Subjective & Objective Data for Patients & Clients
19 hours ago Objective data. You tell Mrs. Smith that you are going to start your physical assessment. You take her vital signs and find the following: blood pressure is 100/52, pulse is 74, respirations are ... >> Go To The Portal
What should be included in the objective section of a report?
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell. Document the patient’s appearance (e.g. “The patient appeared to be very pale and in significant discomfort.” ). “Widespread expiratory wheeze on auscultation of the chest.”
What are the objectives of a health insurance report?
Here are some common objectives that report sponsors cite : [1] Make more informed decisions among competing plans or providers. Make better health care choices. Compare and select the best plan or provider for their needs.
What is objective data in health care?
Definition of Objective Data. In the health care environment, the senses of seeing, hearing, smelling and touching are used to gather information about the patient. The patient's behaviors, actions, test results, measurements and the physical examination are also included.
What is the purpose of Patient Reported Outcome?
Patient-Reported Outcome (PRO) is a tool for capturing data on safety and efficacy. Data from patients may be classed as those that are detectable only by clinicians and data detectable only by patients, as exemplified by the following: Data detectable only by clinicians: tachycardia; neutropenia.

What is objective data of patient?
Objective patient data involves measurable facts and information like vital signs or the results of a physical examination. Subjective patient data, according to Mosby's Medical Dictionary, “are retrieved from” a “description of an event rather than from a physical examination.”
What is objective assessment of a patient?
Objective assessment involves the collection of data that you can observe and measure about the client's state of health.
What is an example of objective information?
Objective Data This is the information that we can gather using our 5 senses. It is either a measurement or an observation. Temperature is a perfect example of objective data. The temperature of a person can be gathered using a thermometer.
What is subjective and objective in medical?
Subjective data are information from the client's point of view (“symptoms”), including feelings, perceptions, and concerns obtained through interviews. Objective data are observable and measurable data (“signs”) obtained through observation, physical examination, and laboratory and diagnostic testing.
What are objective medical findings?
Objective Findings — observations made during medical evaluations that are not under the patient's control, such as X-ray results, nerve conduction studies, and MRIs.
How do you write an assessment objective?
The key to writing learning objectives is using an action verb to describe the behavior you intend for students to perform. You can use action verbs such as calculate, read, identify, match, explain, translate, and prepare to describe the behavior further.
What is objective data in nursing?
Objective data in nursing refers to information that can be measured through physical examination, observation, or diagnostic testing. Examples of objective data include, but are not limited to, physical findings or patient behaviors observed by the nurse, laboratory test results, and vital signs.
Is patient history subjective or objective?
subjective dataInformation obtained while performing a health history is called subjective data. Subjective data is information obtained from the patient and/or family members and can provide important cues about functioning and unmet needs requiring assistance.
What is difference between subjective and objective reporting?
Subjective information or writing is based on personal opinions, interpretations, points of view, emotions and judgment. It is often considered ill-suited for scenarios like news reporting or decision making in business or politics. Objective information or analysis is fact-based, measurable and observable.
Is cough objective or subjective?
Conclusion. Subjective measures of cough and cough reflex sensitivity are poor surrogates for objective cough frequency in asthma. When designing studies to assess interventions for cough in asthma, we advocate a combination of both objective measures of cough and cough-related quality of life.
Is MRI objective or subjective?
But your MRI (“objective”) is normal or shows minimal degenerative findings. In other words, the objective findings on the MRI are not severe enough to be consistent with the amount of back pain you are having.
Is vomiting objective or subjective?
So-called objective parameters may be misleading because nausea is a completely subjective phenomenon and vomiting on the other hand has both subjective and objective aspects [3, 12].
Why Objectives Are Important
Well-defined objectives can help your organization stay focused on the strategies that will move it closer to its goals.
Objectives Become What You Evaluate
The link between your project’s objectives and its future evaluation has three immediate implications for the planning process:
Common Purpose Statements
There are a number of different reasons why organizations decide to produce quality report cards for consumers. Here are some common objectives that report sponsors cite : [1]
For More Information
To learn more about selecting reasonable and measurable goals, go to Assess Your Reporting Project.
