Bedside shift report: Nurses opinions based on their …
2 hours ago Strategy 3: Nurse Bedside Shift Report. Research shows that when patients are engaged in their health care, it can lead to measurable improvements in safety and quality. To promote stronger engagement, Agency for Healthcare Research and Quality developed the Guide to Patient and Family Engagement in Hospital Quality and Safety, a tested, evidence-based resource to help … >> Go To The Portal
Does bedside shift report improve patient safety and nurse accountability?
Bedside shift report improves patient safety and nurse accountability J Emerg Nurs. 2010 Jul;36(4):355-8.doi: 10.1016/j.jen.2010.03.009.
How do you write a bedside report on a patient?
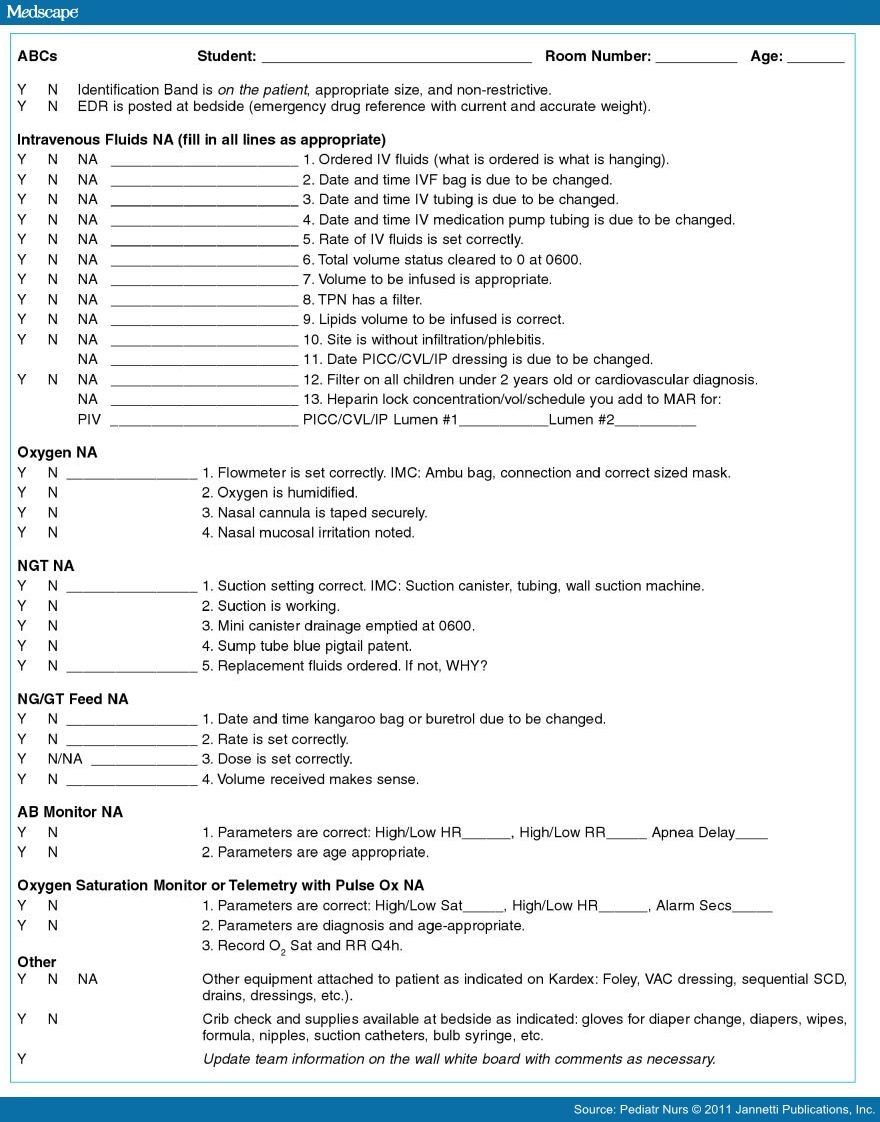
It should start outside of the patient's room covering the general information history what's occurred, then kind of go through a head‐to‐toe assessment of what's going on. Then you go into the room and you can finish the bedside report at the bed, looking at all of the things that you might have noted.
Where can I find nurse-to-nurse bedside shift report implementation handbook?
Nurse bedside shift report implementation handbook. www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/engagingfamilies/strategy3/Strat3_Implement_Hndbook_508.pdf. 26. Caruso EM. The evolution of nurse-to-nurse bedside report on a medical-surgical cardiology unit. . 2007;16(1):17–22.
What is the relationship between nursing workload and patient safety?
The nurse-to-patient ratio is only one aspect of the relationship between the nursing workload and patient safety. Overall nursing workload is likely linked to patient outcomes as well.
