The Productivity Report - Trinity Health
22 hours ago Measuring and managing clinical productivity is one of the most popular uses of our in-depth efficiency reports. These reports allow CPSC members to track productivity in both work and/or total RVUs, and by unit frequency at the department, specialty or individual provider level. Your group can use the data in these wide-ranging reports to: >> Go To The Portal
The Productivity report provides an analysis of productivity over any period, both retrospectively and prospectively. You can view data such as actual vs. budgeted time, percent utilization, actual Hours per Patient Day (HPPD), and budgeted HPPD. You cannot set a filter in the Productivity Report.
Full Answer
What is a Productivity Report?
Using productivity reports are a great way to keep track of employee productivity in your business. A productivity report usually combines data from several metrics to give managers a broader view of employee productivity. And unlike metrics, productivity reports aren’t limited to separate functions of the organization.
How is productivity measured in the medical field?
Depending on the medical setting and the goals of the organization, productivity will be measured differently. It might be measured by the outcomes versus cost in a value-based primary care practice, whereas in a primarily fee-for-service setting, it might focus on the number of patient encounters per day.
How long is a hospital's productivity?
Many hospitals are now tracking daily productivity. The same equation is used for the daily calculation, with 24 hours as the time period instead of 14 days as in the example.
How does physician productivity affect the ROI of a hospital?
From a hospital’s perspective, greater physician productivity directly affects the hospital’s ROI via increased patient volume. Well-designed productivity programs also should lead to second-order effects like enhanced reputation and quality, which spur further increases in volume and satisfaction.
What is a productivity report in healthcare?
In the healthcare sector, the traditional measures of productivity are the labor output per health worker and the cost of the goods/services. Here, the two key metrics are time and financials, which directly focus on the bottom line of your operations, rather than the quality of services you provide.
What is in a productivity report?
The Productivity report provides an analysis of productivity over any period, both retrospectively and prospectively. You can view data such as actual vs. budgeted time, percent utilization, actual Hours per Patient Day (HPPD), and budgeted HPPD.
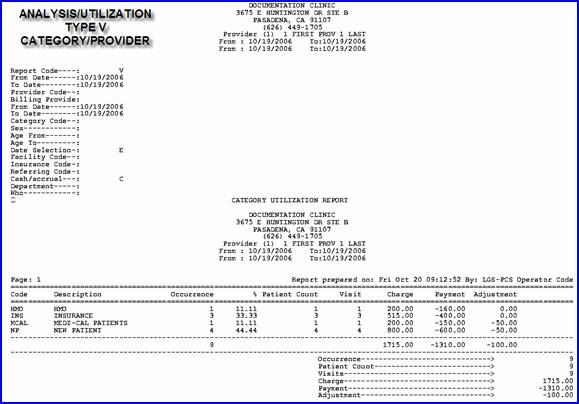
What is a provider productivity report?
Provider Productivity - This report provides summary totals for all procedures rendered by a provider, grouped by provider, and sub-grouped by location, over a period of time. Daily Report - This report provides an analysis of daily transaction activity, including charges, adjustments, and payments.
How is productivity measured in healthcare?
Hospital productivity is measured as the ratio of outputs to inputs. Outputs capture quantity and quality of care for hospital patients; inputs include staff, equipment, and capital resources applied to patient care.
What are the 4 essential components of productivity?
What Are the 4 Essential Components of Productivity?Your Ability to Plan (Strategically) What are you doing tomorrow? ... Your Desire to Remain Focused (One Project at a Time!) This is perhaps the hardest element of productivity, but one which you can master in time. ... Making the Right Choices. ... Your Consistency.
Why is productivity report important?
Being the indicator of business performance, many companies use productivity metrics to measure their own performance standards and to assess their own progress too. By accurately measuring individual productivity, a business can significantly increase its revenue and take a winning position in the industry.
How do you measure productivity of a provider?
To measure productivity for individual physicians:Collect data on the number of procedures each physician has performed by CPT code for a given period.Multiply the number of procedures by the total RVUs (or work RVUs only) for each CPT code. ... Total the products.More items...
What is physician productivity?
What is physician productivity? In simplest terms, physician “productivity” is a measure of a physician's work or output. A physician is considered more productive when he or she generates greater results according to the measure used.
How do physicians measure performance?
Physicians are compared using the cost of patients (population-based measurement) and episodes of care (episode-based measurement) attributed to them and are measured against benchmarks after adjustment for risk and episode (disease) class, patient severity, physician specialty, geographic area, and patient pharmacy ...
What is patient productivity?
This may have included number of patients seen, the speed of their care received or the overall amount of time that each physician or staff member spent on each patient. In this model of care, productivity is measured by how fast patients can move through the practice, not necessarily on the quality of care.
What is productivity in nursing?
Productivity has been defined as a measure of output per unit of input. Within the discipline of nursing, productivity is described as proof or evidence of how efficient the NP is in his/her labor, job setting, or how efficiently she/he handles resources and equipment (Martin, 2005).
