40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
2 hours ago · S: Patient reported difficulties in home care, in particular cleaning and shopping. She expressed concern of putting strain on her son who is her primary caregiver. She is keen to get back to previous roles within home (mother/housewife) and visit friends. O: Patient was polite and joking throughout the exam. She required assistant with getting on and off the exam table. >> Go To The Portal
SOAP Note Example: Subjective: Patient states: “My throat is sore. My body hurts and I have a fever.
Full Answer
How to document a patient assessment (soap)?
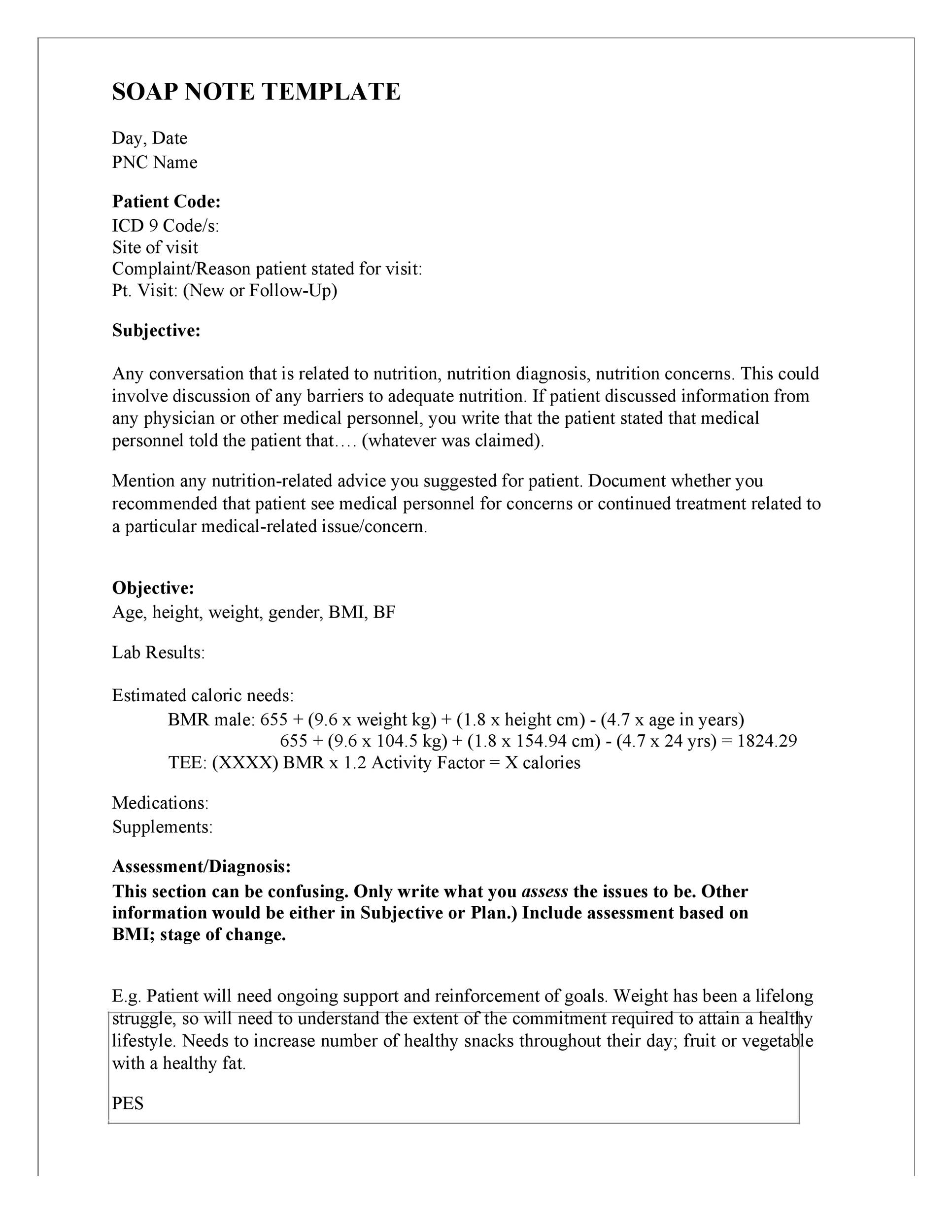
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What is a patient care report?
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.
Who can write reports in healthcare?
