Interoperability and Patient Access Fact Sheet | CMS
12 hours ago Jul 17, 2020 · The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a … >> Go To The Portal
What does the interoperability and patient access final rule mean for You?
Jul 17, 2020 · The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a …
What does better interoperability mean for patient engagement technology?
Apr 26, 2018 · Interoperability, APIs Critical for Effective Patient Portal Use APIs will help enhance patient engagement technology by allowing patients to plug their health information in from multiple patient portals. Source: Thinkstock By Sara Heath
How can healthcare professionals make patient portals more useful?
blueEHR Interoperable Patient Portal Patient portals are changing the healthcare paradigm. A growing percentage of patients are more involved in their care, looking for ways to access care plans, medical records and more. With blueEHR, you get one of the industry’s leading interoperable patient portals.
What is the health interoperability ecosystem?
Nov 02, 2015 · November 02, 2015 - When it comes to delivery of medical test results, patients are comfortable enough with healthcare interoperability to prefer password-protected websites or portals over more...
What is the interoperability and patient access rule?
CMS Interoperability and Patient Access Final Rule The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it.Dec 9, 2021
What is patient interoperability?
Interoperable electronic health records (EHR) allow the electronic sharing of patient information between different EHR systems and healthcare providers, improving the ease with which doctors can provide care to their patients and patients can move in and out of different care facilities.
What is an example of interoperability in healthcare?
Semantic interoperability healthcare systems leverage data in a standardized way as they break down and share information. For example, two systems can now recognize terminology, medication symbols, and other nuances while exchanging data automatically, without human intervention.Apr 9, 2021
What is a patient portal used for?
A patient portal is a secure online website that gives patients convenient, 24-hour access to personal health information from anywhere with an Internet connection. Using a secure username and password, patients can view health information such as: Recent doctor visits.Sep 29, 2017
How do you achieve interoperability in healthcare?
Steps that can be Taken to Improve InteroperabilityUse a health information exchange (HIE) system while diagnosing the patient.Make use of neuro-linguistic programming and voice recognition in your system.Move to a single integrated EHR platform.Integrate workflows with point-of-care images.More items...•Mar 6, 2021
What are healthcare interoperability standards?
Interoperability Standards In order to seamlessly digest information about an individual and improve the overall coordination and delivery of healthcare, standards permit clinicians, labs, hospitals, pharmacies and patients to share data regardless of application or market supplier.
