How to Document a Patient Assessment (SOAP) - Geeky Medics
27 hours ago Choose 4 - Opens eyes spontaneously 3 - Opens eyes in response to voice 2 - Opens eyes in response to pain 1 - Does not open eyes. Verbal Response. Choose 5 - Oriented, converses normally 4 - Confused, disoriented 3 - Words, but not coherent 2 - Sounds, but no words 1 - Makes no sounds. Motor Response. >> Go To The Portal
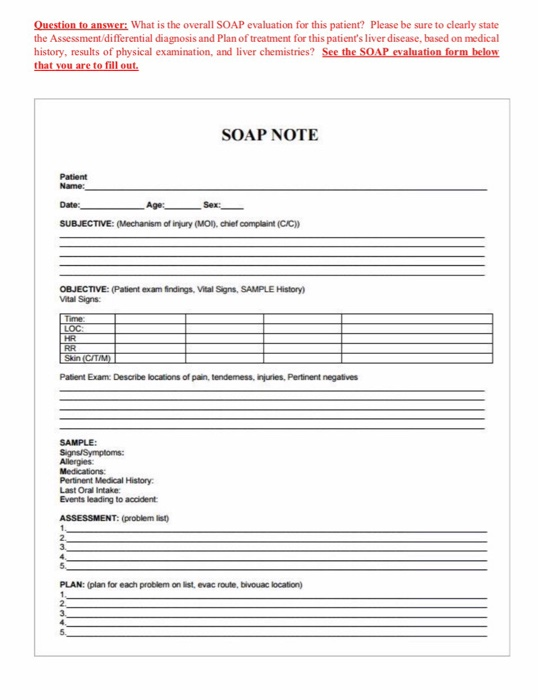
A SOAP (s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers. SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way.
Full Answer
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What is a SOAP note in Aha?
A well-completed SOAP note is a useful reference point within a patient’s health record. Like BIRP notes, the SOAP format itself is a useful checklist for clinicians while documenting a patient’s therapeutic progress. [2]
What are therapy SOAP notes and why are they important?
As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions. Importantly, therapy SOAP notes include vital information on a patient’s health status.
Do you need a SOAP note for your medical practice?
Some medical practices may want the fully-written SOAP note to be reviewed and/or approved by a higher-up, while some practices will want the SOAP note writer to upload the completed document to a database of medical records. Or, the best plan of action may be to carry out the action tasks in the plan as soon as possible.
What is the soap method in healthcare?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What does SOAP stand for and where is it used in a patient care report?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
How do you write the assessment part of a SOAP note?
SOAP Note TemplateDocument patient information such as complaint, symptoms and medical history.Take photos of identified problems in performing clinical observations.Conduct an assessment based on the patient information provided on the subjective and objective sections.Create a treatment plan.More items...•
How do you write a SOAP note for nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo stands for subjective objective assessment and plan let's take a look at each of the fourMoreSo stands for subjective objective assessment and plan let's take a look at each of the four components. So you can understand this neat and organized way of note-taking.
What is assessment in SOAP notes?
SOAP is an acronym for: Subjective - What the patient says about the problem / intervention. Objective - The therapists objective observations and treatment interventions (e.g. ROM, Outcome Measures) Assessment - The therapists analysis of the various components of the assessment.
What is soap stand for?
Subjective, Objective, Assessment, and PlanHowever, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
Why do we use SOAP notes?
Generally, SOAP notes are used as a template to guide the information that physicians add to a patient's EMR. Prehospital care providers such as emergency medical technicians may use the same format to communicate patient information to emergency department clinicians.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What is soap charting in nursing?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
How do you review a patient?
Reviewing patients on callThe importance of reviewing patients. ... Ask for the basics while youre on your way. ... Make a rapid initial assessment. ... Look at the observations chart. ... Review the notes. ... Take a focused history. ... A full and formal examination. ... Putting it all together.More items...•
Why doesn't a medical soap note contain all the details?
