Primary autoimmune myelofibrosis: a case report and …
14 hours ago · Mr M confirms experiencing mild dyspnea with exertion. He has noticed occasional night sweating, bone pain, and despite reporting a decreased appetite, he reports a … >> Go To The Portal
CASE REPORT We present the case of a 66-year-old man with a history of myelofibrosis, medicated with ruxolitinib and darbepoetin, and allopurinol since 2016, with good disease control. In July 2019, he reported to a hematology appointment, complaining of occasional night sweats, nausea, and general malaise, which had worsened in the previous week.
Full Answer
How many cases of myelofibrosis are there?
Myelofibrosis is a rare condition, with about 1.5 cases reported per 100,000 people each year in the United States. It occurs in both men and women. People of any age can have myelofibrosis, although it is more likely to be diagnosed in people over age 50.
What is the main problem in myelofibrosis?
Myelofibrosis causes extensive scarring in your bone marrow, leading to severe anemia that can cause weakness and fatigue. Bone marrow scarring can also cause you to have a low number of blood-clotting cells called platelets, which increases the risk of bleeding. Myelofibrosis often causes an enlarged spleen.
What is the most common presenting symptom of myelofibrosis?
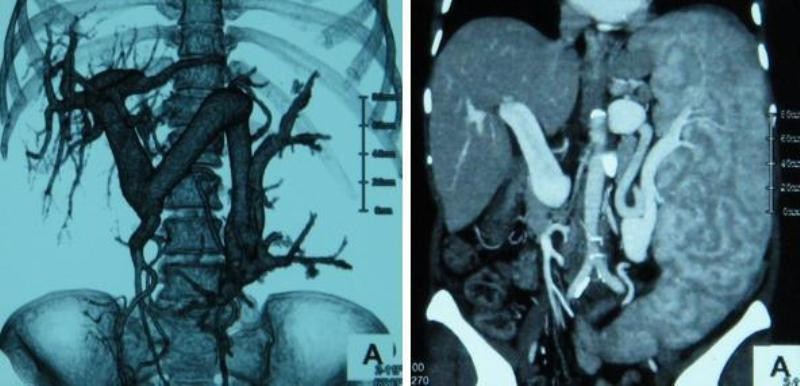
Splenomegaly is the most common finding in patients with primary myelofibrosis, and it is present in approximately 90% of patients. Spleen size may vary from barely palpable to massive (observed in 35% of patients).
What is the life expectancy of someone with myelofibrosis?
Transcript:Srdan Verstovsek, MD, PhD: Myelofibrosis is one of the myeloproliferative neoplasms, a chronic disease of the bone marrow. It is, unfortunately, the aggressive type. It does affect the life expectancy of the patients. The average survival is about 5 to 7 years.
What is the best treatment for myelofibrosis?
The goal of treatment for most people with myelofibrosis is to provide relief from signs and symptoms of the disease. For some, a bone marrow transplant may provide a chance for a cure, but this treatment is very hard on the body and it might not be an option for many people.
What causes death in myelofibrosis?
The common causes of death in patients with primary myelofibrosis are infections, hemorrhage, cardiac failure, postsplenectomy mortality, and transformation into acute leukemia. Leukemic transformation occurs in approximately 20% of patients with primary myelofibrosis within the first 10 years.
How long can you take jakafi?
Jakafi is a long-term treatment. Your Healthcare Professional may allow up to 6 months to see if Jakafi is working for you. If you do not see an improvement after 6 months of treatment, your Healthcare Professional may have you stop taking Jakafi.
Does myelofibrosis cause bone pain?
Myelofibrosis can cause your bone marrow to harden. When that happens, the connective tissues that surround your bones become inflamed. The result: achy or tender bones and joint tenderness.
Can myelofibrosis be cured?
There are currently no medications that cure myelofibrosis. Allogeneic hematopoietic stem cell transplantation is the only treatment that may cure MF or significantly prolong the survival of people with MF.
