Mental health progress note templates & examples
12 hours ago Learn how you can easily assess, monitor treatment progress, and report outcomes for patients with depression, anxiety, and other mental health concerns. Sample progress reports Explore these concise progress reports that graphically display your client’s change in symptomatology over the course of their treatment. >> Go To The Portal
A mental health progress note is a type of note that nurses, health care personnel, or anyone working in the medical field uses to trace out the progress of their patients. It is also the type of note that has the basic information about the patient. This includes the patient’s mental problem and the medical solution if there is any.
What is a progress note in mental health?
What Is a Mental Health Progress Note? A mental health progress note is a recurring note that licensed behavioral health professionals (e.g., psychologists, counselors, etc.) use to monitor and assess the progress of a patient. It is a brief but standardized form that is generally used in therapy or counseling sessions.
What are your experiences of mental health?
This is a themed continuation of my previous article “Mental Health in College: How Professors Are Not Helping.” However, this article will more specifically focus on my own experiences trying to overcome my poor mental health while also trying to ...
Should I see a mental health professional?
If you experience a downturn in your mood, and it lasts longer than two weeks, this can definitely be a sign that you should talk to a mental health professional. Your symptoms are interfering with your job.
Does your state require mental health reporting?
Notwithstanding the confidentiality described in this section, mental health professionals are required to report abuse to children, vulnerable adults, and people with disablities. Alaska Stat. § 08.95.900 : Licensed Social Workers and their Employees: Jan. 1, 1999

How do you write a mental health progress note?
Mental Health Progress Notes Templates. ... Don't Rely on Subjective Statements. ... Avoid Excessive Detail. ... Know When to Include or Exclude Information. ... Don't Forget to Include Client Strengths. ... Save Paper, Time, and Hassle by Documenting Electronically.
What is a mental health progress note?
The Mental Health Progress Notes documents describe treatment modality, goals and response, as well as the follow-up plan for patients. Documents are in Microsoft Word (. docx) format. If you need these documents in a different format please contact Andy Benjamin, JD, PhD, ABPP.
How would you describe progress in therapy?
In the simplest terms, progress notes are brief, written notes in a patient's treatment record, which are produced by a therapist as a means of documenting aspects of his or her patient's treatment. Progress notes may also be used to document important issues or concerns that are related to the patient's treatment.
How do you write a progress note for a client?
What makes a great progress note? Here are three tips:Tip #1: Write a story. When an individual comes to a health professional with a problem, they will begin to describe their experience. ... Tip #2: Remember that a diagnosis is a label. ... Tip #3: Write a specific plan. ... Alright, as a quick recap...
What should be in a progress note?
Progress notes can and should be relatively brief, focusing on developments since the previous note, and recapitulating only relevant, ongoing, active problems. Cutting and pasting from previous notes without editing or updating is not permitted, and outdated and redundant information should be eliminated from notes.
How do you write a therapy report?
State the reason the client came to you, the highlights of your conversation, and the recommendations for a plan of action. Set a goal for the client and list the steps you recommend for treatment or follow-up sessions. Wrap up the report with your overall evaluation of the counseling session and sign the report.
How do you write a progress report?
Best Practices On How To Write a Progress ReportTreat a progress report like a Q&A. ... Include questions on progress, plans and problems (PPP) ... Allow meaningful completion of the progress report. ... Use section headings to make reading and writing simpler. ... Use simple and straightforward language.
How do you write a simple progress note?
5 Tips for Writing Better Therapy NotesBe Clear & Concise. Therapy notes should be straight to the point but contain enough information to give others a clear picture of what transpired. ... Remain Professional. ... Write for Everyone. ... Use SOAP. ... Focus on Progress & Adjust as Necessary.
How do you document your progress?
Some people even like using Post-It notes to document progress. They can simply remove each Post-It note as they finish a step in the process. Another way to visually track your progress is by creating a visual roadmap for your week or for the timeline until your project is finished.
What is a mental health progress note?
A note that records the progress of a patient. Whether it is a small or a huge progress. Often used by nurses, psychologists, health care workers o...
What is the purpose of the progress note?
People working in the medical field use these notes as a way to understand how far the patient has gone or if there is any improvement from the the...
Why should saying anything bad about a patient be avoided?
Your progress note should always be in a professional level and manner. Bad mouthing a patient for their slow progress is a huge no. As this is not...
How can these progress note templates allow you to create effective progress notes?
Progress notes are a contract between the client and their clinician. They are where treatment goals and plans can be discussed and decided on before they are put into a document to track the treatment progression.
Counselling progress note template & examples
For counselors, progress notes often take a journal-like form, focusing on the process between therapist and client and the counselor's own thoughts and feelings in the work.
