5+ SAMPLE Patient Incident Report in PDF
5 hours ago 5+ SAMPLE Patient Incident Report in PDF. According to the World Health Organization, every year in the United States, up to 440,000 individuals die as a result of hospital errors, which … >> Go To The Portal
What is a patient incident?
As defined by Berxi, a patient incident report is “a detailed, written description of the chain of events leading up to and following an unforeseen scenario in a healthcare context,” which can be either computerized or paper-based. Nurses or other qualified professionals are often responsible for completing reports.
How to submit an incident report?
- Include factors may have contributed to loss
- Include any other relevant information
- State if patient harm was involved
- Use extra sheets if necessary
Should I file an incident report?
Generally, though, you should outline:
- What happened (detailed description of the incident, incident category/type)
- When it happened (date and time)
- Where it happened (be as specific as possible)
- How it happened (Are there any obvious root causes, like a puddle on the floor where an employee slipped)
- Who it happened to (employee name and title)
- Who reported it (Who is writing this document?)
How should an incident report be filed?
Guidelines for filling out the form should include:
- Give a brief narrative description of the incident, consisting of an objective description of the facts (never include the writer's judgment).
- Use quotes where applicable with unwitnessed incident, eg, "patient states."
- Write the name of any witnesses including the nurse practitioner if she/he is not the reporter.
How do you write a patient incident report?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What are some examples of healthcare incidents?
Wrong dose of prescription indicated. Wrong medication supplied. Incomplete or incorrect medication handoffs....3. Incidents related to patient examination include:Delayed/incorrect examination results.Incorrect examination application.Digression from protocols and working agreements.
How do you write a simple incident report?
How to write an incident reportRecord the basic facts. Start by recording basic facts related to the incident. ... Note affected individuals. ... Find witnesses. ... Create a narrative description of the incident. ... Note the injuries. ... Record the treatment. ... Indicate damages. ... Establish a corrective action plan.More items...•
What is an example of an incident?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting. An event in a narrative or drama.
What are patient safety incidents?
Patient safety incidents are any unintended or unexpected incident which could have, or did, lead to harm for one or more patients receiving healthcare. Reporting them supports the NHS to learn from mistakes and to take action to keep patients safe.
What is an incident report in healthcare?
Incident reporting in healthcare refers to collecting healthcare incident data with the goal to improve patient safety and care quality. Done well, it identifies safety hazards and guides the development of interventions to mitigate risks, thereby reducing harm.
What are 3 types of incidents?
3 Types Of Incidents That Stand Out: Is Your Help Desk Prepared?Major Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What are the five elements of good Incident Report?
Facts related to the incident include:The Basics. Identify the specific location, time and date of the incident. ... The Affected. Collect details of those involved and/or affected by the incident. ... The Witnesses. ... The Context. ... The Actions. ... The Environment. ... The Injuries. ... The Treatment.More items...•
What are the three C's of an Incident Report?
Training your brain before you find yourself in a high-pressure situation may help you save a life or potentially help someone in pain. There are three basic C's to remember—check, call, and care. When it comes to first aid, there are three P's to remember—preserve life, prevent deterioration, and promote recovery.
What makes a good incident report?
Effective Incident Reports identify the facts and observations. They avoid inclusion of personal biases; they do not draw conclusions/predictions, or place blame. Effective Incident Reports use specific, descriptive language and identified the action(s) taken by staff as a result of the unusual incident.
How do you write an incident report in nursing?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
What's a medical incident?
A medical incident can be described as unforeseen occurrences that affect patients or staff safety. Medical incidents are mostly related to injuries, equipment failures, administrative flaws, patient care, or medical errors.
What are 3 types of incidents?
3 Types Of Incidents That Stand Out: Is Your Help Desk Prepared?Major Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What are the three types of incident in the hospital work place?
Broadly, there are three types of incident reports:Clinical Incidents. A clinical incident is an unpleasant and unplanned event that causes or can cause physical harm to a patient. ... Near Miss Incidents. Sometimes an error/unsafe condition is caught before it reaches the patient. ... Non Clinical Incidents. ... Workplace Incidents.
What is the most common adverse event in healthcare facilities?
The most common and most consistently reported types of AE in the included studies were operative/surgical-related events, often resulting from procedural complications and injuries such as post-op bleeding or return to surgery.
What is a critical incident in nursing examples?
In nursing, for example, a critical incident could take the form of a medication error, a nosocomial infection or helping a patient achieve a comfortable, dignified death.
How Effective Are Incident-Reporting Systems for Improving Patient Safety?
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a...
When to Report an Incident to the Police?
The general rule of thumb is that an incident report should be completed as quickly as possible after an occurrence happens. Minor injuries should...
How Are Patient Safety Event Reporting Systems used?
Hospitals are replete with patient safety event reporting systems, which serve as a cornerstone of efforts to detect patient safety incidents and q...
What Is the Purpose of Patient Incident Report?
