FREE Nursing Report Sheets & How to Make One - 2022
35 hours ago · Perfect patient report sheet for the ultimately organized nurse. All the important vital information for your patient on one page. Lots of … >> Go To The Portal
What are nurses required to report?
The law requires nursing homes to disclose more detailed financial information. This is especially important as an increasing number of facilities are owned by private equity firms. The law imposes additional requirements on facilities with repeated code violations, including more frequent surveys and more stringent penalties.
Can a nurse refuse treatment of a patient?
You cannot refuse to be involved in the care of patients because of their condition or the nature of their health problems. All blood and body fluids should be treated as infectious. All health care staff should understand local and national standards for infection control precautions. Please also see our infection protection and control guidance .
How do nurses affect patient outcomes?
“As a key player on the front lines of health care delivery, nurses play a critical role in preventing adverse events, coordinating care and enabling patients to achieve optimal outcomes,” Press Ganey states.
Should nurse to patient ratios be mandated?
The bill mandates that a one-to-one nurse-patient ratio would be imposed for patients in the ICU, OR, trauma, critical care, as well as for unstable neonates and patients needing resuscitation. Another provision of the bill places a one-to-three nurse-patient ratio limit for pediatrics and patients who are pregnant.

How do you write a nurse report sheet?
0:2120:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipGo to the search bar which is at the top right and type nursing report templates or nursing reportMoreGo to the search bar which is at the top right and type nursing report templates or nursing report sheets.
How should a nurse write a patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
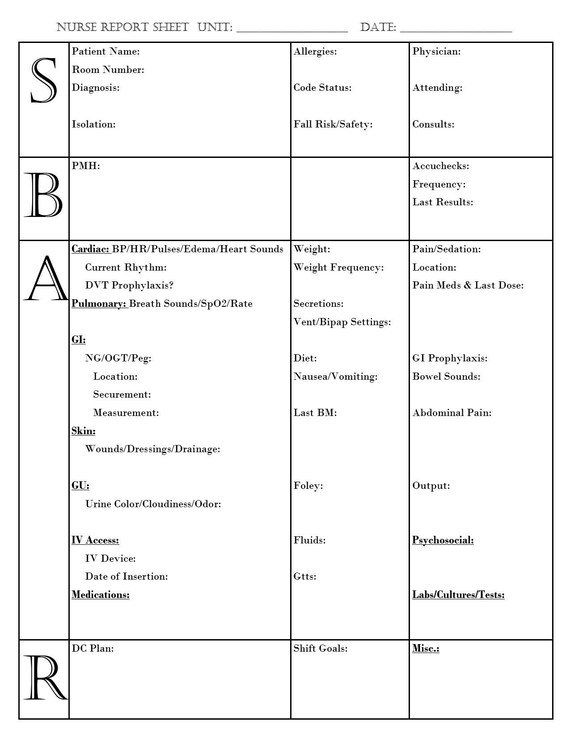
What is a report sheet in nursing?
A Nurse's Brain, also known as a nursing report sheet, is a term for a sheet of paper that nurses use to capture important patient information and stay organized. It contains sections for key areas like patient history, diagnoses, labs, medications, body systems status, and more.
How do you create a report sheet?
6 Steps to Make a Report SheetStep 1: Determine the Purpose. ... Step 2: Determine What to Include. ... Step 3: Write a Summary. ... Step 4: Explain Your Purpose. ... Step 5: Provide Your Recommendations. ... Step 6: Proofread the Report and Submit.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
How do I fill out a patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
How many types of nursing reports are there?
There are different types of nursing reports described in the literature, but the four main types are: a written report, a tape-recorded report, a verbal face-to-face report conducted in a private setting, and face-to-face bedside handoff.
What is SBAR template?
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
How a report should look like?
A report is designed to lead people through the information in a structured way, but also to enable them to find the information that they want quickly and easily. Reports usually, therefore, have numbered sections and subsections, and a clear and full contents page listing each heading.
How do you write a report example?
2:128:49How to write a Report | Format | Example | Blood Donation CampYouTubeStart of suggested clipEnd of suggested clipAnd designation if any in the left hand corner write the place of the report and below that writeMoreAnd designation if any in the left hand corner write the place of the report and below that write the date on which the report is written. After that comes the body of the report.
What is the format of a report?
Reports are divided into sections with headings and subheadings. Reports can be academic, technical, or business-oriented, and feature recommendations for specific actions. Reports are written to present facts about a situation, project, or process and will define and analyze the issue at hand.
Why do nurses need a report sheet?
A nursing report sheet enables these nurses to keep a track of the tasks that they have to perform. This allows them to go through their activities, in an untroubled manner and without missing out on any of the tasks.
Why are nursing report sheets important?
These report sheets are highly beneficial in helping the medical staff to obtain information efficiently.
What is an ICU nursing report?
ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
What is patient monitoring?
Patient Monitoring: Vital Signs – The Patient Monitoring section contains the vital signs that have been recorded at some particular time during their stay at the healthcare center. A few of the most important characteristics which are present in all the nursing reports are the Time Check, Blood Pressure details, Heart Rate, Temperature, Oxygen Saturation Levels, Oxygen, Respiratory Rates, Pain (if any, that has been inflicting the patient), Blood Sugar Details, Details of Dispensed Medications and Medicine Administration Timing.
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
Why is it important to create a nursing report?
A1. A nursing report is created to facilitate the job of transferring information. Therefore, it is highly essential that the nursing report is created in a manner that successfully fulfills its objective. Given below are a few tips which all nurses keep in mind to create a near-perfect nursing report:
What is a nursing report sheet?
