01.02 How to Take Nursing Report | NURSING.com
21 hours ago Number two, competence. Think of report is your chance to assume the care of a human being. This is a great responsibility and you can take pride in your role as a nurse. Don’t be afraid to ask questions, hold your head up and speak with confidence whether or not you feel competent. You still have to get report and care for the patient. >> Go To The Portal
Getting a good nursing report before you start your shift is vitally important. It is not only important for the nurse but for the patient as well. Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient.
Full Answer
How do you give a nursing report?
Nursing report is usually given in a location where other people can not hear due to patient privacy. If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended.
Can a nurse give report outside of a patient's room?
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended. SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
Is it hard to take Nursing Report?
Taking report is a skill and it can be extremely intimidating. Think of yourself as an investigator trying to uncover everything you can about this patient. I’m confident that if you follow these six steps and use the associated form, you will find great success in taking nursing report.
Why is it important to take a nursing report?
Taking an effective nursing report can set the tone for your entire shift and improve outcomes for your patient. Has anything changed or not been done? Join NURSING.com to watch the full lesson now. Taking report can be a very intimidating process.

How do you get a nursing report?
1:3420:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd what I do with my report should sheet. At the end of the day I always tread it so tip alwaysMoreAnd what I do with my report should sheet. At the end of the day I always tread it so tip always shred your report sheet whenever you're done giving a report you don't want to stick it in your locker.
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
How should a student nurse write a report?
How to Write a Nursing Report?State your position clearly.Write the reason why you are creating an internal report.Provide an example or at least two to show your position.Support your decision with statistics and facts.As much as possible, keep your report concise.More items...
How do you collect data in nursing?
The primary methods used to collect data are observing, interviewing, and examining. Observation occurs whenever the nurse is in contact with the client or support persons. Interviewing is used mainly while taking the nursing health history. Examining is the major method used in the physical health assessments.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What questions should a nurse consider when receiving a report?
Questions to Ask During Nursing Report:Does that patient have any family?Who is the patient's primary contact if something was to happen?Does the patient have any type of testing that they must be NPO for?Does the patient need assistance eating, showering, or using the bathroom?More items...
What is taking report in nursing?
Report or handoff involves providing information to the nurse who will be taking over the care of your patients. It should be given anytime patient care is transferred to another nurse. This may include at the end of your shift or if a patient is being transferred to another unit in the hospital.
What are the types of reports in nursing?
There are different types of nursing reports described in the literature, but the four main types are: a written report, a tape-recorded report, a verbal face-to-face report conducted in a private setting, and face-to-face bedside handoff.
Why is nursing report important?
Most importantly, communication supports the foundation of patient care. So, hand-off reporting during shift change is a critical process that is crucial in protecting a patient's safety. Throughout the hand-off report, it is vital to provide accurate, up-to-date, and pertinent information to the oncoming nurse.
What are the 5 methods of collecting data?
Before we dive deeper into different data collection tools and methods – what are the 5 types of data collection? Here they are: Surveys, quizzes, and questionnaires. Interviews....Qualitative data collection methodsOpen-Ended Surveys and Questionnaires. ... 1-on-1 Interviews. ... Focus groups. ... Direct observation.
How do you collect patient data?
You can collect patient data in several different ways — by conducting an interview in a clinical setting, by having the patient complete a paper form, or by having the patient fill out an online form.
What are the two primary methods used to collect data nursing?
The two primary methods of collecting data are interviewing and physical examination.
Why do nurses fill out report sheets?
According to research, when a nurse fills a report sheet, it makes their patient comfortable and guarded. Additionally, the report eliminates the time wastage required for another nurse to ask the patient about their condition.
Why do nurses need to rest?
A nurse’s duty can be tasking, and they need to have a period of rest because of how tedious the job might be. However, before transferring your duty to another, it is vital to provide relevant details of your patient.
Do nurses need a nursing report?
