Nursing Report Sheet Template: 15 Best Templates and …
35 hours ago Check out our nurse report sheet 6 patient selection for the very best in unique or custom, handmade pieces from our templates shops. ... Single Patient Reporting Template, ICU Nurses resources, Med Surg, A4 and US Letter Ad by PlanPrintLand Ad from shop PlanPrintLand PlanPrintLand From shop PlanPrintLand. 5 out of 5 stars (2,417) >> Go To The Portal
What is a nursing report sheet?
When a patient has been registered for care in a healthcare institution, nurses form to be one of the primary groups in-charge of taking care of the said patients. In order to make sure that they are able to provide the optimum required care, nurses use a tool known as the Nursing Report Sheet.
What is completion in a nursing report template?
Completion – Completion is the final section of a nursing report template. This section contains the details regarding the nurse on duty. The various details to be recorded here are the Name, Signature of the Nurse and the Date and Time of the ending of the shift.
What is a med surg organization sheet?
For example, the room where the patient was treated, the name of the patient, the contact of the person closest to the patient, the condition of the patient during treatment, and also the type of care received. Med surg organization sheet functions as a journal report. So that tracking can be done in patients who have just had surgery.
Why are nursing report templates important in healthcare?
This means that, even if there is a change in the shifts of a particular group of doctors or nurses, the subsequent shift can continue providing care to their patients without any obstacles. Being such a useful and essential part in healthcare circles, these nursing report templates are implemented by institutions all around the world.
How do I write a nursing report sheet?
0:0020:45Nursing Shift Report Sheet Templates | How to Give a Nursing Shift ReportYouTubeStart of suggested clipEnd of suggested clipSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is atMoreSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is at the top right and type nursing report templates or nursing report sheets.
What should be included in a nurse to nurse report?
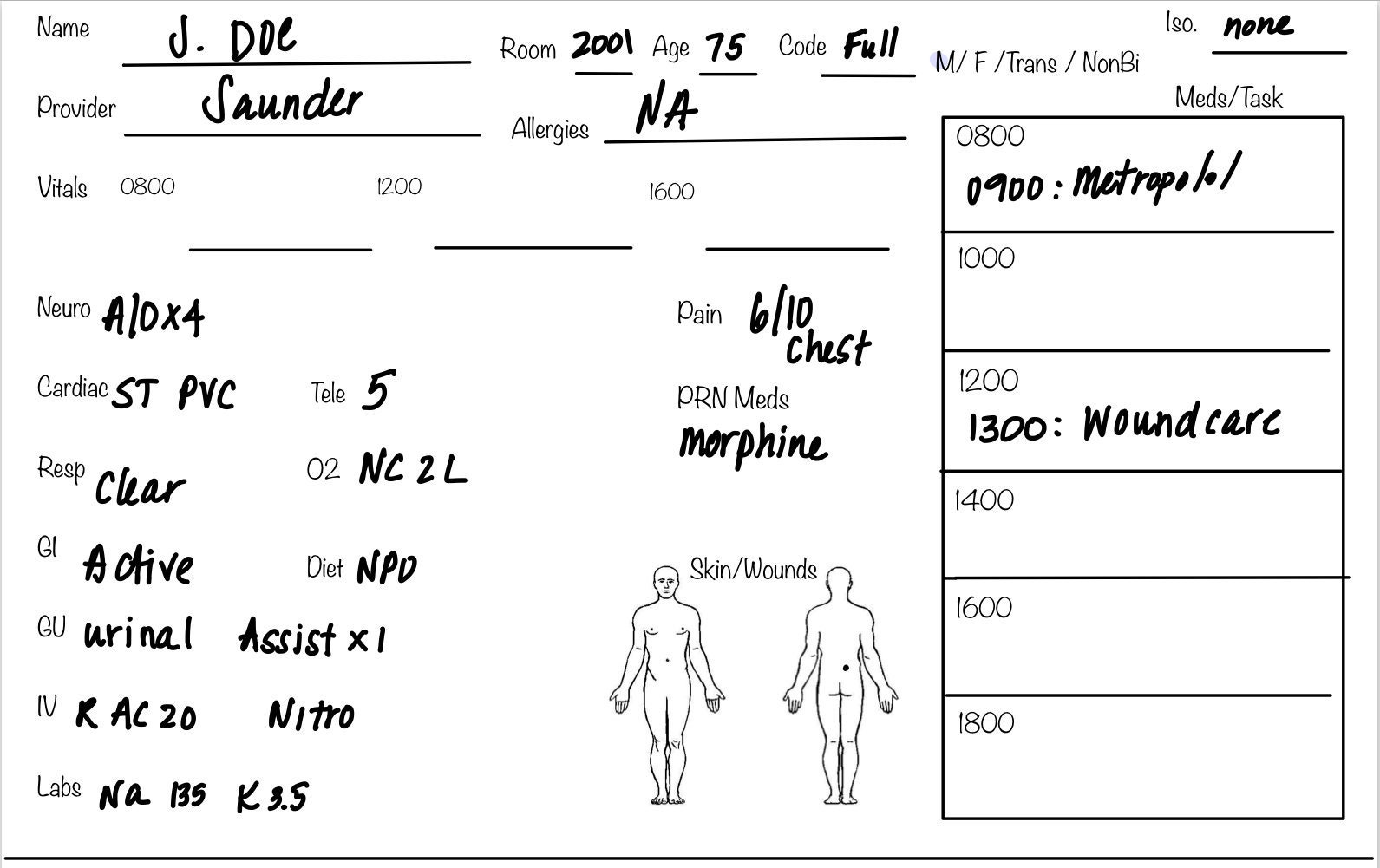
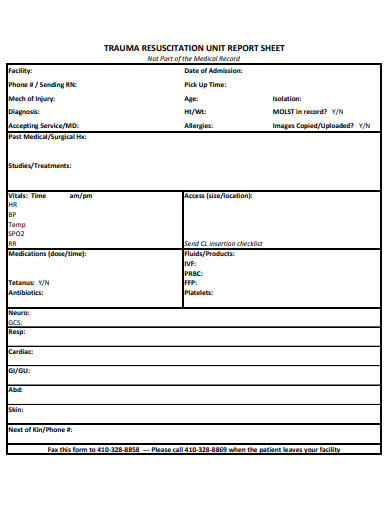
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What should be included in a nursing shift report?
Written by nurses who are wrapping up their shifts and provided to those nurses beginning the next shift, these details should include a patient's current medical status, along with his or her medical history, individual medication needs, allergies, a record of the patient's pain levels and a pain management plan, as ...
What is a nursing brain sheet?
A "brain sheet" is simply a reference used by nurses so they can keep track of important information about each patient. This sheet is often filled out with key information during change-of-shift report and then updated as things change (and they always do!).
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What is good nursing documentation?
The nursing record should include assessment, planning, implementation, and evaluation of care. Ensure the record begins with an identification sheet. This contains the patient's personal data: name, age, address, next of kin, carer, and so on. All continuation sheets must show the full name of the patient.
How do I write a nursing daily report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
What is the SBAR format?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
What is SBAR template?
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
How do you make a brain sheet?
1:4511:02How to Make a Brain Sheet, Cheat Sheet, Nursing Report ... - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo if you start from the top I always start with the patient's room number the patient's. Name they'MoreSo if you start from the top I always start with the patient's room number the patient's. Name they're grabbing a pair of status. Their blood type GPS status what time they were ruptured.
What is a nurse report?
Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient. Nursing report is usually given in a location where other people can not hear due to patient privacy.
How do you use a nursing brain sheet?
0:3410:04Nurse Brain Sheet | ORGANIZE YOUR NURSING SHIFT | Nursing ReportYouTubeStart of suggested clipEnd of suggested clipSo this is what my report sheet looks like I use it as a half pane over here and I can fit twoMoreSo this is what my report sheet looks like I use it as a half pane over here and I can fit two patients on one sheet. And what I like to do is I actually take it. And I fold it in.
How do you give a good report?
How to write a report in 7 steps1 Choose a topic based on the assignment. Before you start writing, you need to pick the topic of your report. ... 2 Conduct research. ... 3 Write a thesis statement. ... 4 Prepare an outline. ... 5 Write a rough draft. ... 6 Revise and edit your report. ... 7 Proofread and check for mistakes.
What should a handover nurse include?
What goes in to a handover?Past: historical info. The patient's diagnosis, anything the team needs to know about them and their treatment plan. ... Present: current presentation. How the patient has been this shift and any changes to their treatment plan. ... Future: what is still to be done.
How do I write a good bedside report?
5 Best Practices For an Effective Bedside Shift ReportShift Reports Should be Done at the Bedside. ... A Great Bedside Report Sets the Tone for the Shift. ... Be Mindful of Patient Privacy. ... Benefits of a Great Shift Report. ... Ask The Oncoming Nurse “What Other Information Can I Provide For You?
How do you make a good sbar?
The components of SBAR are as follows, according to the Joint Commission:Situation: Clearly and briefly describe the current situation.Background: Provide clear, relevant background information on the patient.Assessment: State your professional conclusion, based on the situation and background.More items...
Description
Color coded to differentiate between patients. This is a patient report sheet, allows you to keep all the information organized and efficiently keep track of your patients during day or night shift. It includes all the pertinent information you may need.
More from this shop
Get 10% off your order when you spend $110 at this shop. Discount shown at checkout.
What is an organization sheet in med sg?
What a Med Surg organization sheet contains? At the Med Surg department, there are certainly organization sheets that are part of their duties. Contains data about patients in the scope of their care. For example, the room where the patient was treated, the name of the patient, the contact of the person closest to the patient, ...
Why is the knowledge possessed by each nurse so different?
The knowledge possessed by each nurse is very different because, in their studies, they have focused on one department. So that the action that can be taken by all the nurses initially is general medical knowledge.
What is a med sage?
Med Surg stands for medical-surgical which is a department that contains nurses specifically handling patients who need recovery after undergoing surgery. There is no specific age for patients treated by Med Surg nurses. To be sure, after undergoing surgery, patients will find it difficult to move the body and there are even some patients who need ...
You Need a Nursing Brain Sheet That Works for YOU
For the longest time I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . put at closer inspection you start to see all the details and information you have available with it. From lab values, to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experience nurse.
6. Just the Boxes
I’ll be honest . . . after a couple years of being a nurse my “brainsheet” has evolved into more of a few freehand drawing on a sheet of paper. If that sounds like you, this is probably the one for you. With little more than a few suggestions . . . this is a pretty basic organizer for nurses.