10+ Patient Care Report Examples [ EMS, EMT, …
23 hours ago How to Write a Patient Care Report? 1. Be More Specific Than Just Being General One thing you may take notice of or the first thing that you may take notice... 2. Fill Out the Correct Details If your report is mostly like that of a checklist or a fill in the blanks type, remember... 3. Write the ... >> Go To The Portal
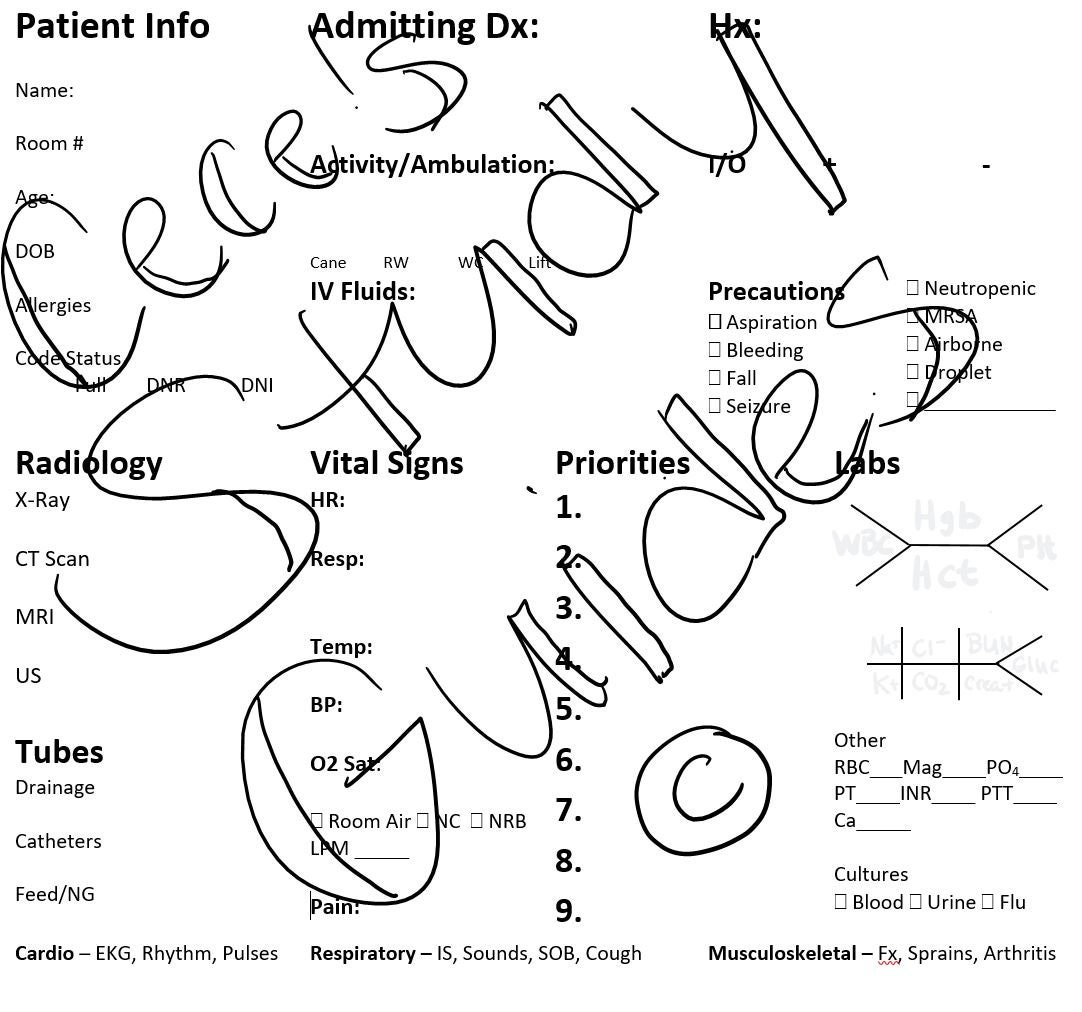
How to Write a Patient Care Report?
- Be More Specific Than Just Being General One thing you may take notice of or the first thing that you may take notice...
- Fill Out the Correct Details If your report is mostly like that of a checklist or a fill in the blanks type, remember...
- Write the Report Once the Call Is Made After you get the call it is always best to...
- Dispatch & Response Summary. ...
- Scene Summary. ...
- HPI/Physical Exam. ...
- Interventions. ...
- Status Change. ...
- Safety Summary. ...
- Disposition.