Because it doesn’t contain all the details a medical SOAP would usually have, including the patient’s race, age, gender, and initial information about the chief complaint. This is because those details were most likely already written about in a previous SOAP note.
Why do we use soap notes?
SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records. To see what a SOAP note template looks like, check out (and use!) this example from Process Street: ...
What is a soap note template?
The SOAP Note Template is a documentation method used by medical practitioners to assess a patient's condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information.
What is the history of the soap note?
The SOAP note isn’t some made-up mumbo-jumbo; rather, it has a long history rooted in the need to solve complex real-life problems faced by real-life practicing physicians on a day-to-day basis. Here’s a short history lesson for you.
Can POMR change the multiplicity of problems that physicians face?
The POMR cannot change the multiplicity of problems that physicians face. But the POMR enables a highly organized approach to that complexity.”. – Dr. Lawrence Weed, Interview with Lawrence Weed, MD: The Father of the Problem-Oriented Medical Record Looks Ahead.
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
What is a soap note?
An effective SOAP note is a useful reference point in a patient’s health record, helping improve patient satisfaction and quality of care.
What is a soap progress note?
SOAP is an acronym for the 4 sections, or headings, that each progress note contains: Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
What is the purpose of a detailed assessment?
A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and. Plan: Where future actions are outlined.
Is soap a subjective or unbiased?
Unbiased: In the Subjective section, particularly, there is little need for practitioners to use weighty statements, overly positive, negative, or otherwise judgmental language. SOAP notes are frequently used both as legal documents and in insurance claims.
What does soap stand for in nursing notes?
SOAP notes are a way for nurses to organize information about patients. SOAP stands for subjective, objective, assessment and plan.
What is an A in nursing?
A is for analysis or assessment. Nurses make assumptions about what is going on with the patients based on the information they obtained. Although these assessments are not the medical diagnosis that health care providers make, they still identify important problems or issues that need to be addressed.
What does S mean in medical terms?
S is for subjective, or what the patients say about their situation. It includes a patient's complaints, sensations or concerns. In most cases, it is the reason the patient came to see the doctor. Here are some examples: The patient complained of a severe pain on the right side of his head.
Why are soap notes still used?
SOAP notes have been around for some time now and because of their efficiency and functionality, they are still being used now. The very first SOAP note template was created and developed by a brilliant doctor named Lawrence Weed way back in the 1960s. It was done at the University of Vermont as an element of the POMR (Problem-Oriented Medical Record). During those times, objective documentation did not exist so physicians had the tendency to make decisions about treating patients without scientific basis.
What is a soap note?
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data. Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors. Using these kinds of notes allows the main health care provider ...
What is a soap note template?
A SOAP note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. A SOAP note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
What is the oldest method of documentation?
Written and narrative notes are the oldest and most enduring method for documentation so chances are, the majority of health professionals are familiar with them. Though there are different formats for documentation, SOAP notes are the most organized, structured and easy to understand.
What is the purpose of assessment?
The main purpose of the patient’s medical visit is to seek treatment and so the assessment should contain all the symptoms stated by the patient along with the diagnosis of the illness or injury.
What is a soap note?
SOAP notes are easy to use and designed to communicate the most relevant information about the individual. They can also provide documentation of progress. For clinical professionals, SOAP notes offer a clear, concise picture of where the client is at the time of each session.
What is the S part of a client's notes?
Symptoms are what the person tells you is going on physically, psychologically, and emotionally. They are the client’s subjective opinion and should be included in the “S” part of your notes. Signs are objective information related to the symptoms the client expressed and are included in the “O” section of your notes.
Why is documenting important in healthcare?
Documentation protects the medical and therapeutic professionals while also helping the client. Clear notes communicate all necessary information about the patient or client to all of the people involved in the person’s care. SOAP notes facilitate the coordination and continuity of care.
What is a plan in healthcare?
A plan is where the rubber meets the road. Working with the client or patient, the clinician creates a plan going forward. The plan might include additional testing, medications, and the implementation of various activities (e.g., counseling, therapy, dietary and exercise changes, meditation.)
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
