40 Fantastic SOAP Note Examples & Templates ᐅ …
34 hours ago · SOAP note example for Psychotherapist. Subjective . Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety. Objective . Stacey was unable to attend her session as she is on a family holiday this week. >> Go To The Portal
- The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns.
- Some common examples may include chest pain, decreased appetite, and shortness of breath.
- You can also talk to a family member or spouse to get any necessary information.
Full Answer
What is a SOAP note used for in healthcare?
What is a SOAP Note? A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information.
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
Do pediatricians need a SOAP note?
Being a pediatrician, you deal with various patients who face different types of conditions. But because infants, children, and adolescents can be quite vague with how they express their feelings, creating a medical SOAP note has proven to be a challenge. In such cases, you may have to consult the patient’s parent or guardian for further details.
What should be included in a patient report?
S.O.A.P. Report Format (S)ubjective: In this area you will document anything that the patient or family & friends tell you. Things to include: Chief complaint, MOI or NOI, SAMPLE including (PQRST), pertinent negatives.
What is included in a patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool. The documentation included on the PCR provides vital information, which is necessary for continued care at the hospital.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What should be included in a SOAP note assessment?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
How do you write a good patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
How do you write a SOAP note for nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo stands for subjective objective assessment and plan let's take a look at each of the fourMoreSo stands for subjective objective assessment and plan let's take a look at each of the four components. So you can understand this neat and organized way of note-taking.
What is the soap format in a medical record?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
How do I write a PT assessment?
2:0815:45How To Write a Physical Therapy Evaluation - YouTubeYouTubeStart of suggested clipEnd of suggested clipInformation the patient's medical history a systems review tests and measures posture and gaitMoreInformation the patient's medical history a systems review tests and measures posture and gait analysis. Range of motion. And muscle strength testing.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What is soap charting in nursing?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
How do you write a good PCR?
How to Write an Effective ePCR NarrativeBe concise but detailed. Be descriptive in explaining exactly what happened and include the decision-making process that led to the action. ... Present the facts in clear, objective language. ... Eliminate incorrect grammar and other avoidable mistakes. ... Be consistent and thorough.
What is the primary purpose of a patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool.
What is a PCR in writing?
The PARCC Summative Assessments in Grades 3-11 will measure writing using three prose constructed response (PCR) items. In the classroom writing can take many forms, including both informal and formal.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
SOAP note example for Nurse or Nurse Practitioner
John reports that he is feeling 'tired' and that he 'can't seem to get out of bed in the morning.' John is 'struggling to get to work' and says that he 'constantly finds his mind wondering to negative thoughts.' John stated that his sleep had been broken and he does not wake feeling rested.
SOAP note example for Psychotherapist
Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety.
SOAP note example for Paediatrician
Mrs. Jones states that Julia is "doing okay." Mrs. Jones said her daughter seems to be engaging with other children in her class. Mrs. Jones said Julia is still struggling to get to sleep and that "she may need to recommence the magnesium." Despite this, Mrs. Jones states she is "not too concerned about Julia's depressive symptomology.
SOAP note example for Social Worker
Martin has had several setbacks, and his condition has worsened. Martin reports that the depressive symptoms continue to worsen for him. He feels that they are 'more frequent and more intense. Depressive symptomology is chronically present.
SOAP note example for Psychiatrist
Ms. M. states that she is "doing okay." Ms. M. states that her depressive symptomatology has improved slightly; she still feels perpetually "sad." Ms. M.
SOAP note example for Therapist
"I'm tired of being overlooked for promotions. I don't know how to make them see what I can do." Frasier's chief complaint is feeling "misunderstood" by her colleagues.
SOAP note example for Counselor
David states that he continues to experience cravings for heroin. He desperately wants to drop out of his methadone program and revert to what he was doing.
What is a soap note?
A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication ...
What is the best software to collect SOAP notes?
Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. Collect photo evidence for a more informative and descriptive patient record.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
What is a medical soap note?
One of which includes the medical SOAP note. The note is a highly structured format required to communicate information to other healthcare providers, to provide proof of contact with the patient, and to document the procedure taken for treatment.
Why do pediatricians need a soap note?
But because infants, children, and adolescents can be quite vague with how they express their feelings, creating a medical SOAP note has proven to be a challenge. In such cases, you may have to consult the patient’s parent or guardian for further details. The doctor’s note is essential to aid the healthcare provider in their diagnosis.
What is a soap note?
But to a health professional, it’s all in a day’s work. A SOAP note is often used to document this assessment. It can be as brief or as detailed as possible, depending on the amount of information that needs to be acquired. 4. Medical Massage Therapy SOAP Note.
Why do expectant mothers need a soap note?
A medical SOAP note is written to report on the patient’s current status for further evaluation.
Why is infant medical soap important?
Infant Medical SOAP Note. The body of an infant is extremely delicate and sensitive to any infections, diseases, or injuries obtained. This is one of the reasons why parents and guardians are strictly advised to have their child checked once certain symptoms become apparent.
How to live with health issues?
Living with health issues is never easy. You could be put on a meal plan, an exercise regimen, and prescription pills for the rest of your life. Seeing a professional to help you with your struggles is one way to get by. A nutritionist may provide you with some guidelines to prevent your health from deteriorating and causing further problems. To determine which program will suit your condition and assess whether or not it is effective, a medical SOAP is written for documentation and reference. The information found in the medical note may also be discussed with other healthcare personnel to offer proper treatment.