A nursing report is usually a document that nurses presents or handover to their fellow nurses when they want to go home. This report represents the details of a patient’s condition and is transferred to the next nurse on duty. Furthermore, a nursing report may also represent a nurse or doctor’s report during a legal investigation.
Why do nurses give reports outside of the room?
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended.
Why is it important to get a nursing report before you start your shift?
It is not only important for the nurse but for the patient as well. Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient.
What does SBAR stand for in nursing?
SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
You Need a Nursing Brain Sheet That Works for YOU
For the longest time I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
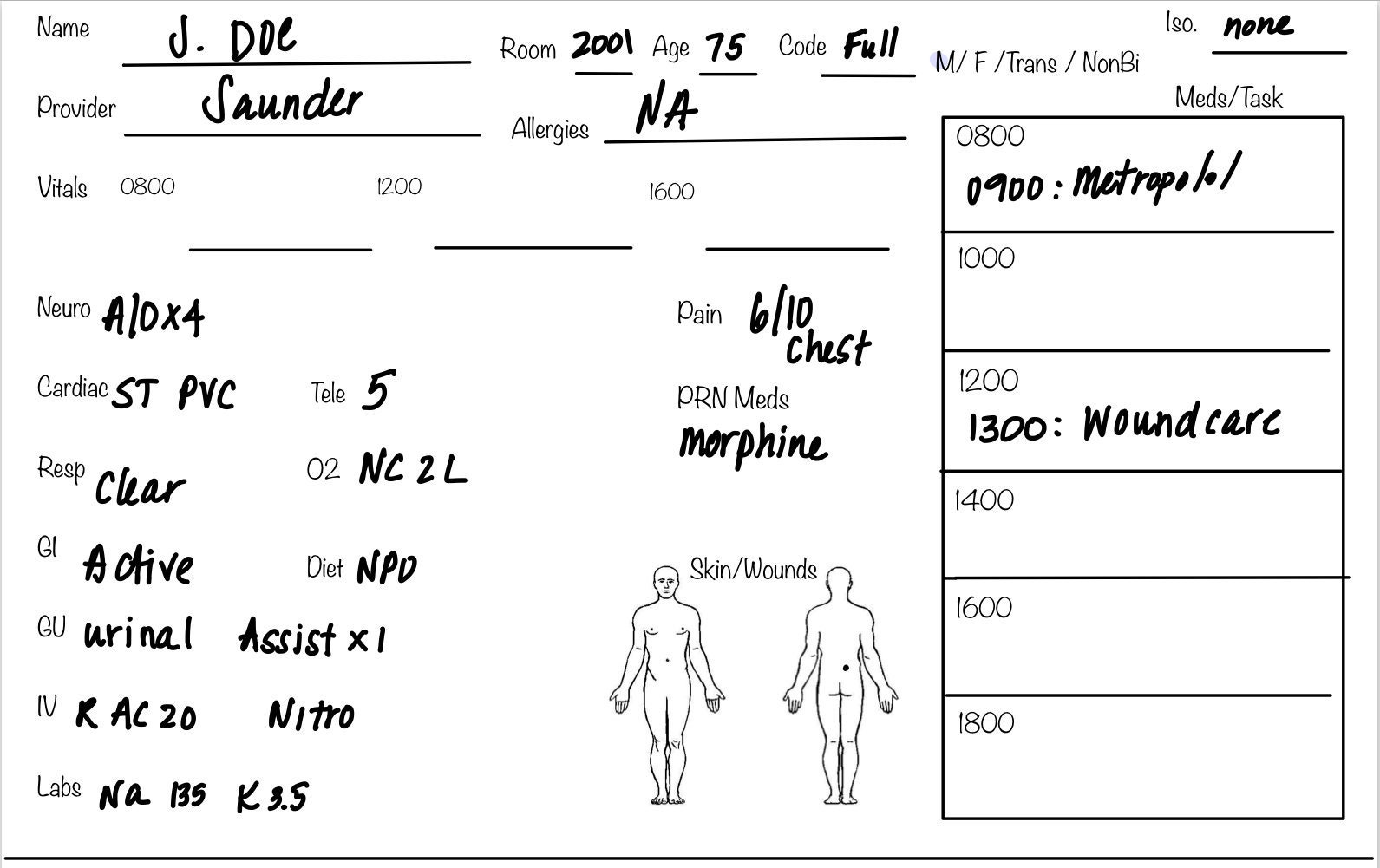
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . put at closer inspection you start to see all the details and information you have available with it. From lab values, to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experience nurse.