What is a productivity standard?
Productivity standards are achieved when: The correct pieces of equipment are used on the various surfaces involved. Cleaning tasks are carried out at required frequencies. All the employees carry out their cleaning tasks in a consistent manner.
What is clinical fingerprint?
The Clinical Fingerprint Report allows members to compare their case mix of physicians with the average physician in the CPSC. This customized analysis delivers a deeper understanding of underlying productivity and places selected institutions’ case mixes on a percent-to-total basis in a side-by-side comparison. Choose reports like this to help your medical practice administration create a more informed plan for improving clinical productivity.
What is CPSC data?
CPSC data can give you a deeper understanding of the impact mid-level providers have on your faculty’s productivity. By using billing and service provider information from your organization’s data file, our intuitive reporting algorithms identify the actual and adjusted work RVUs generated by an attending physician — plus the physician’s contribution of work RVUs from the mid-level providers who support him or her. This provides an invaluable resource for boosting clinical productivit y and, in turn, your bottom line.
What is productivity report?
The Productivity report provides an analysis of productivity over any period, both retrospectively and prospectively. You can view data such as actual vs. budgeted time, percent utilization, actual Hours per Patient Day (HPPD), and budgeted HPPD.
What is the minimum value of productive hours in Budget Data?
Budget Data dialog box: Productive Hours must be a value greater than 0.00.
How to set overtime multiplier in payroll?
Employees dialog box, Payroll tab: Set Overtime multiplier to a number greater than 1. If Use profile Settings selected for Overtime Daily or Overtime Weekly, then OT settings need to be set for the employee’s profile in Staff Manager Administrator(see below).
What is reporting hours?
Reporting in Hoursprovides data based on target, budget, and productive hours.
What is the % coverage value in Assignments?
Assignments dialog box, Task tab: % Coverage value should be between 1% and 100% (should not be 0).
How to send a report to multiple people?
Enter your email address in the Email Recipientsbox. If you want, you can also add additional email addresses to send the report to other people. When entering multiple addresses, separate the email addresses with the punctuation used by your facility; this is usually a comma (,) or a semi-colon (;). The report uses the exact text you enter here in the email To: line when sending the report output.
Can you set a filter in a productivity report?
You cannot set a filter in the Productivity Report. Instead, you should use the Report Selection page to limit the data included in the report.
How to measure productivity?
Another useful measurement of productivity is the calculation of overtime (OT): actual number of OT hours worked divided by actual productive hours worked equals OT percentage. This equation is used for the same time period to determine what percentage of the total work hours were worked using OT.
How to evaluate department productivity?
To evaluate the department's productivity, you must first establish the target or goal for the department if it were 100% productive. The target is determined with the following formula: measurement of work multiplied by the budgeted hours per patient day (HPPD) for a defined period (usually the 14-day pay period).
How many hours does an ADT take?
In a very conservative estimate, an ADT takes at least 1 hour of nursing time. Therefore, you can safely estimate that this unit has earned 63 additional hours of nursing care in the productivity target, entitling it to 63 earned hours for the 2-week pay period.
What is departmental performance?
The departmental performance or budget report compares the actual versus budgeted amounts of revenue, expense, and key performance indicators, including equivalent patient volume or units of service, HPPD, salaries per patient day (SPPD), supplies per patient day, and FTEs used to provide care. For most nursing units, the measure of service is patient days, which is determined by combining inpatients, outpatients, and outpatients in a bed. HPPD can be divided into two groups: productive and nonproductive hours. The type of hours that go into each of these subaccounts will vary, so it's important to know how your hospital manages these hours.
What is equivalent patient day?
Equivalent patient days are made up of observation patients, outpatients in a bed, and inpatients. Payers reimburse observation patients and outpatients in a bed by the number of minutes the patient is in a bed. When the minutes accumulate to equal 24 hours, the area is given credit for 1 patient day.
What are some examples of differences between hospitals?
An example of differences between hospitals is that some include orientation and education in productive hours and others may not. In general, productive hours are those hours staff members have worked in direct patient care, as well as some support hours such as manager, meeting, and training hours.
What is the largest group of hospital employees?
Labor costs make up most hospital expenses, and nursing is the largest group of hospital employees.
How is productivity measured in healthcare?
It might be measured by the outcomes versus cost in a value-based primary care practice, whereas in a primarily fee-for-service setting, it might focus on the number of patient encounters per day.
How to improve physician productivity?
In order to support productivity initiatives in key physician practices, healthcare executives need to drive performance through effective leadership, incisive data and analytics and financial arrangements. They also should identify the main barriers to productivity and evaluate trade-offs created by eliminating those barriers.
How does physician productivity affect hospital ROI?
From a hospital’s perspective, greater physician productivity directly affects the hospital’s ROI via increased patient volume. Well-designed productivity programs also should lead to second-order effects like enhanced reputation and quality, which spur further increases in volume and satisfaction.