What is a patient report experience?
Patient report experiences through the use of PREMs, such as satisfaction scales, providing insight into the patients’ experience with their care or a health service. There is increasing international attention regarding the use of PREMS as a quality indicator of patient care and safety.
What is indicator in healthcare?
Indicators are a type of metric that identifies issues requiring further investigation (eg, increase in number of falls) (NHS Institute for Innovation and Improvement/Public Health Observatories, 2007) and reflects how effectively an organization is performing on a set of metrics.
What is a disease specific prom?
In contrast, disease-specific PROMs are designed to identify specific symptoms and their impact on the function of those specific conditions. Disease-specific PROMs have greater face validity and credibility than generic PROMs, but these comparisons cannot always be made across a variety of conditions.
What is IRT model?
IRT is a probabilistic, mathematically based model used to describe the relationship between an individual’s response to questions about his or her health and an underlying variable measured by the instrument (eg, strength of attitude, intelligence).
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
Why choose a platform that is web-enabled for quick reporting?
You’ll never miss important details of a patient incident because you can file your report right at the scene. A platform with HIPAA-compliant forms built in makes your workflow more efficient and productive, ensuring patient incidents are dealt with properly.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What is a PRO in clinical practice?
A patient-reported outcome (PRO) refers to an assessment of a patient’s health condition that comes directly from the individual (see Chapter 6 for further discussion). PROs are increasingly recognized as an important aspect of clinical practice and clinical trials.
What is a PRO in medicine?
This chapter reviews the definition, development, and utilization of PROs for both research and clinical purposes, including developmental considerations for administration of PROs with children. Health-related quality of life measures (HRQoL) are one type of PRO, and several condition-specific PROs have been developed for a variety of pediatric respiratory diseases, including vocal cord dysfunction, asthma, cystic fibrosis, sleep-related breathing disorders, and primary ciliary dyskinesia. A substantial body of literature has demonstrated that condition-specific, rather than generic measures, are more sensitive to change and better reflect the patient's symptoms and functioning. This chapter reviews the currently available PROs for pediatric respiratory conditions, including a description of the instrument, the domains of functioning it measures, the appropriate developmental age for administration, and the psychometric properties of the instrument, including its reliability and validity. Use of PROs is becoming standard practice for both randomized clinical trials and clinical care. The current shift in medicine toward patient-centered care is consistent with development and use of PROs. These measures provide unique information about patient symptoms, level of daily functioning, and systematic response to treatment. These measures have also been shown to facilitate patient-provider communication and shared decision-making. Integration of PROs into clinical care is a critical step in promoting patient-centered, quality health care practice.
What is a PRO?
A PRO is any measure of a patient's health status that reflects how a person functions, feels, or survives, as reported by the patient himself or herself. 3 Health-related quality of life (HRQOL) measures are one type of PRO that typically includes several domains of functioning. 4 These tools capture the aspects of functioning known only to the patient, including his or her symptoms, behaviors, and daily functioning (e.g., frequency of cough, physical limitations, worries about the future). PROs can be used for several purposes: (1) as primary or secondary outcomes in clinical trials, (2) to evaluate pharmaceutical, surgical, or behavioral interventions, (3) to assess the effect of a disease on multiple aspects of patient functioning, and (4) to develop individualized treatment plans. 5–8
Is condition specific measure more actionable than generic measure?
Although well-developed condition-specific or individualised measures are likely to have enhanced clinical relevance than generic measures, providing information that is more actionable, appropriate education and training in the application and interpretation of PROMs is required.
What is objective data in nursing?
Objective data in nursing is part of the health assessment that involves the collection of information through observations. In the health care environment, the senses of seeing, hearing, smelling and touching are used to gather information about the patient. The patient's behaviors, actions, test results, measurements and ...
How do nurses obtain objective data?
For instance, nurses can obtain objective data by noting the patient's body language and behavior. They also use tools, equipment, and techniques, including physical exams and diagnostic checks, to gather additional data. All of this ensures an efficient amount of information is obtained about patients.
What is subjective data?