6. Just the Boxes
I’ll be honest . . . after a couple years of being a nurse my “brainsheet” has evolved into more of a few freehand drawing on a sheet of paper. If that sounds like you, this is probably the one for you. With little more than a few suggestions . . . this is a pretty basic organizer for nurses.
Do you know them?
It’s really recommended that you avoid taking care of patients whom you actually know in real life.
Are they discharging during your shift?
This can be a good thing or a bad thing. It’s a good thing if you need experience discharging a patient. It’s a bad thing if you need to write a paper or a care plan on that patient and will only have an hour or 2 to get all of the information you need.
Is their diagnosis too complicated or hard?
Okay…here’s the thing…I’m all about you giving it your 1000% in nursing school. That is amazing and you are a rock star.
Is their diagnosis too easy?
On the flip side, don’t settle for less (and this one goes for just about everything in life).
How to write an incident report?
In determining what to include in an incident report and which details can be omitted, concentrate on the facts.#N#Describe what you saw when you arrived on the scene or what you heard that led you to believe an incident had taken place. Put secondhand information in quotation marks, whether it comes from a colleague, visitor, or patient, and clearly identify the source.# N#Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected .#N#Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient’s physician. Include any statement a patient makes that may help to clarify his state of mind, as well as his own contributory negligence.#N#It’s equally important to know what does not belong in an incident report.#N#Opinions, finger-pointing, and conjecture are not helpful additions to an incident report.#N#Do not:
When is an incident report required?
When a situation is significant—resulting in an injury to a person or damage to property —it’s obvious that an incident report is required. But many times, seemingly minor incidents go undocumented, exposing facilities and staff to risk. Let’s discuss three hypothetical situations.
Why is incident reporting important?
An incident report invariably makes its way to risk managers and other administrators, who review it rapidly and act quickly to change any policy or procedure that appears to be a key contributing factor to the incident. The report may also alert administration that a hospital representative should talk to a patient or family to offer assistance, an explanation, or other appropriate support. That’s an important function because such communication can be the balm that soothes the initial anger—and prevents a lawsuit.
Why is it important to file incident reports?
Filing incident reports that are factually accurate is the only way to help mitigate potentially disastrous situations arising from malpractice and other lawsuits. It’s your responsibility to record unexpected events that affect patients, colleagues, or your facility, regardless of your opinion of their importance.
What is the duty of a nurse?
As a nurse, you have a duty to report any incident about which you have firsthand knowledge. Failure to do so could lead to termination. It could also expose you to liability, especially in cases of patient injury. Protect yourself and your patients by filing incident reports anytime unexpected events occur.
What happens when incident reports are filled out properly?
If the incident report has been filled out properly with just the facts, there should be no reason to be concerned about how it’s used. The danger comes only when incident reports contain secondhand information, conjecture, accusations, or proposed preventive measures that do not belong in these reports.
Why is it important to talk to a hospital representative?
That’s an important function because such communication can be the balm that soothes the initial anger —and prevents a lawsuit.
Popular Posts:
- 1. middlesex orthopedic group patient portal
- 2. greater newport physicians patient portal for authorization request
- 3. core pediatrics patient portal
- 4. lakewood regional medical center patient portal
- 5. island family medical patient portal
- 6. patient portal reflections
- 7. ocean psychiatric group patient portal registration
- 8. digestive disease physicians patient portal
- 9. southwest care center santa fe patient portal
- 10. www.adena.org/patient portal