Psychotherapy progress note template & examples
Psychotherapy progress notes are notes taken by mental health professionals for the purpose of documenting or analyzing the content of a conversation during a therapy session.
Medical progress note template & examples
Medical progress notes are the part of a medical record where practitioners record details to document a patient's clinical status or progression during the course of hospitalization or over the course of outpatient care. They're a bit different.
Patient progress note template & examples
Patient progress notes are the component of the patient's record in which you record notes about the interaction you had with them, their reason for visiting, examinations performed on them, medications prescribed on the day, and other relevant details.
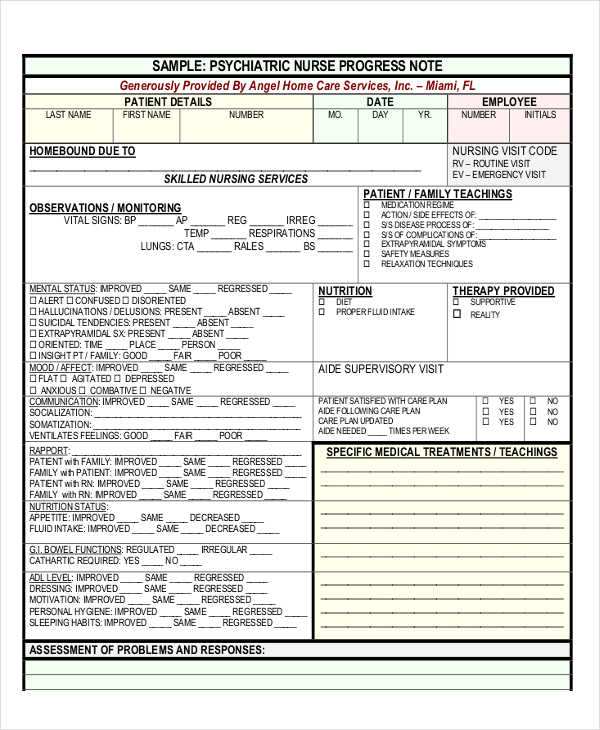
Nursing progress note template & examples
Nursing progress notes are the records kept by nurses during their interactions with each client. These notes help health professionals keep track of the medications and care a patient receives and allow for the patient's medical records to be as up-to-date as possible.
Doctor progress note template & examples
Physicians record their notes concerning the progress or lack of progress made by the patient between the time of the previous note and the most recent note. In addition to this, doctor's progress notes also describe the patient's condition and the treatment given or planned."
What Is a Mental Health Progress Note?
A mental health progress note is a type of note that nurses, health care personnel, or anyone working in the medical field uses to trace out the progress of their patients. It is also the type of note that has the basic information about the patient. This includes the patient’s mental problem and the medical solution if there is any. In addition to that, it also features the progress that is being plotted by the medical personnel who was in charge of that patient.
What is the purpose of the progress note?
People working in the medical field use these notes as a way to understand how far the patient has gone or if there is any improvement from the therapy or the medications being given to them. They then record the progress of the patient’s progress note.
Why should saying anything bad about a patient be avoided?
Your progress note should always be in a professional level and manner. Bad mouthing a patient for their slow progress is a huge no. As this is not helping the patient at all. In addition to that, others are able to read your progress note, and may see what you have done.
Why do we need progress notes for mental health?
The importance of having a mental health progress note is not only to keep track of the progress, but to understand the background or the history of the patient’s problems. It is also used as notes for future study. This is usually done by doctors and for those who may want to know about what may cause it and how to find a solution for others who may also be suffering from it as well.
How to keep a progress note?
Keep your progress note in a professional manner. Avoid using jargon that may be too hurtful or wrong for the patient. Avoid saying anything negative in your notes as these notes are going to be read by others to use for comparison. In addition to that, your progress note should always contain the correct professional information and should not be made as something that you guessed. As any information that may not be true or correct may give out some risks. This should be avoided at all costs.
What is correct information?
Correct information includes the general information of your patient. Their name, age, location and their mental health history. Most of the time, the information is filled out by the nurse or the medical staff who attend to the patient, but there are others who let the patient fill it out to the best of their knowledge. While some tend to ask the closest person which is the family member to fill out the information. The reason the information has to be correct is because this is used as a record for their progress.
Should minor events be listed on progress report?
Anything major or minor events that may have been observed should also be listed down. As this is still part of the progress report. Your patient may have any improvements regardless of how small or huge they are. It should still be written down. These major and minor events are simply milestones if they show any improvement.
What is a non-SNAP PHS 2590?