Subjective data is another type of patient data that medical professionals collect. It can be defined as anything patients say about the reason for their doctor's visit. The phrase 'signs and symptoms' is often used to describe a patient's health problems. The signs refer to the objective data and are based on what the nurse sees. The symptoms refer to the subjective data and based on what patients say they feel. Another way to help you remember the difference is to see that 'objective' and 'observes' both begin with the letter 'O' while 'subjective' and 'says' both begin with the letter 'S.'
What does lack of eye contact mean?
Lack of eye contact could mean the patient is shy.
Is objective data more reliable than subjective data?
Objective data can be measured, and, in some cases, is more reliable than subjective data. You can see this in this example of a patient telling the nurse he quit smoking, though he still has the smell of cigarette smoke on his breath. Lesson Summary.
Is blood pressure subjective or objective?
In another instance, a patient states he feels his blood pressure is high, which is subjective. After hearing this, the nurse reads the patient's elevated blood pressure, which is objective. A patient says she feels like she has a fever; this is subjective.
Is a patient's cough subjective or objective?
In some cases, the data that is collected is objective and subjective at the same time, as seen in the following examples: A nurse hears a patient cough, which is objective. At the same time, the patient says he has been coughing for a week with a cold; this is subjective.
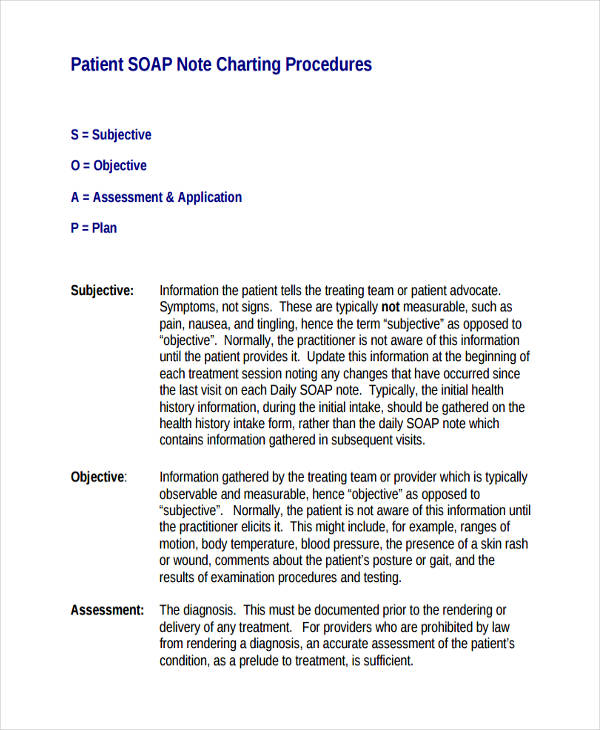
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
What are the objectives of a patient safety contract?
Objectives: Patient will contract for safety with staff at least once per shift. Patient will report any perceived conflict to staff. Patient will identify two medications and state why he is taking them. Patient will participate in at least one complete group or activity per day.
What is the goal of a bipolar patient?
Depressive Disorder (and Bipolar depressed) Goal: Resolution of depressive symptoms. Objectives: Patient will contract for safety with staff at least once per shift. Patient will identify two coping skills related to (specific stressor) Patient will report at least six hours of restful sleep each night.
How many hours of sleep do you need to be a patient?
Patient will report at least six hours of restful sleep a night. Patient will participate in at least two complete groups or activities a day. Patient will reality test (specific delusion) for at least 10 minutes a day with staff. Patient will eat at least two out of three meals a day.
How many hours of sleep do you need to report manic/hypomanic symptoms?
Resolution of manic/hypomanic symptoms. Objectives: Patient will report any perceived conflict to staff. Patient will report at least six hours of restful sleep per night. Patient will remain in at least two groups per day for the entire length of the group. Patient will eat at least two out of three meals a day.
Popular Posts:
- 1. memorial hospital nh patient portal
- 2. curemd patient portal app
- 3. christus schumpert patient portal login
- 4. frekko primary care patient portal
- 5. virginia hospital center patient portal
- 6. nexus group patient portal
- 7. standalone patient portal
- 8. dr manjul srivastava's patient records portal
- 9. t vincent patient portal
- 10. chartmaker patient portal registration