What are the benefits of productivity initiatives?
If a productivity initiative encompasses the right tools, metrics and incentives as well as addresses physicians’ and other clinicians’ concerns about workflow barriers, benefits should include increased professional satisfaction, reduced turnover and improved overall hospital culture.
What are the barriers to productivity?
Barriers to productivity can range from the minor, such as small design problems within the facilities, to the systemic, such as inefficient document feedback, laboratory bottlenecks and slow-loading electronic health records (EHRs).
What is the role of a physician leader?
Choosing a physician leader is a critical decision; the physician should have a natural emotional intelligence but also may need training in performance management techniques. Physician leaders should model the desired behavior and be able to manage and coach others toward the model.
How many metrics should be used to measure productivity?
Different medical units will select different ways to measure productivity. No matter the unit, though, there should be no fewer than three metrics chosen, and their logic should be transparent. Leaders should strive to provide accessible data on current performance against all metrics as timely and as close to the point of care as possible.
Why is it important to have a productivity report?
Productivity reports are essential to boost employee productivity. However, manual reports are prone to error and using them could lead to inaccurate decision making. Using a time tracking tool that generates automatic productivity reports can help you easily compare and boost the productivity of every staff member.
Why do businesses use manual productivity reports?
Many businesses use manual productivity reports to measure the performance of their staff.
Why do managers use HR metrics?
Managers can use HR metrics to understand the workflow of the HR team of the organization.
What is sales metrics?
Sales metrics help managers determine the performance of their sales team.
What is productivity in business?
Productivity is traditionally defined as the measurement of units of output against units of input. Generally, you can group productivity into four types: Labor Productivity: Measures the efficiency of an organization’s employees by considering the output per labor hour.
What is Activity Summary Report?
The Activity Summary report shows the amount of active minutes, seconds, unproductive hours, mobile time and manual time logged for each user within a given period.
Why is it important to measure productivity?
Measuring productivity is essential to understand how your organization can function better.
How is productivity measured in healthcare?
In this model of care, productivity is measured by how fast patients can move through the practice, not necessarily on the quality of care . In a financial sense, productivity might be measured by the cost of hiring staff during peak hours, or keeping physicians on the clock longer than necessary to either see patients or fill out paperwork.
What are the barriers to productivity in a clinic?
In terms of emotional wellbeing, clinics should also consider reducing any physical barriers to productivity, like cluttered areas and uncomfortable spaces.
What are the metrics that measure productivity?
This means that often times measuring productivity must include both “hard” metrics, like time spent with patients and cost per patient , as well as “soft” metrics like patient (and staff) satisfaction, and the overall value and quality of care provided.
What is positive productivity?
In which case, positive productivity would include reducing clinic hours to save costs or to only hire staff that is absolutely necessary for the most essential patient care. While keeping both costs and time constraints low may improve some aspects of care, they are not necessarily the best measures of success.
Why is patient satisfaction important?
Patients with higher satisfaction rates in the clinic are often more inclined to give positive reviews outside of the clinic, whether online or to friends and family. This can improve the overall reputation of your practice and increase quality of care given.
Why do patients have more access to their own medical records?
Patients who have more access to and control over their own medical records are also shown to view healthcare services more favorably.
Why should clinics use electronic medical records?
For example, clinics should be using Electronic Medical Records (EMRs), so that patient notes stay organized and note taking is made easier. Paper forms and records may take more time to record, file and track down during busy days.

Settings Affecting The Productivity Report
Viewing The Productivity Report
- The Productivity Report displays values in hours, FTEs, Hours/UOS, or a combination of these, depending on what you selected on the report selection page. The report can also have one to four sections, depending on your report selections. 1. Productivity Graphs: You can select to display an Hours/UOS variance graph, a cumulative variance graph, or both, but the report can o…
Notes on Formatting
- Cumulative volume values are followed by CUM and average workload values by Avg. Variances: Positive variances display/print in bold red type; negative variances display/print in italic blue type. The use of bold and italics provides a visual flag when printing in black and white.
Sample Reports
- The following illustration shows a sample of all three reporting options: Summary, Detail by Partition and Skill, and Detail by Skill. 1. Workload measurement label 2. Bold red text indicating a positive variance 3. Italic blue text indicating a negative variance The following illustration shows a Productivity Report for the ancillary department Respiratory Therapy. The report displays the S…
Popular Posts:
- 1. bay care patient portal login
- 2. fearmonti patient portal
- 3. delta health patient portal
- 4. athenahealth fl - dr josephine v jasper md patient portal
- 5. dr gregory ryan patient portal
- 6. vicki seidmeyer patient portal
- 7. mesa view medical group patient portal
- 8. patient portal hoag hospital dr. leehealey
- 9. st louis medical clinic patient portal
- 10. patient portal dr confon