How to Read Your Radiology Report
13 hours ago · Next, the radiologist writes a report detailing the results. A typical radiology reports includes these sections: Name or Type of Exam; Date of Exam; Interpreting Radiologist – the name of the radiologist who read the diagnostic imaging exam and wrote the report. Clinical History – describes the patient’s symptoms or existing diagnosis. >> Go To The Portal
A typical radiology reports includes these sections: Name or Type of Exam Date of Exam Interpreting Radiologist – the name of the radiologist who read the diagnostic imaging exam and wrote the report. Clinical History – describes the patient’s symptoms or existing diagnosis.
Full Answer
What does it mean in a radiology report?
The report is the written communication of the radiologist's interpretation, discussion, and conclusions about the radiologic study. The written report is frequently the only source of communication of these results. The report should communicate relevant information about diagnosis, condition, response to therapy, and/or results of a procedure ...
How accurate are radiology reports?
How accurate are radiology reports? A new report finds that radiological errors are common and in many cases are connected to serious injury or death of a patient. New York residents may need to have radiological tests performed as part of their routine preventive health checks or in order to investigate potential health problems.
How to read your radiology report?
Sections of the Radiology Report
- Type of exam. This section shows the date, time, and type of exam. ...
- Clinical history. This section contains personal information, such as your age, gender, and relevant medical information.
- Comparison. Sometimes, the radiologist will compare the new imaging exam with any available previous exams. ...
- Technique. ...
- Findings. ...
What does this radiology report indicate?
The written radiology report is the most critical component of the service provided by a radiologist. It constitutes the formal documentation and communication of the results of a radiologic study or procedure. 1 The reports are usually dictated by a trained radiologist, but reports may vary greatly in style, format, and effectiveness.

What should be included in a radiology report?
According to the respondents, the characteristics that should be included in the radiology report are the quality of the image, details of the clinical presentation, diagnostic impression, examination technique, and information about contrast administration, selected by 92%, 91%, 89%, 72%, and 68%, respectively.
What does the impression on a radiology report mean?
Impression – this is the radiologist's “impression” or diagnosis of the diagnostic imaging exam. This section includes a summary of the results and any follow up testing (like a biopsy or additional diagnostic imaging) that the radiologist recommends.
What does clinical indication mean on a radiology report?
The indication should be a simple, concise statement of the reason for the study and/or applicable clinical information or diagnosis. A clear understanding of the indication may also clarify appropriate clinical questions that should be addressed by the study.
How do you write a radiology report?
10:4028:23Featured Video - How to make a great radiology report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo the emphasis and findings is on short informative and factual phrases. And the impression is theMoreSo the emphasis and findings is on short informative and factual phrases. And the impression is the meaning of the findings which leads to a diagnosis or differential diagnosis.
Can a radiologist tell you results?
They are acquiring diagnostic images according to specific protocols, so that a radiologist (a medical doctor with many years of specialized education) can interpret the images to provide an accurate report of the findings and results of your study.
What does clinically indicated mean?
Medically Indicated means Medical Care provided or ordered by Associate which is necessary in order to treat or care for symptoms of an illness or injury, or to diagnose an illness or condition that is harmful to life or health, and which is commonly and customarily recognized throughout the Associate's profession as ...
Why is patient history important in radiology?
The clinical history and indication (CHI) provided with a radiological examination are critical components of a quality interpretation by the radiologist. A patient's chronic conditions offer the context in which acute symptoms and findings can be interpreted more accurately.
What does non specific mean in radiology report?
Non-specific is used for a symptom, sign, test result, radiological finding, etc., that does not point towards a specific diagnosis or etiology. For example, a high T2 signal lesion of the white matter on an MRI brain is a non-specific finding as the number of possible causes is broad.
How do you read CT reports?
To read a CT scan, start by noting the shades of white, gray, and black. The white area signals dense tissues like bone, the gray area represents soft tissues and fluids, and the dark gray and black area shows air and fat.
How do I present radiology?
Top 10 presentation tipsPay attention to the clinical details.Learn your lines.Comment on image quality - briefly.Describe the 'obvious' abnormality first.Continue systematically.Describe things you are unsure of and come back to them only if you think they are relevant.Check the review areas.More items...
How do I read my MRI results?
MRI interpretation Systematic approachStart by checking the patient and image details.Look at all the available image planes.Compare the fat-sensitive with the water-sensitive images looking for abnormal signal.Correlate the MRI appearances with available previous imaging.Relate your findings to the clinical question.
What is radiographic message?
An image produced by radiation, usually by x-rays, and recorded on a radiosensitive surface, such as photographic film, or by photographing a fluoroscopic image. Also called radiogram, shadowgraph, skiagram, skiagraph.
What is included in a radiology report?
A typical radiology reports includes these sections: Name or Type of Exam. Date of Exam. Interpreting Radiologist – the name of the radiologist who read the diagnostic imaging exam and wrote the report. Clinical History – describes the patient’s symptoms or existing diagnosis.
What does "impression" mean in a radiologist?
Impression – this is the radiologist’s “impression” or diagnosis of the diagnostic imaging exam. This section includes a summary of the results and any follow up testing (like a biopsy or additional diagnostic imaging) that the radiologist recommends. ...
Can you request a copy of a radiology report?
Patients may request copies of imaging studies and/or copies of their radiology reports. Radiology reports will be available to patients following the radiologist’s interpretation of the imaging study. Patients must complete a radiology patient health information release form before the report or images can be released to the patient.
Do you have to complete a release form for radiology?
Patients must complete a radiology patient health information release form before the report or images can be released to the patient. The release form is not necessary for the physician who ordered the exam to receive the report. Frequently Asked Questions.
What is a radiology report?
The radiology report is a crucial diagnostic tool, the considered opinion of a medical expert, and a vital part of your health records. A radiologist writes them, your doctor reads them, and they can help by creating a clearer picture of a pathology. That will ultimately improve your care.
What is the role of a radiologist in a MRI?
When the images are complete, a radiologist examines, or “reads,” them, and writes a report indicating clinically significant details .
Can you write a radiology report without medical lingo?
There’s no way to write a clear, actionable analysis without resorting heavily to medical lingo, which can often look like a foreign language to lay readers. Most radiology reports follow a familiar template. Here are the sections found in the typical radiology report: Exam Type.
Why is a radiology report considered a medical record?
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) considers the radiology report to be part of the medical record because it documents the results of a radiologic test or procedure. 13 In addition, hospitals have specific policies regarding the radiology report as part of the medical record.
Who is the reader of a radiology report?
Most often, the reader of the radiology report is the individual responsible for providing direct patient care. In some cases, the reader will be the patient.
Why is it important to write a radiology report?
The written radiology report is the critical service of radiology and should provide clear and concise communication that is understandable by the intended reader. Since increasingly more often the patient is the reader of the report, it is even more important to keep the report clear and concise.
What is an impression in a radiology report?
Impression. The abstract is the summary of a scientific report. In a radiology report, the summary has been referred to as the "Impression," "Conclusion," or "Diagnosis" section. Sometimes this summary is an impression, sometimes it is a conclusion or diagnosis, and sometimes it is a concise statement of the findings.
Why do radiologists sue?
One of the 3 most common reasons for malpractice suits against radiologists is failure to communicate results clearly and effectively. 2,3 Poor communication is a common reason patients choose to sue the doctor. 5,6 In some situations, such as mammograms, it is helpful to give a copy of the report directly to the patient, which makes it even more important that the report is clear and understandable. 6,7 If a report is written so that a patient can understand what is said, it is much more likely that a healthcare provider, who depends upon the report to make decisions concerning patient management, will also understand the report. 8
Why is recapitulation of the indication for the study at the time of the report dictation appropriate?
Therefore, recapitulation of the indication for the study at the time of the report dictation is appropriate because it will document the actual reason the study was performed. In addition, many third-party payers and Medicare now require an appropriate indication before they will reimburse for a study.
What is routine study in radiology?
Every radiologic study has a procedure associated with performing the examination. For most routine studies, the procedure is implied by the title. For example, a routine study such as a "PA & LAT Chest," by accepted use, implies the procedure (posteroanterior and lateral chest radiograph), and a separate "Procedure" section of the report is not necessary. However, a separate "Procedure" section may be convenient to document informed consent, technical limitations, drugs, and isotopes or contrast material associated with the study. Frequently, reports for invasive procedures are best organized in a separate "Procedure" section.
