Reporting Patient Safety Events | PSNet
9 hours ago · Background and Significance. A patient safety event is defined as any process, act of omission, or commission that results in hazardous healthcare conditions and/or unintended harm to the patient [ 1].Reporting patient safety events is a useful approach for improving patient safety [ 2].The mechanism of event reporting was first introduced in the high-risk industries … >> Go To The Portal
As defined by Berxi, a patient incident report is “a detailed, written description of the chain of events leading up to and following an unforeseen scenario in a healthcare context,” which can be either computerized or paper-based. Nurses or other qualified professionals are often responsible for completing reports.
Full Answer
What are the most frequently reported events in electronic hospital event reporting?
Studies of electronic hospital event reporting systems generally show that medication errors and patient falls are among the most frequently reported events. Source: Milch CE, Salem DN, Pauker SG, Lundquist TG, Kumar S, Chen J. Voluntary electronic reporting of medical errors and adverse events.
How can we increase patient safety event reporting?
A major part of increasing patient safety event reporting comes down to simplifying the reporting process itself. The urgent nature of doctors’ and nurses’ jobs means stepping away isn’t always an option, leading them to overlook reporting.
What is the difference between patient safety event reporting and incident reporting?
Patient safety event reporting systems are ubiquitous in hospitals and are a mainstay of efforts to detect patient safety events and quality problems. Incident reporting is frequently used as a general term for all voluntary patient safety event reporting systems, which rely on those involved in events to provide detailed information.
What is a patient safety event?
A patient safety event is defined as any process, act of omission, or commission that results in hazardous healthcare conditions and/or unintended harm to the patient [ 1]. Reporting patient safety events is a useful approach for improving patient safety [ 2].
What is an event report healthcare?
The Event Reporting System (EVR) shall be used to report any occurrence that is not consistent with routine operations that may potentially or actually result in injury, harm, or loss to any patient or visitor at UCLA Health System and outpatient clinics.
How do you write an incident report on a patient?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What is a patient event?
Patient Safety Event – An event, incident, or condition that could have resulted or did result in harm to the patient and can be but is not necessarily the result of a defective system or process design, a system breakdown, equipment failure, or human error.
What is an example of a patient safety event?
A patient safety incident occurs but does not result in patient harm – for example a blood transfusion being given to the wrong patient but the patient was unharmed because the blood was compatible. or expected treatment – for example he/she did not receive his/her medications as ordered.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What are examples of incidents?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
What is a patient safety report?
Patient Safety Reporting (PSR) gives military treatment facility personnel the ability to anonymously report medical events that impact the safety of patients.
Why must a SI report be?
It is important that any incident suspected as a SI is notified to the Patient Safety Team as soon as possible. The notification ensures communication of incidents and the mobilisation of help and support. Even when it is decided an incident is not a SI the notification can be very valuable.
Why is safety event reporting important?
Despite its flaws, safety event reporting is an important tool for identifying system hazards and aggregate data, and sharing lessons within and across organizations. Systems can share known fail points in care, which allow other systems to identify that as a potential risk within their own organization.
What types of events should be reported in a safety report?
Events that affect staff safety should be reported as well. Staff can also report “near miss” or potential events, things that were caught before patients or family members were impacted but that could have been a problem if the staff had not noticed in time.
What should be documented in the safety event report for this patient?
Filling Out an Effective Incident Report Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected. Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient's physician.
What is the most common type of incident reporting event?
medication incidentsThe most common types were medication incidents (29%), falls (14%), operative incidents (15%) and miscellaneous incidents (16%); 59% seemed preventable and preventability was not clear for 32%. Among the potentially preventable incidents, 43% involved nurses, 16% physicians and 19% other types of providers.
How Effective Are Incident-Reporting Systems for Improving Patient Safety?
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a...
When to Report an Incident to the Police?
The general rule of thumb is that an incident report should be completed as quickly as possible after an occurrence happens. Minor injuries should...
How Are Patient Safety Event Reporting Systems used?
Hospitals are replete with patient safety event reporting systems, which serve as a cornerstone of efforts to detect patient safety incidents and q...
Streamline the Incident Reporting Process
Riskonnect’s Patient Safety Event Reporting software captures complete and accurate information with intuitive and accessible forms – and alerts the right people in real-time so issues can be swiftly addressed.
costly problems?
