no obvious symptoms, so many people don’t know they have osteoporosis until they suffer a fracture. Fractures can be life-altering, causing pain, disability and loss of independence.
What is the risk of fractures in osteoporosis?
Osteoporosis is a common disease characterized by low bone strength that results in an increased risk of fracture (1). Fractures are associated with serious clinical consequences, including pain, disability, loss of independence, and death, as well as high healthcare costs. Early identification and intervention with patients at high risk for fracture is needed to reduce the burden of osteoporotic fractures (2). The management of a patient with a confirmed diagnosis of osteoporosis or low bone mass (osteopenia) includes assessment of fracture risk, evaluation for secondary causes of skeletal fragility, making decisions on initiation of treatment, and identification of all relevant clinical factors that may influence patient management. This is a review of the key components in the care of patients with osteoporosis prior to treatment.
What is a fracture risk assessment tool?
A fracture risk assessment tool (FRAX) combines CRFs and femoral neck BMD in a computer-based algorithm that estimates the 10-year probability of hip fracture and major osteoporotic fracture (i.e., clinical spine, hip, proximal humerus, and distal forearm fracture ). FRAX can be accessed online at http://www.shef.ac.uk/FRAX (Figure 1), on most software versions of DXA systems, and on smartphones. FRAX is based on analysis of data from 12 large prospective observational studies in about 60,000 untreated men and women in different world regions, having over 250,000 person-years of observation and more than 5,000 reported fractures reported.
What is QCT in osteoporosis?
QCT is a useful research tool to enhance understanding of the pathophysiology of osteoporosis and the mechanism of action of pharmacological agents used to treat osteoporosis. QCT predicts fracture risk, with the correlation varying according to skeletal site and bone compartment measured, type of fracture predicted, and population assessed (26). The ISCD Official Positions state that “spinal trabecular BMD as measured by QCT has at least the same ability to predict vertebral fractures as AP spinal BMD measured by central DXA in postmenopausal women with lack of sufficient evidence to support this position in men; pQCT of the forearm at the ultra-distal radius predicts hip, but not spine, fragility fractures in postmenopausal women with lack of sufficient evidence to support this position in men (26).” QCT is more expensive than DXA and QUS and uses higher levels of ionizing radiation than DXA. T-scores by QCT are typically lower than with DXA (27), thereby overestimating the prevalence of osteoporosis, with the exception of total hip and femoral neck T-scores calculated from 2D projections of QCT data, which are similar to DXA-derived T-scores at the same regions of interest and may be used for diagnosis of osteoporosis in accordance with the WHO criteria. T-scores and femoral neck BMD derived from 2D projections of QCT data may also be used as input for the FRAX algorithm to estimated 10-year fracture probabilities.
What is the best method to measure bone density?
Devices that measure or estimate BMD differ according to their clinical utility, cost, portability, and use of ionizing radiation (Table 6). DXA is the “gold standard” method for measuring bone density in clinical practice (18). There is a strong correlation between mechanical strength and BMD measured by DXA biomechanical studies (19). In observational studies of untreated patients, there is a robust relationship between fracture risk and BMD measured by DXA (11). The WHO diagnostic classification of osteoporosis is based primarily on reference data obtained by DXA (3), and femoral neck BMD provides input into the FRAX algorithm. Most randomized clinical trials showing reduction in fracture risk with pharmacological therapy have selected study participants according to BMD measured by DXA (20). There is a relationship between fracture risk reduction with drug therapy and increases in BMD measured by DXA (21). Accuracy and precision of DXA are excellent (22). Radiation exposure with DXA is very low (23). BMD of the 33% (one-third) radius, measured either by a dedicated peripheral DXA (pDXA) device or a central DXA instrument with appropriate software, may be used for diagnostic classification with the WHO criteria and to assess fracture risk, but is generally not clinically useful in monitoring the effects of treatment (23). DXA measures bone mineral content (BMC in grams [g]) and bone area (cm2), then calculates areal BMD in g/cm2and derives parameters, such as the T-score and Z-score. DXA is used for diagnostic classification, assessment of fracture risk, and for monitoring changes in BMD over time.
What is the best way to diagnose fracture risk?