What does a patient care report consist of?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care. What should not be written in a patient care report?
Does your organization have poorly written patient care reports?
If your organization has been plagued with poorly written patient care reports the organization could be in poor financial health. This is especially important with the implementation of ICD-10 coding. Here is a checklist of questions EMS providers should answer before submitting a patient care report (PCR): Are your descriptions detailed enough?
Who can write reports in healthcare?
A lot of people believe that only nurses or health care workers can write reports. Most specifically patient care reports or anything that may be related to an incident report that often happens in hospitals or in some health care facilities.
What is the file size of the patient report form?
File Format DOC Size: 581 KB Download Patient’s Adverse Event Report Form astrazeneca.com Details File Format PDF Size: 1 MB Download Request for Patient’s Medical Report Form ha.org.hk Details File Format PDF Size: 234 KB Download The Parts of Patient Report Forms
What is a PCR in writing?
The PARCC Summative Assessments in Grades 3-11 will measure writing using three prose constructed response (PCR) items. In the classroom writing can take many forms, including both informal and formal.
What is the primary purpose of a patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool.
How do you write a PCR narrative in EMS?
The following five easy tips can help you write a better PCR:Be specific. ... Paint a picture of the call. ... Do not fall into checkbox laziness. ... Complete the PCR as soon as possible after a call. ... Proofread, proofread, proofread.
Why should a patient care report be detailed?
Importance of Documentation The purpose of record documentation is to provide an accurate, comprehensive permanent record of each patient's condition and the treatment rendered, as well as serving as a data collection tool.
What should a patient care report include?
What Patient Care Reports Should IncludePresenting medical condition and narrative.Past medical history.Current medications.Clinical signs and mechanism of injury.Presumptive diagnosis and treatments administered.Patient demographics.Dates and time stamps.Signatures of EMS personnel and patient.More items...•
What is patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool. The documentation included on the PCR provides vital information, which is necessary for continued care at the hospital.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What is EMS CHART?
CHART stands for Chief Complaint History Assessment Received Treatment Transfer of Care (Emergency Medical Care Narrative for Reporting) Suggest new definition.
What is a component of the narrative section of a patient care report?
The narrative section of the PCR needs to include the following information: Time of events. Assessment findings. emergency medical care provided. changes in the patient after treatment.
How do you write a health care report?
Tips on Writing a Report on Health Care Quality for ConsumersWhy Good Writing Matters.Tip 1. Write Text That's Easy for Your Audience To Understand.Tip 2. Be Concise and Well-Organized.Tip 3. Make It Easy to Skim.Tip 4. Use Devices That Engage Your Readers.Tip 5. Make the Report Culturally Appropriate.Tip 6. ... Tip 7.More items...
How do you take care of a patient report?
Document the patient's history completely. Remember bystanders or those close to the patient can often provide valuable information about the patient....Check descriptions. ... Check (and recheck) spelling and grammar. ... Assess your chief complaint description. ... Review your impressions. ... Check the final details.
What is soap EMT?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What is the purpose of the narrative section of the patient care report?
Detailed explanation of medical necessity: Your narrative should be detailed and provide a clear explanation for why the patient needed to be transported by ambulance. Include what the medical reasons were that prevented the patient from being transported by any other means.
What is the purpose of the American Hospital Association patient Care Partnership?
Our goal is for you and your family to have the same care and attention we would want for our families and ourselves. The sections explain some of the basics about how you can expect to be treated during your hospital stay. They also cover what we will need from you to care for you better.
What is a component of the narrative section of a patient care report?
The narrative section of the PCR needs to include the following information: Time of events. Assessment findings. emergency medical care provided. changes in the patient after treatment.
What is the purpose of Nemsis quizlet?
The National Emergency Medical Services Information System (NEMSIS): collects relevant data from each state and uses it for research. When a competent adult patient refuses medical care, it is MOST important for the paramedic to: ensure that the patient is well informed about the situation at hand.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
What questions should I ask a provider?
Here is a checklist of questions providers should answer before submitting a report: 1 Are your descriptions detailed enough? 2 Are the abbreviations you used appropriate and professional? 3 Is your report free of grammar and spelling errors? 4 Is it legible? 5 Is the chief complaint correct? 6 Is your impression specific enough? 7 Are all other details in order?
Can a report be inaccurate without proper English?
Your report should paint a picture, but this is impossible to do without proper English. Besides not being accurate or professional, incorrect English may very well lead a reader to believe something false. For example, there may be confusion (and laughter) if a report says “patient fainted and her eyes rolled around the room.” Though this is a humorous example, dire consequence can follow confusing reporting.