Download our e-book, A Guide to Using Root Cause Analysis, to get the what, why, when, and how of root cause analysis – and start digging deeper for better results.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
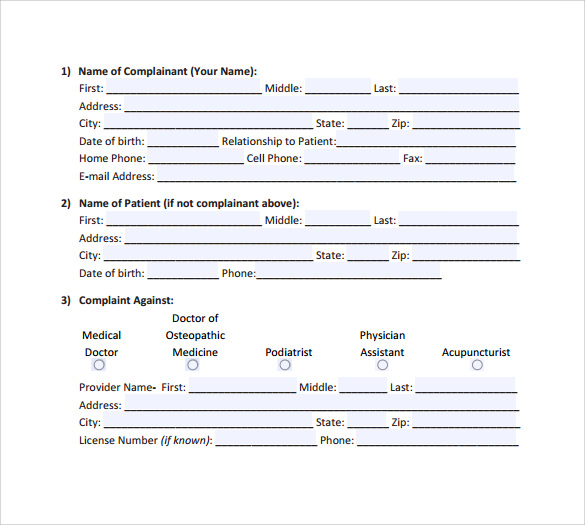
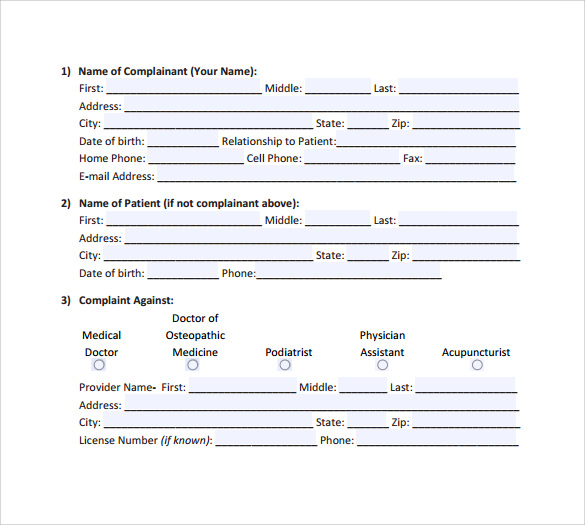
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
How to increase patient safety event reporting?
To increase patient safety event reporting, hospitals must be equally proactive after incidents are reported. This means alerting the necessary parties, strategically analyzing aggregated healthcare data and, finally, sharing the end results with staff. According to The Patient Safety Primer, however, many hospitals do none of the above. The error management study referenced above notes that “most hospitals surveyed did not have robust processes for analyzing and acting upon aggregated event reports” and only “20–21% [of hospitals] fully distribute and consider summary reports on identified events.”
What are adverse safety events?
Adverse safety events—some that lead to serious harm—occur every day, affecting people across entire health systems. With a full schedule of patients and life-or-death situations a part of daily life in hospitals, reporting efforts, not surprisingly, may end up taking a back seat. The ability to collect and analyze this data is crucial ...
How does Origami Risk work?
Origami Risk’s healthcare risk management software allows for reporting via an intranet portal on desktop or via mobile device. This allows staff to capture healthcare data when and where a patient safety event occurs, adding convenience and increasing accuracy. Furthermore, as stated in How to create a successful and sustainable near-miss culture, “The ability to input incident and near miss data while in the field can be a critical part of the process...Mobile reporting reduces lag time and helps investigations begin faster.” The sooner an incident gets reported, the sooner that data can lead to patient aid and organizational change.
What is the cultural shift in healthcare?
The EHS Today article The Risks of Using Injury and Illness Reporting as Measurements of Success says hospital leadership should reexamine their existing patient safety programs to make sure they’re not incentivizing non-reporting, prohibit retaliatory actions against staff who report incidents, and provide training to workplace leaders to communicate these compliance measures.
What is patient safety training?
As the Patient Safety Network states, such training “focuses on developing effective communication skills and a more cohesive environment among team members, and on creating an atmosphere in which all personnel feel comfortable speaking up when they suspect a problem.”.
Where is the Walkrounds clinic?
OSF St. Joseph Medical Center in Bloomington, Illinois, uses the WalkRounds™ concept, sending on-the-ground information directly to the highest levels of leadership for increased awareness and strategic planning.
Is patient safety event reporting bad?
The process of patient safety event reporting often carries a negative connotation. As former British Health Secretary Jeremy Hunt said at the 2018 World Patient Safety Summit in London, “People are terrified that if they're open about what happens, they...might get fired by their hospital, and it'll be bad for the reputation of their unit and their trust.”
Can summary of care records be faxed?
However, the other percentage of summary of care records could still be faxed. Under either circumstance, Promoting Interoperability does not fulfill new patient event notification CoP requirements.
Do post acute providers need an EHR?
Further, under Promoting Interoperability, CCDs are not necessarily sent to all post-acute providers, as a direct address is required to do so and some post-acute providers do not use an EHR that supports CCDs.
Characteristics of Incident Reporting Systems
- An effective event reporting system should have four key attributes: While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic …
Limitations of Event Reporting
- The limitations of voluntary event reporting systems have been well documented. Event reports are subject to selection bias due to their voluntary nature. Compared with medical record review and direct observation, event reports capture only a fraction of events and may not reliably identify serious events. The spectrum of reported events is limited, in part due to the fact that ph…
Using Event Reports to Improve Safety
- A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require furth…
Current Context
- At the national level, regulations implementing the Patient Safety and Quality Improvement Act became effective on January 19, 2009. The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to wo…