Patient falls – What is your incident reporting process?
3 hours ago · A patient incident report, according to Berxi, is “an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.” Reports are typically completed by nurses or other licensed personnel. >> Go To The Portal
The mechanism for recording and reporting a patient fall will vary depending on the state and the in-house mechanism the healthcare facility uses. Generally, mishaps such as falls are recorded in an incident report. After the fall, a nurse and a medical provider will likely perform an examination of the patient and document their findings.
Full Answer
Should I file an incident report?
Generally, though, you should outline:
- What happened (detailed description of the incident, incident category/type)
- When it happened (date and time)
- Where it happened (be as specific as possible)
- How it happened (Are there any obvious root causes, like a puddle on the floor where an employee slipped)
- Who it happened to (employee name and title)
- Who reported it (Who is writing this document?)
What is a fall incident report?
The report states a landing zone was established along Charleston Highway and Murdaugh was airlifted to what SLED later revealed was Memorial Health University Medical Center in Savannah, Georgia. There, he was treated for a superficial gunshot wound to the head, according to SLED.
What is an example of an incident report?
If there is an injury, illness or damage as a result of the hazard, that is an incident and should be reported as such. For example… If no one changes a burned out lightbulb leading to dimly lit conditions in an area, that is a hazard.
What is a serious incident report?
ACCIDENT REPORT/SERIOUS INCIDENT REPORT [SIR] Use to convey flash traffic to the commander and command post relating to an accident or serious incident within the command. Use FLASH precedence on CMD nets. For all other stipulations and instructions refer to AR 190-40 (SIR) and AR 385-40 (Accident Report)

How do I write an incident report for fall?
How to Write an Incident Reportyour name and contact details;name and address of specific location of the incident;time and date of the incident;the names and contact details of those involved;the types of injuries and their severity;the names and contact details of witnesses;More items...
How do you write a patient incident report?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
How do you document a patient fall?
Start by asking the patient why they think the fall occurred and assess associated symptoms, and then check the patient's vital signs, cranial nerve, signs of skin trauma, consciousness and cognitive changes, and any other pain or points of tenderness that could have resulted from the fall.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What are the examples of incident?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
What should an incident report include?
8 Items to Include in Incident ReportsThe time and date the incident occurred. ... Where the incident occurred. ... A concise but complete description of the incident. ... A description of the damages that resulted. ... The names and contact information of all involved parties and witnesses. ... Pictures of the area and any property damage.More items...•
How would you describe a patient fall?
A patient fall is defined as an unplanned descent to the floor with or without injury to the patient. A fall may result in fractures, lacerations, or internal bleeding, leading to increased health care utilization. Research shows that close to one-third of falls can be prevented.
How should you respond if your client has a fall?
These may vary between hospitals and settings but will generally include actions such as:reassuring the patient.calling for assistance.checking for injury.providing treatment as indicated.assessing vital signs and neurological observations.notifying medical officer and nurse in charge.notifying next of kin.More items...•
What do nurses do if a patient falls?
It includes the following eight steps:Evaluate and monitor resident for 72 hours after the fall.Investigate fall circumstances.Record circumstances, resident outcome and staff response.FAX Alert to primary care provider.Implement immediate intervention within first 24 hours.Complete falls assessment.More items...
What are the 3 types of incidents?
3 Types of Incidents You Must Be Prepared to Deal WithMajor Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What is the process of incident report?
An Incident Reporting process is about capturing the details of an incident such as a safety incident, security, property damage, near miss or safety observation and submitting them to a nominated contact for follow up.
What are the different types of incident report?
Incident Report Checklist• Incident Report Template• Worker Incident Report• Accident Injury Report Template• Vehicle Incident Report• Near Miss Report• General Staff Incident Report Form• Incident Investigation Report• Vehicle Damage Report• Fire Incident Report• Event Incident Report FormMay 3, 2022
How Effective Are Incident-Reporting Systems for Improving Patient Safety?
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a...
When to Report an Incident to the Police?
The general rule of thumb is that an incident report should be completed as quickly as possible after an occurrence happens. Minor injuries should...
How Are Patient Safety Event Reporting Systems used?
Hospitals are replete with patient safety event reporting systems, which serve as a cornerstone of efforts to detect patient safety incidents and q...
How long after incident should you report a patient?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred. You may even want to file the report by the end of your shift to ensure you remember all the incident’s important details. RELATED: Near Miss Reporting: Why It’s Important.
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What are physiological falls?
Anticipated physiological falls are associated with patients that are confused, elderly with dementia or Alzheimer’s. For this population to minimize falls, bed alarms can be utilized but if the bed alarm is constantly going off then a bedside sitter needs to be available to sit with the patient because a nurse with high nurse patient ratio cannot always get to the room whenever a bed alarm rings. Accidental falls are associated with patient being tethered to Tubing’s, walking with IV pole, or tripping over cluttered room. For these patients, hourly rounding is best because every hour if a nursing team member goes in to check on the patient many falls can be reduced. Unanticipated physiological and behavioral falls are not preventable because in these situations any outcome is…
What should a nurse check before discharge?
According to Ruggiero, Smith, Copeland, and Boxer, before discharge, the nurse should check medications to “identify discrepancies, such as medication omission, duplication, change in frequency, change in dose, adjustments, new medications not accompanied by a prescription, or omission of core measures.” This is referred to as a discharge time out. If the nurse is not confident about medications, the nurse can ask a pharmacist to help. This discharge time out ensures that patients are discharged to home with the correct medications list (Ruggiero, Smith, Copeland, & Boxer, 2015). Success will be determined if the patient uses handrails and grab bars as needed, use an assistive device such as a walker correctly, clutter and spills from the floors, and correctly transfer while using safe transfer procedures. These procedures will keep the patient safe and prevent the patient from falling (Ackley & Ladwig,…
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
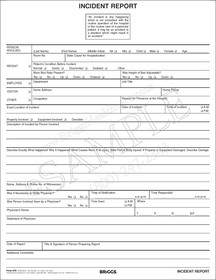
The way to complete the Fall incident report sample form on the internet
To start the form, use the Fill & Sign Online button or tick the preview image of the form.