What is PCR in ambulance?
This includes a detailed assessment of the situation and a full recounting of the treatment administered to the patient. It is specific, informative, free of ambiguity and negligence. But yet, after all extensive training, the best some medics can do in the detailed assessment is to write "patient has pain to the arm."
What is an impression in medical terms?
An impression encompasses the reasons for patient treatment. Trauma and fall are too vague to be used as impressions. Include the body areas or symptoms that are being treated. In other words, what treatment protocol is being followed?
What is a chief complaint?
Chief complaint is not the cause of the injury. For example, a chief complaint is pain to the right lower arm, not the fact that the patient has fallen off a ladder. Using the patient’s own words is an appropriate practice if they describe symptoms of their chief complaint. 5. Review your patient impressions.
Why do you write PCR when you call?
Writing the PCR as soon as the call is over helps because the call is still fresh in your mind . This will help you to better describe the scene and the condition the patient was in during your call.
What should a PCR tell?
The PCR should tell a story; the reader should be able to imagine themselves on the scene of the call.
What is PCR in healthcare?
The PCR must paint a picture of what happened during a call. The PCR serves: 1 As a medical record for the patient, 2 As a legal record for the events that took place on the call, and 3 To ensure quality patient care across the service.
Why is PCR important?
A complete and accurate PCR is essential for obtaining proper reimbursement for our ambulance service, and helps pay the bills, keeps the lights on and the wheels turning. The following five easy tips can help you write a better PCR: 1. Be specific.
How long does it take to complete a PCR?
Most states, and many EMS agencies themselves, often have time limits within which the PCR must be completed after the call ended – 24, 48 or 72 hours are common time limits.
Why is an IV established on the patient?
This specifically explains why an IV was established on the patient and states facts that can be used to show medical necessity for the call. The same can be said for non-emergency transports between two hospitals. Simply documenting that the patient was transported for a “higher level of care” is not good enough.
How to determine if a medical necessity is met?
A primary way to determine if medical necessity requirements are met is with documentation that specifically states why you took the actions you did on a call. For example, simply documenting “per protocol” as the reason why an IV was started or the patient was placed on a cardiac monitor is not enough.
What Do Patient Reports Look Like?
In order to write patient case reports, the content is divided into five elements: the abstract, an introduction that will contain a written review, a description of that review, a discussion entitled “Why does the literature review matter?”, a summary about how it may relate and finally conclusion.”.
What Is Pcr In Medical Billing?
An PCR document serves as a summary of an individual’s permanent medical record as well as one that documents the event they’re having. It constitutes the basis for medical billing claims.
Why Is It Important To Write A Good Patient Care Report?
It’s crucial to accurately reflect this level of patient care, regardless of how well it’s delivered. Likewise, in receiving facilities, good written guidelines may serve as guides for what treatment or treatment plans are to follow for patients previously received.
What Is The Purpose Of Patient Care?
Health outcomes can very well be affected if quality patient care is given. People suffering from illnesses such as cancer are more likely to experience higher levels of depression and improved health outcomes when offered this service.
How Do You Write A Good Patient Care Report Part 2?
Make sure the terms you use are clear. Use neutral words and phrases like “weakness” and “fall” or “transport for high-level care in your nursing communication. These terms don’t provide an accurate picture of the signs and symptoms in the patient at the time of transportation, so aim to be as specific as possible.
What Should Be Included In A Patient Report?
It is proposed that the document include elements of background information, medical records, physical examinations, specimens obtained, treatment options and opinions.
Watch what is a patient care report Video
What Intervention Demonstrates The Integration Of Patient Centered Care?
Thanks for joining us!
Today marks the first in our Documentation 101 blog series. Using the next several blog postings, we’ll be attempting to put together a few coaching blogs to help all of you become better EMS documenters.
Maybe you need some basic writing help?
There’s nothing wrong in admitting that you need help. You can even better yourself, personally, by learning to communicate in writing more effectively. There are tons of self-help tools on the Internet to assist you with writing and grammar skills.
To the Rescue!
We’re not finished. As part of this documentation series, we’ll include some specific steps to make you a better documenter. Make your goal to be the best documenter that your department has and you’re well on your way to PCR writing success.
Not a client?
No problem there. Check out our website right now and complete the “Get Started” section so we can connect. We’d love to talk to you about the many features and how they can benefit your EMS Department!
What is the best thing about documenting signs and symptoms?