Use a non-SNAP PHS 2590 if your Notice of Grant Award indicates the grant is excluded from SNAP. If you need more help call your program officer, or grants management specialist named in the Commons.
How long before NIH progress report due date?
Due dates for progress reports are dictated by the individual grant. NIH e-mails you two months before the due date and again two weeks after the deadline, if you haven't sent it by then. It is your responsibility to submit these reports in a timely way.
How long is a progress report required for NIMH?
Progress Reports. Many NIMH grants are funded for more than one year. Once the initial award is made, NIMH requires that an annual progress report (aka a non-competing continuation application) be submitted and reviewed by Institute staff. NIMH approval of the progress report is a mandatory step before funds can be released for ...
What is a progress report?
The Progress Report contains a "Progress Report Summary" section where the PI is asked to provide a two-page summary of the research accomplishments during the past year. Program Officers treat this section of the Progress Report quite seriously and look to it to provide critical information concerning the continued viability of the project. Please note that you should report ONLY research progress which is directly related to the grant in question. The Progress Report should NOT be used to summarize all research activity in which your lab has engaged in the past year.
Is eSNAP a PHS 2590?
Electronic SNAP or eSNAP. Non-SNAP. For most R series awards, use SNAP, which requires you to fill out only certain pages of the PHS 2590 form in addition to the scientific narrative. Your Notice of Grant Award will indicate whether or not the grant is subject to SNAP.
Where can I send a citation to a journal?
You can also link to your manuscripts at NIH's new public access Web site at National Library of Medicine's PubMed Central. As a PI, you can start uploading your manuscripts now at NIH Manuscript Submission; others may submit them on your behalf.
Who is responsible for assessing scientific progress on your grant?
The program officer is responsible for assessing scientific progress on your grant. The grants management specialist conducts a fiscal and regulatory review. There must be agreement from both before the progress report is approved and ready for the next funding period.
What is the difference between progress notes and psychotherapy notes?
Know HIPAA’s Distinction between Progress Notes and Psychotherapy Notes: Therapists who are HIPAA-covered entities should be knowledgeable about the concept of “Psychotherapy Notes” according to HIPAA. The HIPAA-created “Psychotherapy Notes” category is different from progress notes. According to HIPAA, Psychotherapy Notes exclude: “medication prescription and monitoring, counseling session start and stop times, the modalities and frequencies of treatment furnished, results of clinical tests, and any summary of the following items: Diagnosis, functional status, the treatment plan, symptoms, prognosis, and progress to date”. This implies that HIPAA clearly excludes content that is ordinarily used to document the patient’s treatment, e.g., the content that is ordinarily noted in progress note (www.camft.org).
Why should therapists minimize documentation?
Consider Patient Requests: Some patients ask their therapist to minimize documentation in the record in order to protect the information from certain parties or to avoid potential legal problems. In such situations, clinicians should maintain a balance between meeting documentation requirements and safeguarding the patient’s interests by separating discussions with patients from the rest of the medical record (www.therapynotes.com).
What are the legal and ethical considerations for progress notes?
Legal and Ethical Considerations: While there are no specific legal or ethical standards that govern the format or content of a progress note, as a general rule, therapists need to take practical steps to ensure accurate documentation that reflects the care provided.
Why is it important to keep records of psychological services?
Maintaining appropriate records of psychological services allows providers to monitor their work and promotes continuity of care. Good records protect both the patient and psychologist in the event of legal proceedings and are also essential for the psychologist to obtain appropriate reimbursement for services rendered. Psychiatry transcription service providers play a key role in helping mental health specialists ensure accurate and timely record keeping.
What format do therapists use to write progress notes?
For instance, while some clinicians keep detailed notes, others prefer to record only essential information. Many follow the S.O.A.P. format:
What is progress note?
Provide Evidence that Competent Care was Provided: Progress notes allow a therapist to document their ongoing efforts to assess and manage the patient’s symptoms and also document their how they exercise judgment when dealing with complex and challenging treatment scenarios.
What information should be included in a progress note?
Avoid Shortcuts: Every time a progress note is created, it should include all the necessary information: the clinician’s full name, date, time, patient name, patient identifier and electronic signature. This is strongly recommended for legal and ethical reasons, especially in a multi-provider context.
How many items were included in the PREMs?
A total of 86 articles examining 75 PREMs and totaling 1932 items were included. Only four PREMs used statistical methods from item response theory (IRT). The 1932 items covered seven key mental health care domains: interpersonal relationships (22.6%), followed by respect and dignity (19.3%), access and care coordination (14.9%), drug therapy (14.1%), information (9.6%), psychological care (6.8%) and care environment (6.1%). Additionally, a few items focused on patient satisfaction (6.7%) rather than patient experience. No instrument covered the latent trait continuum of patient experience, as defined by the inductive qualitative approach, and the psychometric properties of the instruments were heterogeneous.