What are the 3 types of interoperability?
There are four levels of interoperability: foundational, structural, semantic, and organizational.Mar 8, 2022
What are the three levels of interoperability?
There are three levels of health information technology interoperability that correlate with data-exchange opportunities: 1) foundational; 2) structural; and 3) semantic.Nov 17, 2014
Which is an excellent example of interoperability issue?
Interoperability enables safer transitions of care, which leads to better patient outcomes over all. For example, a patient who is on vacation and falls ill may not be able to provide all details of his medical history, which can make all the difference to the doctor charged with his care.May 30, 2017
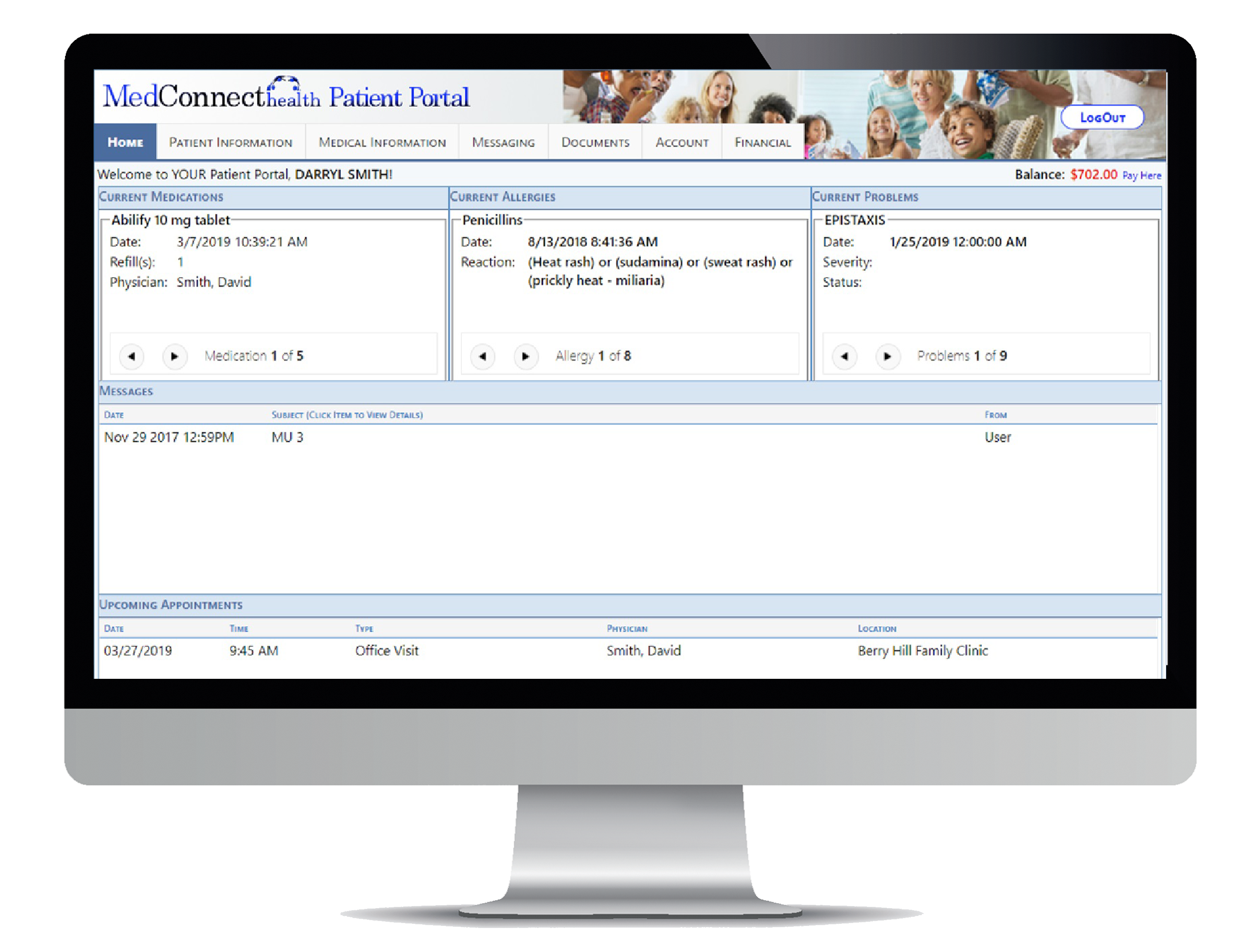
What should be included in a patient portal?
A robust patient portal should include the following features:Clinical summaries.Secure (HIPAA-compliant) messaging.Online bill pay.New patient registration.Ability to update demographic information.Prescription renewals and contact lens ordering.Appointment requests.Appointment reminders.More items...
Is patient portal a system?
There are two main types of patient portals: a standalone system and an integrated service. Integrated patient portal software functionality usually comes as a part of an EMR system, an EHR system or practice management software. But at their most basic, they're simply web-based tools.Feb 12, 2021
Why is the patient portal a good tool for patient engagement?
Background. Engaging patients in the delivery of health care has the potential to improve health outcomes and patient satisfaction. Patient portals may enhance patient engagement by enabling patients to access their electronic medical records (EMRs) and facilitating secure patient-provider communication.
What is interoperability in healthcare?
When implemented effectively, health information exchange (interoperability) can also reduce the burden of certain administrative processes, such as prior authorization. We have issued regulations that will drive change in how clinical and administrative information is exchanged between payers, providers and patients, and will support more efficient care coordination.
What is CMS 9115-F?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it. This final rule focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, Children's Health Insurance Program (CHIP), and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is CMS Interoperability and Patient Access Final Rule?
In August 2020, CMS released a letter to state health officers detailing how state Medicaid agencies should implement the CMS Interoperability and Patient Access final rule in a manner consistent with existing guidance. There are many provisions in this regulation that impact Medicaid and CHIP Fee-For-Service (FFS) programs, Medicaid managed care plans, and CHIP managed care entities, and this letter discusses those issues. Additionally, this letter advises states that they should be aware of the ONC’s 21st Century Cures Act final rule on information blocking. The link for the letter is:
What is the 21st century cures act?
Office of the National Coordinator for Health Information Technology's (ONC) 21st Century Cures Act Final Rule. The Department of Health and Human Services (HHS) finalized technical as well as content and vocabulary standards in the ONC 21st Century Cures Act final rule, which CMS adopted to support these API policies.
What is FHIR release 4.0.1?
FHIR Release 4.0.1 provides the first set of normative FHIR resources. A subset of FHIR resources is normative, and future changes on those resources marked normative will be backward compatible. These resources define the content and structure of core health data, which developers to build standardized applications.
What is Smart on FHIR?
SMART on FHIR provides reliable, secure authorization for a variety of app architectures with the OAuth 2.0 standard. This profile is intended to be used by app developers that need to access FHIR resources by requesting access tokens from OAuth 2.0 compliant authorization servers. The profile defines a method through which an app requests authorization to access a FHIR resource, and then uses that authorization to retrieve the resource.
What is OpenID Connect 1.0?
OpenID Connect 1.0 is a simple identity layer on top of the OAuth 2.0 protocol. It enables clients to verify the identity of the end-user based on the authentication performed by an authorization server, as well as to obtain basic profile information about the end-user in an interoperable and RESTful manner. This specification defines the core OpenID Connect functionality: authentication built on top of OAuth 2.0 and the use of claims to communicate information about the end-user. It also describes the security and privacy considerations for using OpenID Connect.
blueEHR Interoperable Patient Portal
A growing percentage of patients are more involved in their care, looking for ways to access care plans, medical records and more. With blueEHR, you get one of the industry’s leading interoperable patient portals. You or your patients can opt to integrate with any EHR system, share records, and view medical history.
Build trust with patients and deliver the information they need
Provide a personal health record (PHR) through one of the most advanced and fully integrated patient portals that work across EHR vendors and health information exchanges (HIE).
Why are standards important in healthcare?
Standards provide a common language and a common set of expectations that enable interoperability between systems and/or devices. In order to seamlessly digest information about an individual and improve the overall coordination and delivery of healthcare, standards permit clinicians, labs, hospitals, pharmacies and patients to share data regardless of application or market supplier.
What is the adoption and implementation of standards?
The adoption and implementation of standards involves a testing ecosystem that spans standards development, implementation and feedback from real-world testing into the development process to support continuous improvement. There are various different testing and compliance efforts that support advancing health IT interoperability, including:
What is interoperability in health?
The health interoperability ecosystem comprises individuals, systems and processes that want to share, exchange and access all forms of health information, including discrete, narrative and multimedia.
What is the HHS?
With the goal of achieving ubiquitous, interoperable, nationwide exchange, the U.S. Department of Health and Human Services (HHS) has enacted and implemented a variety of legislation, regulations and guidance to further the adoption of standards-based approaches to interoperability.
What is core data?
Core Data for Interoperability is a “standardized set of health data classes and constituent data elements for nationwide, interoperable health information exchange.”. A “Data Class” is an “aggregation of various Data Elements by a common theme or use case.”.
What is interoperability standards advisory?
The Interoperability Standards Advisory (ISA) process represents a single, public list of standards and implementation specifications published by ONC. ONC coordinates the identification, assessment and determination of these recommended standards and implementation specifications for industry use to fulfill specific clinical health IT interoperability needs. Stakeholders are encouraged to implement and use these recommended standards as applicable to their needs.
What is the HIMSS and PCHAlliance?
HIMSS and PCHAlliance strongly urge prioritization of necessary funding and technical assistance to implement modern health information and technology strategies to ensure timely interoperability and sharing of public health surveillance data. An important component is the work in partnership with the Association of Public Health Laboratories, Council of State and Territorial Epidemiologists and the National Association for Public Health Statistics and Information Systems that support this multi-year effort to modernize public health data systems, surveillance and analytics at the CDC, and state, local and tribal health departments. Funding included in the Fiscal Year 2020 Appropriations Package and the Coronavirus Aid, Relief and Economic Security (CARES) Act, will help address some of the challenges, but in the long term, we need a predictable and sustained funding source to fully tackle this issue.
Popular Posts:
- 1. nyp.org patient portal login
- 2. upmc for you patient portal
- 3. integrative physicians durham nc patient portal
- 4. truckee tahoe patient portal
- 5. my sturdy health patient portal
- 6. jis patient portal
- 7. help with d-h patient portal
- 8. patient medical summary report
- 9. baylor medical patient login
- 10. dermatologists of greater columbus patient portal