Risk management. Knowing that an incident has occurred can push administrator s to correct factors that contributed to the incident. This would pave the way in avoiding similar incidents that would possibly happen in the future.
Who should sign the incident report?
Once the incident report is complete, ensure that it is signed off by the supervisor who was on duty during the incident. The supervisor should recheck the accuracy of all details before signing, and contact information of the supervisor should be included should there be additional questions to answer
What to include in an incident report?
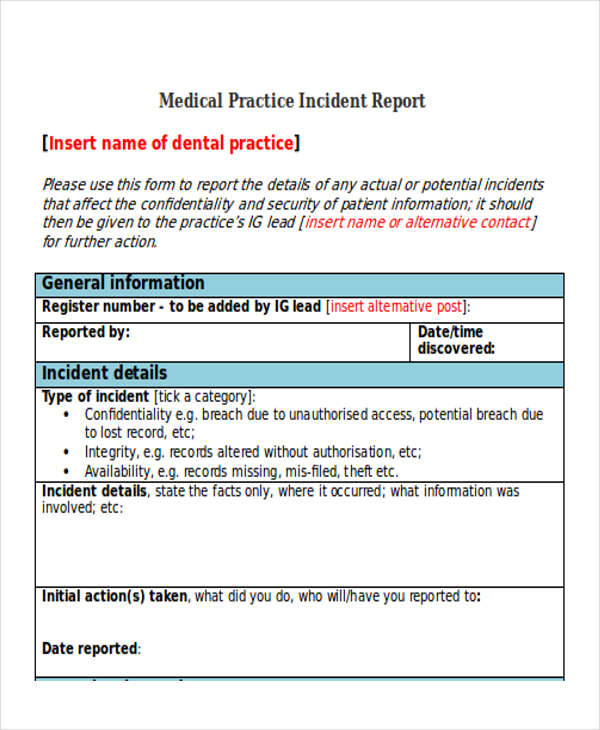
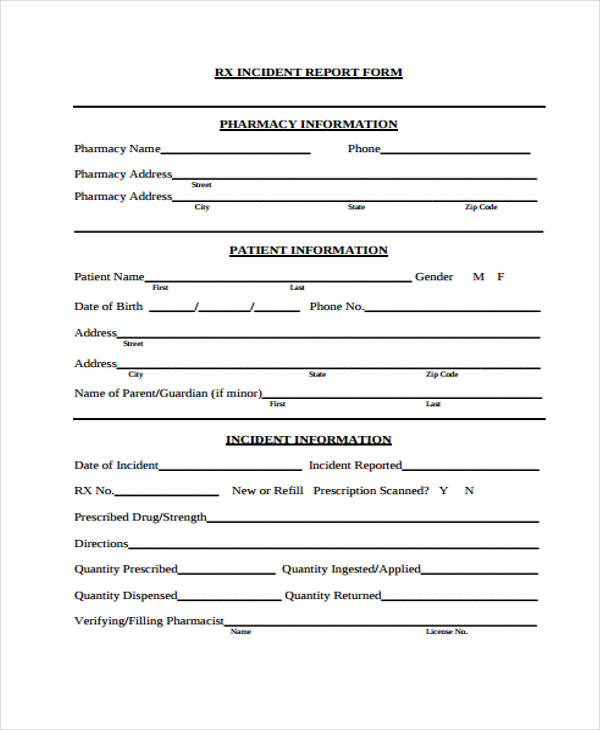
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is 62 percent of incidents not reportable?
Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements. Because of this, the first step to incident management in any healthcare facility is writing strong, clear reporting requirements. Then, staff can submit reports that help correct problems of all types.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What is a harmful incident?
A harmful incident results in injury or illness to a patient or another person. For example, a patient could fall out of bed and break their arm or scratch a nurse as she takes their temperature.
What is incident report?
1. An Incident Report Must Be Accurate and Specific. When you write an incident report, you must be specific and accurate about the details, not merely descriptive. For example, instead of writing "the old patient", it is more accurate to describe him as "the 76-year old male patient".
How to organize an incident report?
How a report is organized depends on the complexity of the incident and the type of report being written. Usually, writing in chronological order is the simplest way to organize a report. However, an inspection incident report may be written by enumerating details according to findings. 5. A Good Incident Report Must Be Clear.
What is the best way to write an incident report?
It is also best to write in an active voice, which is more powerful and interesting than the passive voice. 2. A Good Incident Report Must Be Factual and Objective.
What abbreviations should be used in an incident report?
A Good Incident Report Must Only Include Proper Abbreviations. The use of abbreviations may be appropriate in certain cases, such as the use of Dr. Brown and Mr. Green, instead of writing Doctor or Mister.
What should be stated in a report?
State all facts regarding who, what, when, where, how and why something happened without leaving out important details. Another person who reads the report must be able to get answers to his or her questions about the incident from your report. How many details to include may depend on their relevance to the incident and the policies of your department.
Do you have to include your opinion in a report?