A lot of people believe that only nurses or health care workers can write reports. Most specifically patient care reports or anything that may be related to an incident report that often happens in hospitals or in some health care facilities.
What is a SOAP note used for in healthcare?
What is a SOAP Note? A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What should be included in a SOAP note assessment?
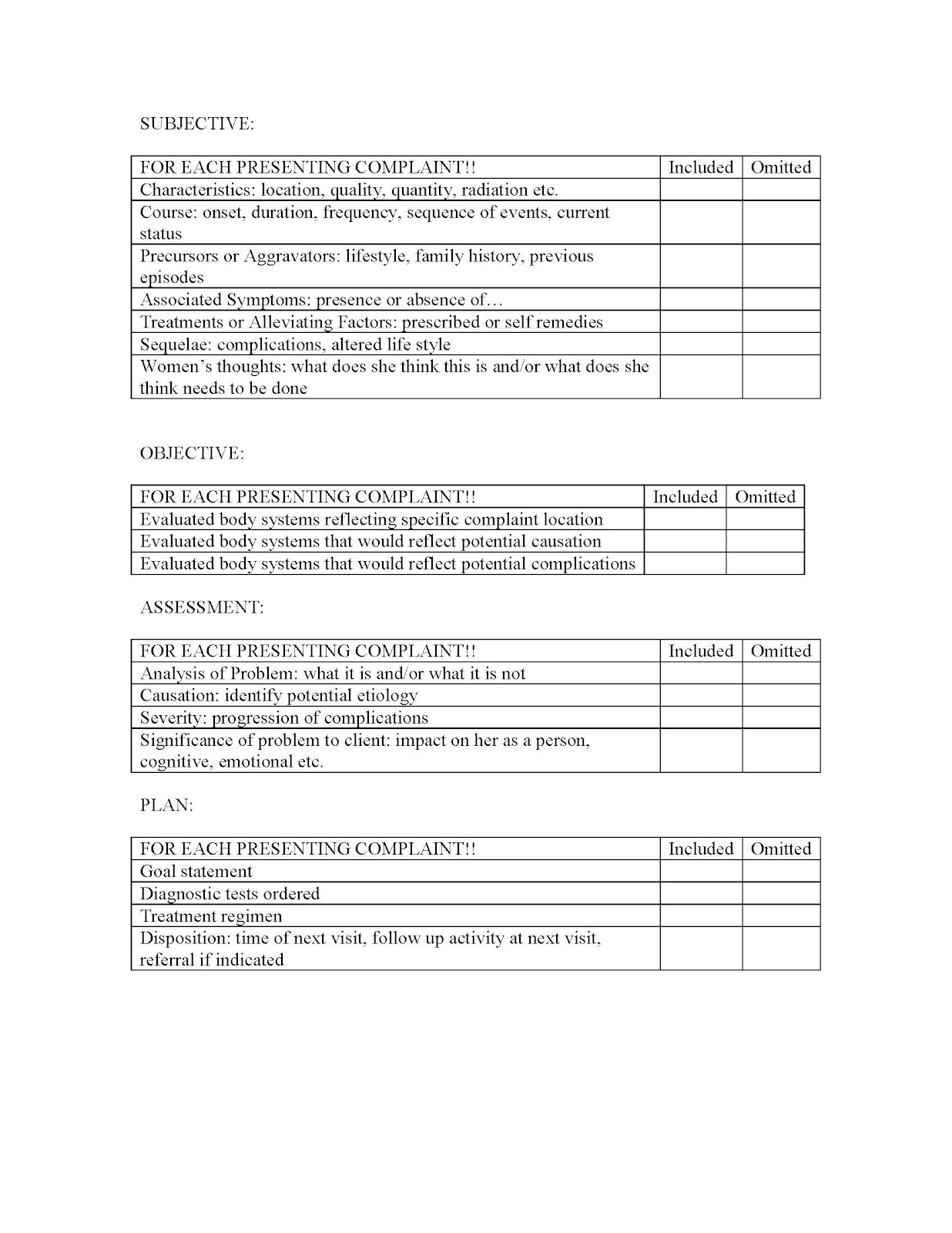
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What are the 4 parts of a soap evaluation?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan.
How do you write a SOAP note for nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo stands for subjective objective assessment and plan let's take a look at each of the fourMoreSo stands for subjective objective assessment and plan let's take a look at each of the four components. So you can understand this neat and organized way of note-taking.