The identification of a patient at high risk of fracture should be followed by evaluation for factors contributing to low bone mass, skeletal fragility, falls, and fractures. Components of the evaluation include a bone density test, osteoporosis-directed medical history and physical exam, laboratory studies, and possibly skeletal imaging. A bone density test with dual-energy X-ray absorptiometry (DXA) helps with diagnostic classification, assessment of fracture risk, and provides a baseline for monitoring the skeletal effects of treatment. FRAX is a fracture risk algorithm that includes input of femoral neck bone mineral density measured by DXA. The DXA T-score, prior fracture history, and FRAX estimation of fracture risk are used with clinical practice guidelines to determine whether treatment is indicated. The medical history may reveal underlying causes of osteoporosis (e.g., nutritional deficiencies, gastric surgery, medications with adverse skeletal effects) and important risk factors for fracture (e.g., past history of fracture, family history of osteoporosis, or recent falls). Physical exam may show skeletal deformities due to unrecognized fractures (e.g., loss of height, kyphosis, or diminished rib-pelvis space), identify possible secondary causes of skeletal fragility (e.g., blue sclera with osteogenesis imperfecta, urticarial pigmentosa with systemic mastocytosis, dermatitis herpetiformis with celiac disease, or bone tenderness with osteomalacia), and help to recognize patients with poor balance and frailty that might lead to falls. Laboratory studies may show potentially reversible abnormalities (e.g., vitamin D deficiency, hypocalcemia, or impaired kidney function) that must be assessed and corrected, if possible, before starting pharmacological therapy. Disorders other than osteoporosis, requiring other types of treatment, may be found; for example, low serum alkaline phosphatase suggests hypophosphatasia, M-component may be due to myeloma, or hypocalciuria due to celiac disease. There are important safety considerations that can be derived from a pre-treatment assessment, as well. A patient with a blood clotting disorder should not be treated with raloxifene, a history of esophageal stricture is a contraindication for oral bisphosphonates, and previous skeletal radiation therapy precludes treatment with teriparatide or abaloparatide. Skeletal imaging may be helpful when a fracture, malignancy, or Paget’s disease of bone is suspected. Bone biopsy is rarely performed in clinical practice, but may be helpful in some situations, such as when it is necessary to determine the underlying bone disease in a patient with severe chronic kidney disease. For complete coverage of all related areas of Endocrinology, please visit our on-line FREE web-text, WWW.ENDOTEXT.ORG.
When should BMD testing be done?
BMD testing should be done when it is likely to have an influence on patient management decisions. Other organizations and other countries with different economic resources and health care priorities have used a variety of methodologies to develop alternative recommendations (8-10).
Does BMD affect fracture risk?
There is a robust correlation between BMD and fracture risk, with approximately a 2- fold increase in fracture risk for every 1 standard deviation (SD) decrease in BMD (11). However, many or most patients with a hip fracture have a T-score better than -2.5 (12); although fracture risk is higher in patients with very low BMD, there are numerically many more patients with a T-score better than -2.5 than with a T-score of -2.5 or worse, therefore numerically more fractures in those with higher T-scores. The presence of clinical risk factors (CRFs) that are independent of BMD, particularly advancing age, prior fracture, and recency of fracture, can identify patients at high risk for fracture by providing information on fracture risk that is complementary to BMD. The NOF has provided an extensive list of CRFs (Table 3) for osteoporosis and fractures. Since most fractures occur as a result of a fall, it is helpful to recognize risk factors for falling (Table 4) so that appropriate interventions can be made, when possible, to reduce the chances of falling.
How to reduce osteoporosis risk?
Lifestyle changes. Smoking cessation, limited alcohol intake (no more than 2 units per day), and weight-bearing exercises can help reduce the risk of osteoporosis.
What is osteoporosis in nursing?
Nursing Study Guide on Osteoporosis. Osteoporosis is a medical condition wherein the bones become brittle and weak. Normally, bone tissues break down and get replaced constantly. However, osteoporosis involves the inability of the new bone tissues to keep up with the loss of the old bone tissues. Osteoporosis makes the person at a high risk ...
What is the best treatment for osteoporosis in men?
Testosterone replacement therapy in men may also help to reduce the risk of osteoporosis. Bone-building medications. New bone-building medications can help treat osteporosis. These include teriparatide (Forteo), abaloparatide (Tymlos), and romosozumab (Evenity). Calcium and Vitamin D supplements.
What is the diagnosis of a fractured hip in nursing?
Nursing Diagnosis: Impaired Physical Mobility related to bone fracture secondary to osteoporosis as evidenced by presence of hip fracture, severe hip pain rated10/10, failure to perform ADLs, and low bone density score
What are the factors that contribute to osteoporosis?
Having a sedentary lifestyle, smoking tobacco, and/or consuming too much alcohol contribute to the development of osteoporosis later in life.
What is the best test to check for bone fractures?
Physical examination – to check for any bone fractures, bone pain, or stooped posture. Blood test – to check for serum calcium levels. Bone density test – using a low-level X-ray machine to measure the mineral proportion of the bones.
What are some examples of bisphosphonates?
Examples of bisphosphonates include: alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast, Zometa).
Overview
Symptoms
Causes
Risk Factors
Complications
Prevention
- There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include: 1. Back pain, caused by a fractured or collapsed vertebra 2. Loss of height over time 3. A stooped posture 4. A bone that breaks much more easily than expected
Popular Posts:
- 1. emory gold patient portal sign in
- 2. anesthesia patient account portal providence park hospital
- 3. patient portal primary care associated wichita ks
- 4. my ramc patient portal
- 5. advantia health patient portal sweta patel
- 6. novant internal medicine patient portal
- 7. santa rosa hospital patient portal milton fl
- 8. patient portal banister lieblong
- 9. how much does it cost to implement a patient portal
- 10. phobe sumter patient portal