The great thing about documenting Signs and Symptoms is that it all has a lot to do with the numbers. In this case, you are recording your findings which are obtained by the skills you’ve developed for assessing things about the patient that, by and large, you can measure.
What is the Glasgow Coma Scale?
Another very important quantitative resource we use and record from the field is the Glasgow Coma Scale. The GSC is a simple means of documenting the patient’s overall status using the three criteria that makes up the GCS.
Why are patient reports important?
Why Patient Reports Are Needed. Patient medical reports serve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not.
What is the relevant information needed for a patient complaint?
In a patient complaint, the relevant information that are needed are as follows: The description of the situation. The effect on privacy.
What is healthcare personnel?
Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results). It goes without saying that everyone wants an accurate general information ...
What to do if you happen to be a relative of an injured person?
As the relative. If in case that you happened to be a relative of the injured person, the first thing to do is to calm down.
Do hospitals keep records of patients?
Therefore, it is mandatory that the medical clinic, center, or hospital keeps a record of their patients. These patient reports also help the doctors and the relatives of the patient to know what is or are behind the patients’ results of their individual health assessment.
Can results from medical assessments be given due to deficiency of relevant information?
Otherwise, results from medical assessments cannot be given due to deficiency of relevant information.
Check Descriptions
- Upon the completion of every ambulance call, a PCR documents all events that occurred. This includes a detailed assessment of the situation and a full recounting of the treatment administered to the patient. It is specific, informative, free of ambiguity and negligence. But yet, after all extensive training, the best some medics can do in the detailed assessment is to write "…
Review Abbreviations
- I have observed a steady degradation of the communication skills in my friends, family and coworkers since the introduction of instant digital communication. We have reduced the English language to acronyms, blurbs and gibberish. This type of language does not have a place in a PCR. Adding to this communication degeneration is the misuse of medical abbreviations in PCR…
Check (and Recheck) Spelling and Grammar
- Your PCR should paint a picture, but this is impossible to do without proper English. Besides not being accurate or professional, incorrect English may very well lead a reader to believe something false. For example, there may be confusion (and laughter) if a PCR says "patient fainted and her eyes rolled around the room." Though this is a humorous ...
Assess Your Chief Complaint Description
- An area of the PCR that is frequently misused is the chief complaint which should explain why you were called to the scene or why the patient is being treated. Chief complaint is not the cause of the injury. For example, a chief complaint is pain to the right lower arm, not the fact that the patient has fallen off a ladder. Using the patient’s own words is an appropriate practice if they de…
Review Your Patient Impressions
- An impression encompasses the reasons for patient treatment. Trauma and fall are too vague to be used as impressions. Include the body areas or symptoms that are being treated. In other words, what treatment protocol is being followed? If you are following a head injury protocol, and your assessment indicates a possible head injury, this should be included in your impression. M…
Check The Final Details of The PCR
- With the implementation of a more detailed ICD-10 coding, the patient’s past medical history and medications are important to note. Avoid writing "history on file." Document the patient's history completely. Hospital providers use this information if the history could affect the patient’s outcome. Another important aspect to clearly document is the outcome of your treatments. So…
Be Specific
Paint A Picture of The Call
- The PCR must paint a picture of what happened during a call. The PCR serves: 1. As a medical record for the patient, 2. As a legal record for the events that took place on the call, and 3. To ensure quality patient care across the service. PCRs should go beyond merely stating that a patient was picked up at a certain location, transported to anothe...
Do Not Fall Into Checkbox Laziness
- EMS professionals have long been promised a PCR that basically writes itself. Electronic PCR softwareis a great tool and can improve the efficiency of PCR completion. However, simply clicking a box or making a selection from a drop-down menu cannot be a substitute for your words in the form of a clear, concise, accurate and descriptive clinical narrative. An EMS provide…
Complete The PCR as Soon as Possible After A Call
- Most states, and many EMS agencies themselves, often have time limits within which the PCR must be completed after the call ended – 24, 48 or 72 hours are common time limits. While it is always important to comply with time limits, there are benefits to getting your PCR completed as soon as possible – preferably right after the call is completed and before your shift ends. In a pe…
proofread, proofread, Proofread
- The easiest way to improve your PCR is to proofread before submitting it. We understand the dilemma, after writing the sixth PCR for the day, and having 10 minutes left in the shift, the last thing anyone wants to do is sit there and reread what they have just written. But that is exactly what needs to be done. Poor grammar and spelling is the easiest way to have your abilities calle…