A nursing report sheet is a paper template that a nurse uses throughout the day to keep track of what is going on with his or her patients. At the beginning of the day, a nurse might start a report sheet based on the information the leaving nurse provides. Throughout the day, that same nurse might have sheets specific to his or her patients ...
What is a patient simple task sheet?
The Patient Simple Nurse Task Sheet (number 4) or Patient Simple Tele Sheet (number 3) are excellent options for those who prefer a minimalist report sheet style. Other simple sheets from that website include All the Boxes and the Vertical Nurse Brainsheet with Assessment Diagram. You can download a three-patient-per-sheet mini report sheet as well. If you prefer, build your own with all the information that matters to you.
How much of a charge nurse brain sheet is needed?
As such, many charge nurse brain sheets are going to be broken down into patients or rooms with each only taking up 1/4 or 1/3 of the sheet itself.
Why use a nursing brain sheet?
The most significant benefit of using nursing brain sheets is that you have immediate access to information about each of your patients. For example, if your patient’s physician asks for information about the patient’s PT/PTT, you merely need to glance at your report sheet to find out the answer and relay it to the proper person. There are other ways a nursing report sheet can be helpful, however.
What is the whitespace nursing assessment sheet?
The Whitespace Nursing Assessment Sheet ( number 20 ) is an excellent example of this idea. The top has the information about the patient, while the edges leave room for information about labs, IV fluids, and other things of that nature. In the middle of the page is a large white area where you can keep note of anything that seems relevant.
Why do we need brain sheets?
When you work with a handful of patients on an average day, things can get mixed up. Your brain sheet prevents you from making errors or forgetting to chart essential things.
What is the most common communication method used in hospitals?
One of the most common techniques is the SBAR. It offers information on how information is structured, how it is communicated, and what it should be composed of. If this is a technique used by your facility, the good news is that there are many report sheets that take this into account.
How many nursing brainsheets are there?
But seriously . . . I’ve only shown you small portions of 20 of the 33 nursing brainsheets included in our massive database.
How many patients do you have in an ICU?
When you work ICU a lot of times you only have two patients . . .sometimes even just one.
Do nurses have to take reports?
Yep. Even charge nurses have to take report.
What is a nursing report sheet?
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report.
Why Do Nurses Use Nursing Report Sheets?
Nurse report sheets are very handy because they contain tidbits of vital information concerning your patient’s diagnosis, history, allergies, attending doctor,consults, things that need to be done on your shift, medication times, vital signs, lab results etc. The report sheet has other usage as well. Other usages of the nursing report sheet include but are not limited to:
What is a nursing note?
Nursing notes to remind yourself of things you need to do for the patient or chart on. Notes to yourself on things you want to remind the next shift. Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them.
Why is it important to have a 6 to 7 patient load?
When you have a 6 to 7 patient load, patient diagnosis and histories can run together and you may get them confused. Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do.
How to find out a patient's INR?
Fast access to patient information. If you are asked by a doctor what a particular patient’s INR was you could simply look at your report sheet to find out. You won’t have fumble around and try to remember which patient he/she was talking about.
Why do you write down on your chart sheet?
Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do. Again with 6 to 7 patients things tend to run together.
Can you print a report sheet for nurses?
You can share them with other nurses as well. Simply click the picture of the report sheet you like and after you download it you can print them. Tip: for less report sheets to carry around set your printer settings so you can print on the back side.
Why is it called a brain sheet?
They are common in nursing, especially when you are just starting off, to organize your thoughts and tasks throughout the shift. Yes, it’s called a brain sheet because literally, this becomes your BRAIN.
What is nursing handoff?
Nursing Handoff: an essential yet terrifying part of your job as a new nurse. If you have ever felt overwhelmed, unprepared, or straight up shoook during handoff, you are not alone. Giving a thorough and accurate report during change-of-shift is critical for patients, but it can give any new/student nurse anxiety beyond belief.
Why do we need a patient report?
These patient reports also help the doctors and the relatives of the patient to know what is or are behind the patients’ results of their individual health assessment . Thus, the form for patient report contains all the fields for information and exact details that are needed to be provided. In other words, the patient report forms are organized and layered which makes it easier to be filled with all the relevant information. And when all the precise information are provided, it is much easier to assess or evaluate the current state of one’s health condition.
Why are patient reports important?
Why Patient Reports Are Needed. Patient medical reports serve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not.
Why is a patient's medical record required?
Patient medical reportsserve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not. These reports are mandatory for the individual patient. This is for the reason that these are part of their health or medical history. Therefore, it is mandatory that the medical clinic, center, or hospital keeps a record of their patients.
What is the relevant information needed for a patient complaint?
In a patient complaint, the relevant information that are needed are as follows: The description of the situation. The effect on privacy.
What is healthcare personnel?
Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results). It goes without saying that everyone wants an accurate general information ...
Can medical records be shared with other people?
Yet, these medical reportsor records should not be shown to other unauthorized people. The reason for this is because these files are confidential, and the only people who could have access to these are those who are authorized, unless the patient or the owner of the records gives his or her consent for the informationto be released to certain people or to the public. Otherwise, the clinic, center, or hospital are held accountable for such infringement with regards to the confidential information.
Do hospitals keep records of patients?
Therefore, it is mandatory that the medical clinic, center, or hospital keeps a record of their patients. These patient reports also help the doctors and the relatives of the patient to know what is or are behind the patients’ results of their individual health assessment.