How do you write a clinical SOAP note?
The Plan section of your SOAP notes should contain information on:The treatment administered in today's session and your rationale for administering it.The client's immediate response to the treatment.When the patient is scheduled to return.Any instructions you gave the client.More items...•
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What is SOAP note format?
The SOAP format – Subjective, Objective, Assessment, Plan – is a commonly used approach to. documenting clinical progress. The elements of a SOAP note are: • Subjective (S): Includes information provided by the member regarding his/her experience and. perceptions about symptoms, needs and progress toward goals.
What is the soap format in a medical record?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
What are three examples of subjective information that can be used during SOAP documentation?
This includes information the patient reports to you verbally (for example, their SYMPTOMS) or information their family shares with you. Other examples of subjective content include: How they are feeling (including their level of pain, level of fatigue, general sense of well-being or illness, etc.)
What is a nurse SOAP note?
Nurses and other healthcare providers use the SOAP note as a documentation method to write out notes in the patient's chart. SOAP stands for subjective, objective, assessment, and plan. Let's take a look at each of the four components so you can understand this neat and organized way of note-taking.
What is objective in SOAP notes?
Objective means that it is measurable and observable. In this section, you will report anything you and the client did; scores for screenings, evaluations, and assessments; and anything you observed. The O section is for facts and data.
What is a focused SOAP note?
the SOAP note or progress note. These terms are sometimes used interchangeably. As this is a more focused record than the complete history and physical documentation, what is recorded is often limited to what is pertinent to the current problem or problems.
What is a soap note?
A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication ...
What is the best software to collect SOAP notes?
Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. Collect photo evidence for a more informative and descriptive patient record.
What is the temperature of a vital sign?
Objective: Vital signs represent a temperature of 39°, BP of 130/80. Patient displays rashes, swollen lymph nodes and red throat with white patches.
Can you download soap note templates?
To help you get started we have created SOAP note templates you can download and customize for free.
Can iAuditor save patient records?
Easily share your findings with other healthcare clinicians and avoid losing track of patient records by securely saving it in the cloud using iAuditor
Why do nurses use soap notes?
Like separating dirty laundry from clean, SOAP notes are what nurses use to separate all the insignificant information about patients from significant information. It shows what is happening to patients in a neat and organized way. This makes it easier for other healthcare members to understand and care for patients more effectively.
What does soap stand for in nursing notes?
SOAP notes are a way for nurses to organize information about patients. SOAP stands for subjective, objective, assessment and plan.
What does it mean to enroll in a course?
Enrolling in a course lets you earn progress by passing quizzes and exams.
Why do nurses need to be documented?
The information also needs to be clearly documented so that other health providers can understand and do their part in caring for the patient.
What is an A in nursing?
A is for analysis or assessment. Nurses make assumptions about what is going on with the patients based on the information they obtained. Although these assessments are not the medical diagnosis that health care providers make, they still identify important problems or issues that need to be addressed.
What does S mean in medical terms?
S is for subjective, or what the patients say about their situation. It includes a patient's complaints, sensations or concerns. In most cases, it is the reason the patient came to see the doctor. Here are some examples: The patient complained of a severe pain on the right side of his head.
Do you have to be a Study.com member to unlock this lesson?
To unlock this lesson you must be a Study.com Member.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
How many OSCE checklists are there?
If you'd like to support us and get something great in return, check out our OSCE Checklist Booklet containing over 150 OSCE checklists in PDF format. You might also be interested in our Clinical Skills App and our OSCE Flashcard Collection which contains over 2000 cards.
What is assessment section?
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
What is the purpose of Part One of our two part special on diabetes?
Part one of our two part special on diabetes focuses on the firsthand experience of a patient living with diabetes. We discuss what it is like to be diagnosed with Type 1 diabetes and to live with and manage the condition day-to-day. We hope that this episode will be useful for students, medical professionals, and anyone who wants to understand more about the challenges of managing this condition. Guest: Ashwin Bali
What should be included in subjective documentation?
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
What is the final section of a review?
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
When to use quotation marks in a patient response?
You should document the patient’s responses accurately and use quotation marks if you are directly quoting something the patient has said.
Can you comment on a diagnosis that is already known?
If the diagnosis is already known and the findings of your assessment remain in keeping with that diagnosis, you can comment on whether the patient is clinically improving or deteriorating: