Ultimate Nursing Report Sheet Database & Free Downloads
2 hours ago Check out our nursing report sheet 5 patient selection for the very best in unique or custom, handmade pieces from our shops. >> Go To The Portal
What are nurses required to report?
The law requires nursing homes to disclose more detailed financial information. This is especially important as an increasing number of facilities are owned by private equity firms. The law imposes additional requirements on facilities with repeated code violations, including more frequent surveys and more stringent penalties.
Can a nurse refuse treatment of a patient?
You cannot refuse to be involved in the care of patients because of their condition or the nature of their health problems. All blood and body fluids should be treated as infectious. All health care staff should understand local and national standards for infection control precautions. Please also see our infection protection and control guidance .
How do nurses affect patient outcomes?
“As a key player on the front lines of health care delivery, nurses play a critical role in preventing adverse events, coordinating care and enabling patients to achieve optimal outcomes,” Press Ganey states.
Should nurse to patient ratios be mandated?
The bill mandates that a one-to-one nurse-patient ratio would be imposed for patients in the ICU, OR, trauma, critical care, as well as for unstable neonates and patients needing resuscitation. Another provision of the bill places a one-to-three nurse-patient ratio limit for pediatrics and patients who are pregnant.
How do I write a nursing report sheet?
0:0020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is atMoreSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is at the top right and type nursing report templates or nursing report sheets.
What should a nursing report include?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What is a report form in nursing?
Patient Progress Report A progress report is a written document that is vital in health care settings because this is where the health care practitioner will base their next plan of treatment. A good health progress report follows the ADPIE (Assessment, Diagnosis, Planning, Intervention, Evaluation) format.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
How do I fill out a patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
How do you make a report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What is SBAR report?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
How many nursing brainsheets are there?
But seriously . . . I’ve only shown you small portions of 20 of the 33 nursing brainsheets included in our massive database.
How many patients do you have in an ICU?
When you work ICU a lot of times you only have two patients . . .sometimes even just one.
Do nurses have to take reports?
Yep. Even charge nurses have to take report.
What is a nursing report sheet?
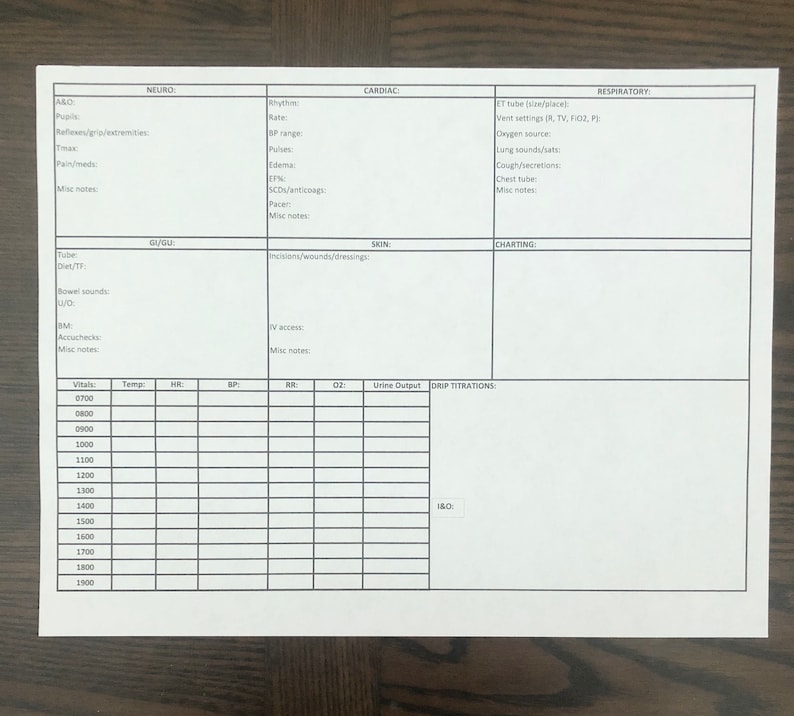
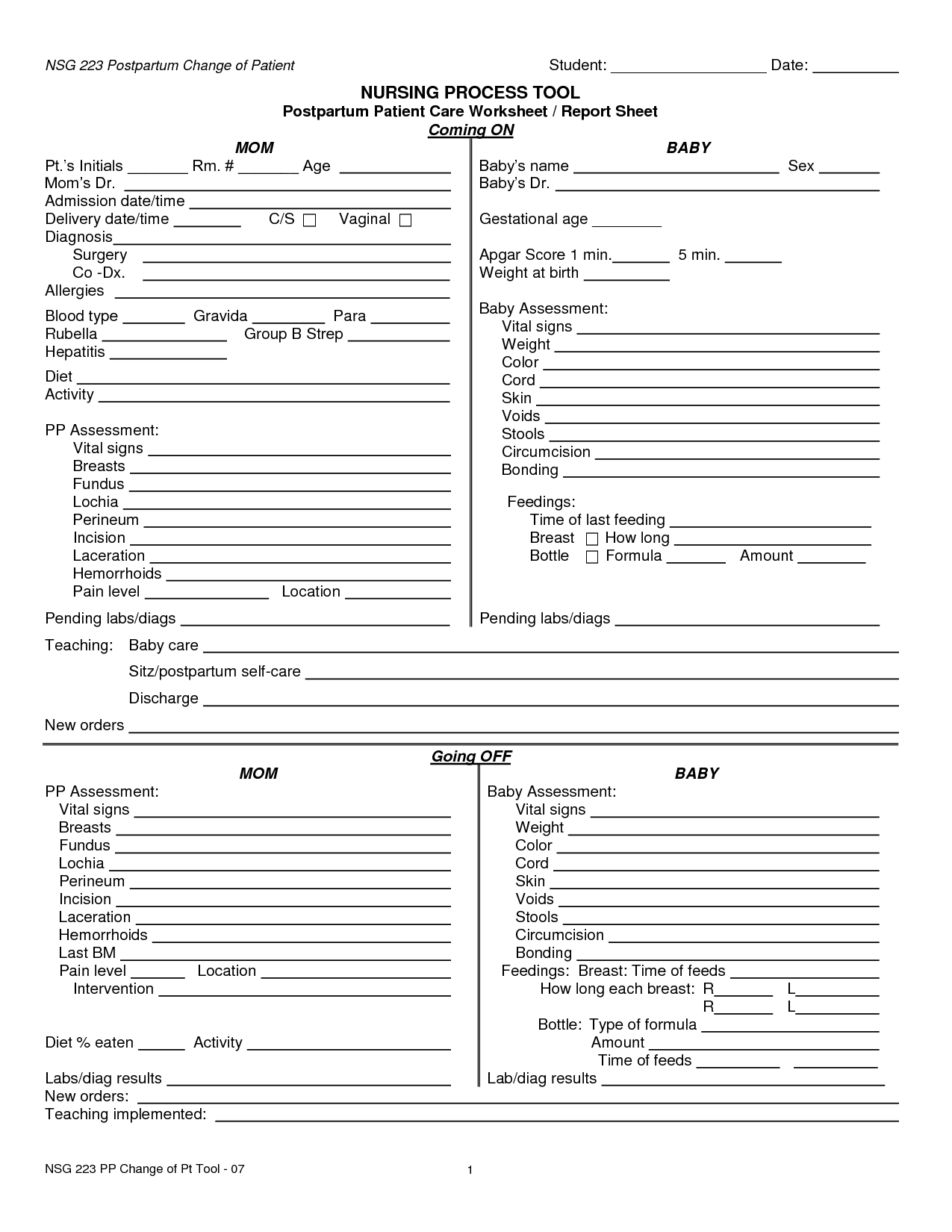
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report.
Why Do Nurses Use Nursing Report Sheets?
Nurse report sheets are very handy because they contain tidbits of vital information concerning your patient’s diagnosis, history, allergies, attending doctor,consults, things that need to be done on your shift, medication times, vital signs, lab results etc. The report sheet has other usage as well. Other usages of the nursing report sheet include but are not limited to:
What is a nursing note?
Nursing notes to remind yourself of things you need to do for the patient or chart on. Notes to yourself on things you want to remind the next shift. Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them.
Why is it important to have a 6 to 7 patient load?
When you have a 6 to 7 patient load, patient diagnosis and histories can run together and you may get them confused. Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do.
How to find out a patient's INR?
Fast access to patient information. If you are asked by a doctor what a particular patient’s INR was you could simply look at your report sheet to find out. You won’t have fumble around and try to remember which patient he/she was talking about.
Why do you write down on your chart sheet?
Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do. Again with 6 to 7 patients things tend to run together.
Can you print a report sheet for nurses?
You can share them with other nurses as well. Simply click the picture of the report sheet you like and after you download it you can print them. Tip: for less report sheets to carry around set your printer settings so you can print on the back side.
What is nursing handoff?
Nursing Handoff: an essential yet terrifying part of your job as a new nurse. If you have ever felt overwhelmed, unprepared, or straight up shoook during handoff, you are not alone. Giving a thorough and accurate report during change-of-shift is critical for patients, but it can give any new/student nurse anxiety beyond belief.
Why is it called a brain sheet?
They are common in nursing, especially when you are just starting off, to organize your thoughts and tasks throughout the shift. Yes, it’s called a brain sheet because literally, this becomes your BRAIN.