Can you live 20 years with myelofibrosis?
Results from a retrospective study suggest that identification of patients with primary myelofibrosis likely to survive 20+ years can be made on the basis of age, sex, blood counts, and symptoms, without inclusion of genetic risk factors. This study was published in the American Journal of Hematology.
Can you live a long life with myelofibrosis?
Life expectancy in PMF Primary myelofibrosis, also known as idiopathic myelofibrosis or myelofibrosis with myeloid metaplasia, is a rare disease19, 20 usually affecting elderly people. Median survival ranges from 4 to 5.5 years in modern series6, 7, 8, 9, 10, 11, 12, 13, 14 (Figure 1).
What is new in myelofibrosis?
A drug used to treat certain advanced breast cancers may offer a new treatment option for a deadly blood cancer known as myelofibrosis, new research from UVA Cancer Center suggests. The drug, palbociclib, may be able to prevent the scarring of bone marrow that existing treatments for myelofibrosis cannot.
Is myelofibrosis life threatening?
Myelofibrosis is uncommon, but potentially deadly if left untreated. Normally, your bone marrow produces all kinds of blood cells. Myelofibrosis (MF) disrupts this process and causes the marrow to produce scar tissue instead of vital cells.
Can myelofibrosis affect the brain?
Can Myelofibrosis Affect the Brain? Myelofibrosis can occur anywhere in the body, and tumors can develop elsewhere in your body, such as the lymph nodes, spinal cord, and lungs. Since these tumors cannot be eliminated from the body, they affect the brain.
Why does the spleen enlarged in myelofibrosis?
People with MF have a bone marrow problem. Bone marrow is where blood cells are primarily made. When the bone marrow can't make enough normal cells, the spleen helps out by starting to produce them. This causes the spleen to grow larger.
Can myelofibrosis spread?
These faulty genes make copies of themselves. The bad versions spread through your body and make the cells that lead to inflammation in your marrow.
What is primary myelofibrosis?
Introduction : Primary myelofibrosis is a disease of middle aged and elderly patients. Both sexes are equally affected. Patient present with weight loss, night sweats, anorexia, fatigue or lump in left hypochondrium (due to splenomegaly). Some patients also present with gout and renal colic manifestations. Petechiae, echymoses and lymphadenopathy may present in few patients. All patients have anemia with Hb < 10gm/dl and it demonstrates anisopoikilocytosis with tear drop cells. There is also “leucoerythroblastic reaction” with presence of nucleated red cells along with myelocytes and metamyelocytes in peripheral smear. Initially platelet count is high and it decreases at the terminal stage. WBC count is higher in the range of 15- 30×109/L with shift to left and sometimes leucopenia is present in terminal stage. NAP score is markedly increased and serum LDH level is also high. In 2016, prefibrotic primary myelofibrosis was formally classified as a distinct condition that progresses to overt PMF in many patients, the primary diagnostic difference being the grade of fibrosis. (1)
What is prefibrotic stage?
Prefibrotic stage is characterized by mild normocytic anemia with poikilocytosis, tear drop cells, nucleated rbcs, thrombocytosis and mild leukocytosis with some immature forms . The marrow is hypercellular and contains abnormal megakaryocytes which clusters around sinuses and trabeculae. Bonemarrow shows atypical, enlarged and immature megakaryocytes with cloud like immature nuclei and small megakaryocytes. Intrasinusoidal hematopoiesis is often present. (3) Diagnostic criteria for primary myelofibrosis, prefibrotic / early stage: must meet all 3 major criteria plus at least
Popular Posts:
- 1. rappahannock health connect patient portal login
- 2. dr shannon berry patient portal templeton ca
- 3. patient co account login
- 4. yuma regional patient portal
- 5. dme patient portal
- 6. optomitrists with patient portal
- 7. marin genreal patient portal
- 8. patient portal kiosk
- 9. patient portal urology group og
- 10. how to report about a patient in post conference of psychiatric unit