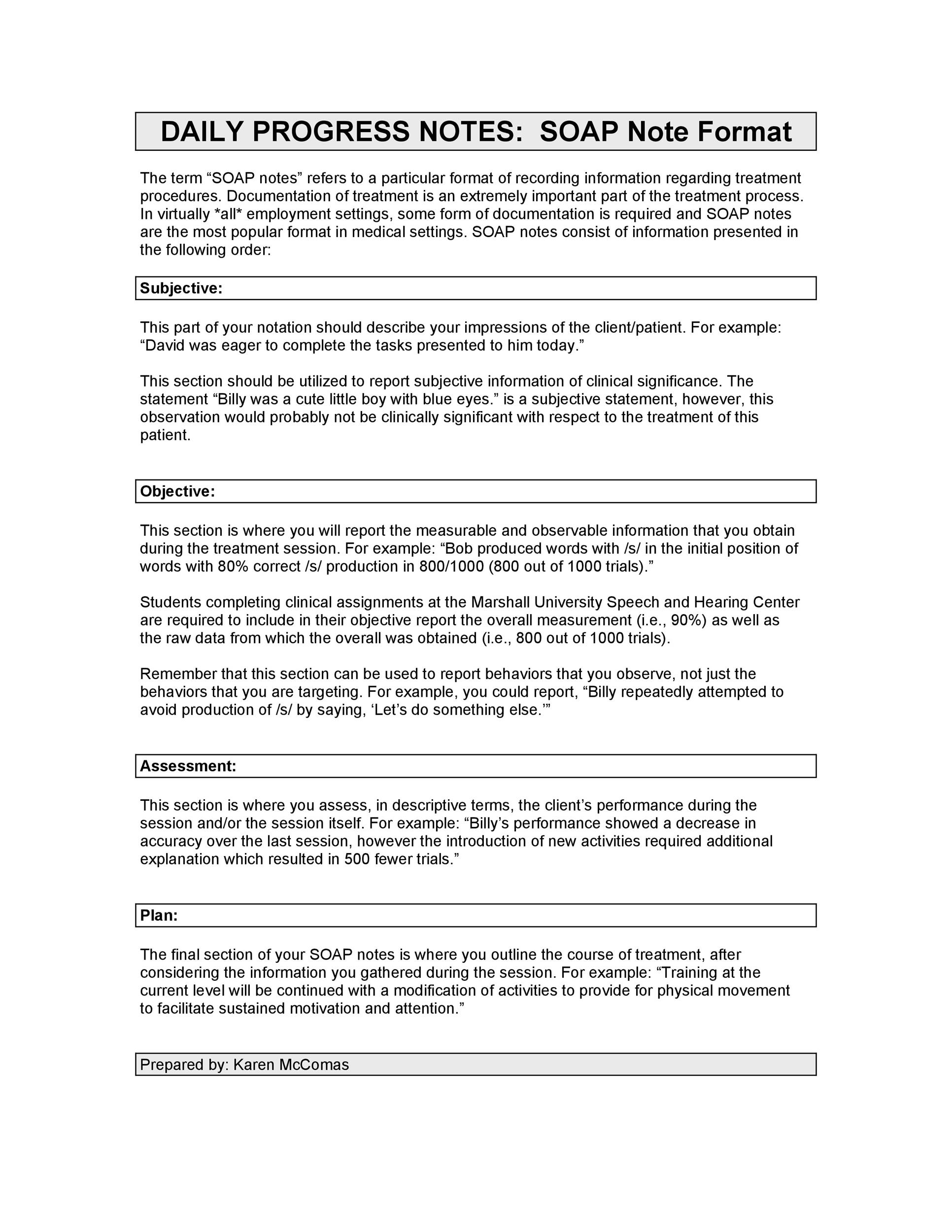
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
What is prepopulated detail in point care?
The Pre-populated details in Point Care should be viewed as “prompts” for elaboration of the specific treatment and should include patient/CG response that occurred on the visit. Details that are not pertinent to your patient should be edited out. Added text by the clinician to clarify the patient specific response, thereby supporting a skilled need, is highlighted.
What to do if daughter is unable to purchase cushion?
If daughter is unable or unwilling to purchase cushion, proceed with plans to discharge patient for reaching maximum potential with all goals.

What Are The Four Parts of A Soap Note?
Soap Note Example – How to Write & What Format
- Writing in a SOAP note format—Subjective, Objective, Assessment, Plan—allows healthcare practitioners to conduct clear and concise documentation of patient information. This method of documentationhelps the involved practitioner get a better overview and understanding of the patient’s concerns and needs. Below is a walkthrough of how you can effect...
Use A Template For Your Notes
- Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. 1. Create SOAP notes in digital format and easily update and share with teammates 2. Collect photo evidence for a more informative and descriptive patient record. 3. Save completed SOAP reports in a safe cloud stor…
Popular Posts:
- 1. summit pain management patient portal
- 2. john muir patient login
- 3. being subjective mean in patient care report
- 4. providence healthcare network waco patient portal
- 5. jackson-hinds patient portal
- 6. planned parenthood patient portal (p4) login
- 7. patient portal west tn health care
- 8. cystic fibrosis foundation patient registry 2016 annual data report
- 9. pediatricare associates patient portal
- 10. "inter-agency patient referral report" pdf