Providing Access
According to Arun Krishnaraj, MD, MPH, chair of the ACR’s Commission on Patient- and Family-Centered Care, prior to the implementation of the Cures Act, many institutions had varying degrees of embargoes regarding radiology reports.
Providing Context
According to Pahade and Krishnaraj, there has been a lack of resources to support radiologists in communicating within the radiology report in terms that patients understand. So, the two set out to develop and distribute a simple translation resource for patients — helping them to understand the basics of a radiology report.
What is radiology report?
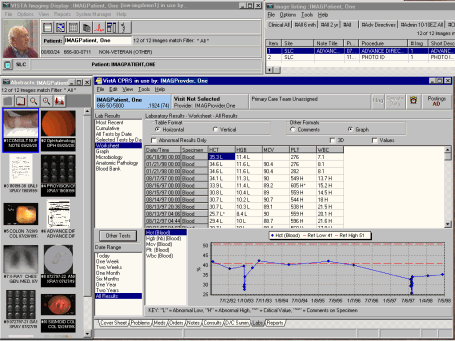
Traditionally, radiology reports comprise text only, using just words to describe and communicate the meaning of the images. Research has proven that people process and retain information visually much more effectively than through words alone.
What is the importance of a radiology report?
First is the interpretation of the study, which involves the identification and recognition of the salient findings and using them to arrive at a diagnosis or a differential diagnosis (in other words, a suggested pathway for further investigation). ...
What should the findings section emphasize?
The findings section should emphasize short, informative, and factual observations while avoiding inappropriate interpretation, excessive use of terms of perception, and redundancy. The impression is the thoughtful synthesis of the meaning of the findings leading to a diagnosis, a differential diagnosis, and management recommendations.
Why use a macro in radiology?
A macro is a predetermined sentence or phrase that can be reused in multiple cases and selected from a repository or software system used to create the radiology report.
What is the second component of a report?
The second component is the equally important element of communicating those findings and conclusions clearly, usefully and unequivocally in a report. Mastering one component does not necessarily mean success in the other. 1. Patients place a high value on procedural correctness and clear communication with their radiologist or ...
Why do radiology reports include X-rays?
Radiology reports have evolved in recent years to include both the X-ray images and schematics or charts to help point out analysis in a visual manner , as studies have shown it is an effective educational tool and beneficial to the patient, according to the Journal of Digital Imaging.
Why is communication important in healthcare?
Communication is a key component of success, but perhaps never more so than in the health care professions. When you communicate clearly with your patients, you have a much greater chance to connect, educate, gain their trust, and thus achieve better patient compliance to treatment. And one of the best ways to communicate clearly ...
Why are radiologists opposed to providing their reports directly to patients?
One of the naysayers’ biggest concerns was that patients wouldn’t be able to understand the content of the reports and could easily misinterpret the results for the worst.
What is the piece of the puzzle that a radiology report is?
The radiology report is only one piece of the puzzle, and patients recognize that their doctors have the other pieces, such as medical history, symptoms, and physical exam. Their doctors are the ones who can put all the pieces together to reach a diagnosis and suggest treatment options, he says.
Why did the PA radiology society oppose the bill?
Berlin says the Pennsylvania Radiological Society, among others, opposed the bill because members feared patients wouldn’t be able to understand the reports. Taxin says there also was opposition because the complex bill was poorly written and would have been costly for radiology practices and hospitals to implement.
How long does it take for a radiologist to report a scan?
The radiologist reads the scan and sends the report to the referring physician. The referring physician reports the results to the patient in a few days to a week.
What would happen if you didn't understand the medical reports?
According to Johnson, the patients also said that if they didn’t understand the reports, they would take steps to have them translated into lay terms. Some said they would do their own research on the Internet; some said they would ask friends and family who were more knowledgeable about medical terms.
Do radiologists have to send mammography reports?
About three years ago, a Pennsylvania state representative proposed a bill that would require radiologists to send reports of all exams directly to patients. The representative was the friend of a lawyer who was outraged when his wife wasn’t told of her cancer findings and died, Berlin says.
When did the Mammography Quality Standards Act become law?
Since 1999, when the Mammography Quality Standards Act was enacted, facilities are required to send a summary of the mammography report to patients. “Since the law went into effect, I’ve never seen a lawsuit where a woman is suing because she wasn’t told she had breast cancer,” Berlin says.