Video instructions and help with filling out and completing Incident Report Patient Fall Sample Form
Find a suitable template on the Internet. Read all the field labels carefully. Start filling out the blanks according to the instructions:
Instructions and help about medical incident report form
you in this short a learning course the objective is to identify types of incidents determine what to do when those incidents occur document the incident in an incident report form contact supervisors or managers about the incident and follow through you may ask what is an incident well there are multiple things there patient complaints which can account for wait times communication issues difficult patience harassment of staff employee injuries such as Falls or needlesticks confidentiality HIPAA privacy and security medication errors including dosages incorrect meds a medical risk a harm to the patient perhaps even language barriers or theft stolen food or wallets why report incidents in the first place firstly it's to improve quality and also to discover trends and repeated occurrences of incidents plus it is mandated by accreditation agencies such as Jayco here is a sample incident report it's divided into three sections the patient or employee information the type of incident and t.
FAQs
Here is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Why are patient forms at hospitals such a pain to fill out?
Usually there is a one or maybe a two-page form. I don't think they are that difficult to fill out. They copy my insurance card and that's it. Generally they include a brief list of history questions and current symptom questions. If it is a current doctor, only the current symptom questions.
How do I fill out the Form 102 (ICAI) for an articleship? Can anyone provide a sample format?
Form 102 serves as a contract between you and your Principal at work. It becomes binding only when its Franked.Franking is nothing but converting it into a Non Judicial Paper. So u'll be filling in your name, your articleship period and other details and you and your boss (principal) will sign it on each page and at the end.
What tax forms do I need to fill out for reporting bitcoin gains and loses?
IRS1040 and 1099 forms.“For instance, there is no long-term capital gains tax to pay if you are in the lower two tax brackets (less than $36,900 single income or less than $73,800 married income).
Why do we need to write incident fall reports?
In such cases, we need to write incident fall reports so that we can take precautions for future such incidents. Some inconveniences can be damaging and cost a lot of lives.
How to write a fall report?
Step 1: Gather Facts. The first step in writing an incident fall report is to gather the real account of the whole incident. You need to gather all the facts of the events leading up to the incident. This will help you understand the reason behind the incident so that you can avoid the same in the future as well.
What should I do when I have a slip and fall incident?
When you engage in a slip and fall incident, then the first thing you need to do is write a report informing about the incident for the hospital staff so that they can treat you instantly. For the report, it’s always better to use incident report sample templates so that you don’t need to create the report from scratch and also get to include necessary information as required.
How to take pictures of a fall?
In a fall incident, taking pictures is the best evidence. Since it’s obvious that everyone has a smartphone with them, it’s wise to click immediate pictures of the incident instantly when you fall. Get pictures of your injury and immediately call for the doctor’s appointment. If the hazard is too much, you can ask someone else to click your picture.
Do you need to fill out a post fall incident report?
If you visit the hospital with an injury due to a massive fall, you are likely to fill out an incident report for safety. However, you can save time and get yourself checked instantly if you have this Post Fall Incident Report Form already with you. Get this on your device and use it when you encounter an accident so that you can immediately report and get a doctor’s appointment.
Should I write a report on a fall?
When you are injured due to a severe fall, it’s imperative you write a report on the incident so that you can inform the doctor as soon as possible. The longer you wait, the more chances are that your injury worsens. It’s better to be safe than sorry. Download this Fall Incident Report Form Template in PDF format and create such reports instantly. So no more waiting!
What Is a Nursing Incident Report?
A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side.
What Are the Information Needed in a Nursing Incident Report?
An incident report should be completed every time that an accident or any mishaps in giving care to the patient or any instances or possibilities of deviating from the normal operation and routine of the facility and/or from the patient.
What Is the Desired Outcome of Writing a Nursing Incident Report?
In writing an incident report a positive outcome should always be manifested but that depends on the event of the accident. There are times that the outcomes are deviated from what we expect and manifest. For pessimistic situations that will not happen in the future, a good, desired outcome must be manifested in writing a nursing incident report.
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Incidents happen from time to time. We cannot deny the fact that accidents of different kinds may occur or happen unexpectedly. Such cases may happen inside a hospital facility. It can happen in the operating room, wards, nurses’ station, laboratories, and even emergency rooms.
Purpose of a Nursing Incident Report
Nursing incident reports are used to initiate communication in sequencing events about the important safety information to the hospital administrators and keep them updated on aspects of patient care. Writing an incident report has its own purpose that will provide us a clearer understanding of how it works and how it is done.
How to Write a Nursing Incident Report
This is to confirm that an accident or incident has occurred that requires an incident report. Clinical reasoning and judgment must be possessed by a clinical health practitioner or any healthcare professional. It is a skill that is needed to be learned in a span of time.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes that need to be made in the facility or to facility processes to prevent recurrence of the incident and promote overall safety and quality of care.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
What is the third leading cause of death in the U.S.?
According to a 2016 study conducted by Johns Hopkins, medical errors have become the third-leading cause of death in the U.S. and threaten the safety and well-being of patients. As time-consuming as incident reports may be, their role in patient care cannot be ignored.