If you must include an opinion in your report, it is best to state it with the similar description that appears on some incident report samples: "In my opinion, there were too many people in the overloaded bus. In fact, there were 80 persons inside, when a bus of this size is only allowed to carry 70 individuals."
Do you have to include statements in a report?
If you have to include statements from a witness or other people, you must clarify that you are quoting someone, and the words you used are not your own.
What is incident report?
An incident report is a formal recording of the facts related to a workplace accident, injury, or near miss. Its primary purpose is to uncover the circumstances and conditions that led to the event in order to prevent future incidents. Every incident report you file should contain a minimum of the following:
When Does an Incident Report Need to Be Completed?
Create an incident report as soon as your employees are safe, which includes seeking medical attention and implementing an immediate corrective action to prevent further danger or damage.
Why is incident reporting important?
Their importance means you want to get as much relevant information as you can as quickly as possible.
What are the two common mistakes you should avoid when reporting an accident?
But sometimes, safety teams can get in their own way and miss out on important details by making common mistakes. Blame-casting and just getting it done are two common incident reporting mistakes you should avoid. It is easy to go on a witch hunt when accidents happen.
Why is it important to include the details above in an incident report?
It’s important to include the above information in as detailed and concise a manner as possible. Holes in your report could lead to inferences and missed opportunities to create a safer workplace.
What is a narrative description of an incident?
A narrative description of the incident, including the sequence of events and results of the incident
How long does it take to complete a fact gathering report?
While it may take a few days to complete your report, it should take you only hours (or less) to start it. After an incident, secure the worksite for all crews and make sure injured employees are receiving medical care if needed. Start your fact gathering for your report immediately after this.
Sample
Use this form to report accidents, injuries, medical situations, criminal activities, traffic incidents, or student behavior incidents. If possible, a report should be completed within 24 hours of the event.
INCIDENT REPORT FORM
Use this form to report accidents, injuries, medical situations, criminal activities, traffic incidents, or student behavior incidents. If possible, a report should be completed within 24 hours of the event.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
What is a Workplace Incident Report?
A workplace incident report is a document that states all the information about any accidents, injuries, near misses, property damage or health and safety issues that happen in the workplace.
Why is it important to write a work incident report?
As soon as an incident takes place and everybody in the workplace is safe, a work incident report should be written up.
What is a general staff accident report?
It includes all the necessities to describe a workplace incident to ensure it is recorded correctly. This general form is ideal for any business type.
Why should an accident report be signed?
The accident report should be signed to acknowledge that it is everything that the employee remembers happening. This workplace incident report template includes the basic guidelines and best practices of what to include to make sure the report includes all the details it should.
What form do you fill out to keep a log of an OSHA incident?
If this is an OSHA recordable incident (accident) and the company is exempt from OSHA recordkeeping, the employer must also fill in OSHA Form 300 . This form enables both the employer and the agency to keep a log of the injuries or illnesses that happen in the workplace.
What should be noted when a workplace vehicle is involved?
If a workplace vehicle was involved, all information about the vehicle should be noted, and the possible reasons why it occurred if there is no clear answer. Employers should ensure vehicle safety guidelines are adhered to in order to prevent incidents in the workplace.
Why is it important to record incidents?
In any case, it’s crucial to record any incidents that arise because this helps create a safer work environment.
What is incident report?
INCIDENT REPORTS. Function/Purpose. An incident report is not part of the patient’s chart, but it may be used later in litigation. A report has two functions: It informs the administration of the incident so management can prevent similar incidents in the future. It alerts administration and the facility’s insurance company to a potential claim ...
Who should report an incident?
Who Should Report. Only people who witness the incident should fill out and sign the incident report. Each witness should file a separate report. Once the report is filed, the nursing supervisor, department heads, administration, the facility’s attorney, and the insurance company may review it.
How long does it take for a supervisor to provide a copy of the Incident Report?
The supervisor shall provide a copy of the Incident Report and the Worker’s Compensation Report (if necessary) to the LHDs Safety Officer within five working days of the accident.
Why do you need to follow strict guidelines when completing an incident report?
Because incident reports will be read by many people and may even turn up in court, you must follow strict guidelines when completing them. If an incident report form does not leave enough space to fully describe an incident, attach an additional page of comments.
What is exposure incident?
Exposure Incidents: skin, eye, mucous membrane or parental contact with blood or other potentially infectious materials that may result from the performance of an employee’s duties. Accident, Injury: patient, visitor, employee slips or falls, or other incident, which results or may result in injury.
How to document an unusual occurrence?
Document any unusual occurrences that you witnessed. Record the events and the consequences for the patient in enough detail that administrators can decide whether or not to investigate further. Write objectively, avoiding opinions, judgments, conclusions, or assumptions about who or what caused the incident.
Who is responsible for preparing an incident report?
All employees are responsible for preparing an incident report as soon as possible and reporting immediately to their supervisor or in the supervisors absence report to the administration any incident or injury including near misses. Recommendations and appropriate changes shall be discussed with the supervisor and necessary corrections implemented to prevent further accidents.