What are the objectives of a systematic review of prems?
Given the growing number of PREMs and the need for using them in clinical settings, the objectives of this systematic review were to 1) identify all available PREMs designed to measure the mental health care experience of adult patients, 2) provide an overview of their content and psychometric properties, and 3) critically analyze the methodological quality of these instruments using a set of pre-established robust criteria.
What database was used for the Prisma review?
A comprehensive review following the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines was conducted using the MEDLINE database with no date restrictions. The content of PREMs was analyzed using an inductive qualitative approach, and the methodological quality was assessed according to Pesudovs quality criteria.
What are the criteria used to assess the quality of the instruments?
The criteria used to assess the quality of the instruments are derived from the Quality Assessment Criteria framework developed by Pesudovs et al.40Originally designed to perform a standardized assessment of the quality of the development process and the psychometric properties of patient-reported outcome measures (PROMs), Pesudovs’ criteria proved to be relevant for evaluating PREMs.41These criteria are presented in Table 1. Each instrument was independently rated by two authors (SF and LB) as positive (⩗⩗), acceptable (⩗) or negative (X) against each criterion. When consensus could not be reached, a third author (GF) was consulted.
How was data extracted from the included articles?
Excel was used to collect all the relevant information from the included articles using a predefined data extraction form. The following data were extracted for each instrument: general data (author(s) and year of publication, name and abbreviation of the instrument, country and language of origin, study objective(s), characteristics and size of the sample, administration method), structure (number of items, number and labels of dimensions/factors, time frame, response scale), development characteristics (viewpoints and sources for item development) and some psychometric properties (reliability and construct validity).
What are inclusion criteria in mental health?
The inclusion criteria were as follows: (i) articles dealing with the process of development and/or validation of any instrument intended to be used and/or applicable in the context of mental health care; (ii) adult participants, regardless of their care setting; (iii) instruments designed to capture the experience of patients/service users; and (iv) study written in English. This means that any study describing, at least in part, the operationalization of the construct, item development, pretesting or psychometric analyses were included.
Where is the Institute for Research and Information in Health Economics located?
3Institute for Research and Information in Health Economics (IRDES), Paris, France
What is client progress report?
Client Progress Report for Psychotherapy PDF template provides the essential information that should contain in a clinical psychotherapy report such as the name of the patient, the type of session made with the patient, the date of the session, a comprehensive assessment, and treatment goals and objective for the patient/client.
What is a school counselor's progress report?
School Counseling Progress Report Sample will help teachers or school counselors to record and monitor students progress in an efficient manner. It provides a standard way of scoring or evaluating students.
What is a management report?
A management report is a periodic report type, in which manager's in a company is able to provide valuable feedbacks about the operations undertaken by certain departments within a definite time interval. Business.
What is a daily report template?
Personnel Daily Report Template is a perfect report sample to track the daily completion of the predefined goals. With this template, employers or managers can easily see the performance of employees easily.
What is an alumni chapter annual report?
Alumni Chapter Annual Report template is a yearly report about the activities of an alumni organization. On the other hand, template displays the feedback field for the association.
What Are Progress Notes?
Counselling Progress Note Template & Examples
Psychotherapy Progress Note Template & Examples
Medical Progress Note Template & Examples
Patient Progress Note Template & Examples
- Patient progress notes are the component of the patient's record in which you record notes about the interaction you had with them, their reason for visiting, examinations performed on them, medications prescribed on the day, and other relevant details. Click here to see an example.
Nursing Progress Note Template & Examples
Doctor Progress Note Template & Examples
Group Therapy Progress Note Template & Examples
Do's and Don't When Writing Progress Notes & Examples.
Types of Progress Reports
Progress Report Due Dates
- Due dates for progress reports are dictated by the individual grant. NIH emails you two months before the due date and again two weeks after the deadline, if you haven't sent it by then. It is your responsibility to submit these reports in a timely way. Please note, a late progress report can delay and possibly reduce your award.
Progress Reports Review Process
Assessing Scientific Progress
Tracking Human Subject Usage
Changes in Human and Animal Subject Usage
Reporting on Personnel
Popular Posts:
- 1. detar patient portal
- 2. patient portal statistics
- 3. carithers pediatric patient portal
- 4. emory healthcare patient portal index html
- 5. patient portal ntmc
- 6. imprints patient identification information on each report
- 7. ivch patient portal login
- 8. meridian visiting physicians patient portal
- 9. sign up for cvfp patient portal
- 10. patient portal dr morlan