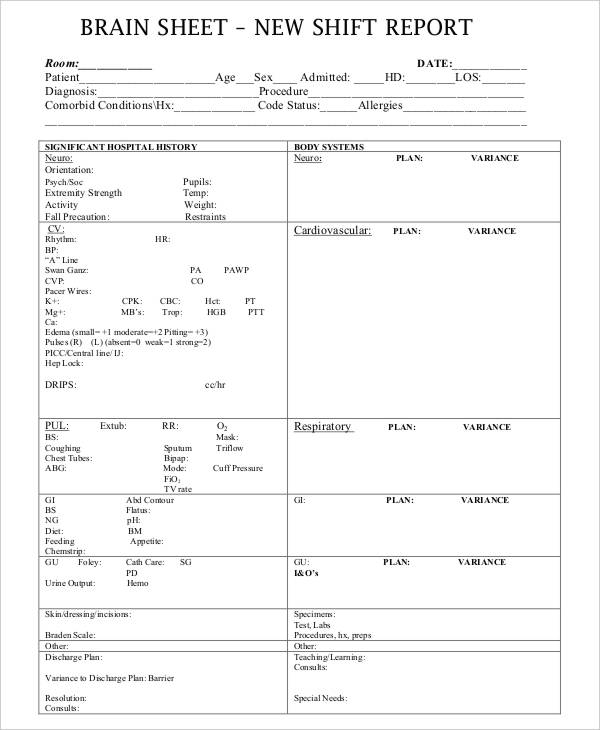
What should be included in a bedside report?
Now, during a bedside report, patients may include information not previously shared, ask questions, and thank the nurses for spending the time to discuss what's going on.
What is bedside report in nursing?
Bedside shift reports are the essential transmission of patient information between incoming and outgoing nurses in a patient care setting. This nursing communication provides for the continuity of safe and effective medical care and prevents medical errors.
How do I write a good bedside report?
Here's what they had to say:Give a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What is a bedside report?
By definition, a BSR is the change-of-shift report between the offgoing nurse and the oncoming nurse that takes place at the bedside. This makes patients a part of the process in the delivery of care.
Why is bedside report important in nursing?
Bedside shift report (BSR) enables accurate and timely communication between nurses, includes the patient in care, and is paramount to the delivery of safe, high quality care.
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do you give a good report?
1:2020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd what I do with my report should sheet. At the end of the day I always tread it so tip alwaysMoreAnd what I do with my report should sheet. At the end of the day I always tread it so tip always shred your report sheet whenever you're done giving a report you don't want to stick it in your locker.
Does bedside reporting increased patient safety?
Research concluded that conducting bedside reporting leads to increased patient safety, patient satisfaction, nurse satisfaction, prevented adverse events, and allowed nurses to visualize patients during the shift change. In addition, medication errors decreased by 80% and falls by 100%.
What are 4 components of correct nursing documentation?
For documentation to support the delivery of safe, high-quality care, it should: Be clear, legible, concise, contemporaneous, progressive and accurate.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
How do nurses give good reports?
1:1611:43How to Give a Good Nursing Shift Report (with nursing report sheet ...YouTubeStart of suggested clipEnd of suggested clipAll. Right guys here we are looking at our handoff. Report and assessment sheet this is the sheetMoreAll. Right guys here we are looking at our handoff. Report and assessment sheet this is the sheet that I recommend that you print out about 30 minutes before the end of any shift and print out one for
How do I improve my bedside handover?
Yet a simple strategy to improve communication is to bring the report to the patient's bedside. This facilitates earlier connection between the oncoming nurse and the patient and presents an opportunity for the patient to ask questions and clarify information with both nurses.
What should a handoff report include?
Nurses complete their handoff report with evaluations of the patient's response to nursing and medical interventions, the effectiveness of the patient-care plan, and the goals and outcomes for the patient. This category also includes evaluation of the patient's response to care, such as progress toward goals.
What is bedside handoff report?
Nurse bedside shift report, or handoff, has been defined in the literature as a process of exchanging vital patient information, responsibility, and accountability between the off-going and oncoming nurses in an effort to ensure safe continuity of care and the delivery of best clinical practices.2-6 There are different ...
How do you give a good handover in nursing?
Here are five tips to polish your handover technique:Be organised. Try to follow an organised sequence when handing over: patient details, presenting complaint, significant history, treatment and plan of care. ... Stay focused. Stay relevant. ... Communicate clearly. Be concise and speak clearly. ... Be patient-centred. ... Allow time.
Why are nurses always on the same page during the report?
Nurses are always on the same page during the report because they're both looking at the same information at the same time. 12. The patient benefits from BSR too.
How does BSR help nurses?
The advantages for the nurse begin with the efficiency of report, which streamlines all pertinent information and saves nursing time. BSR improves staff's teamwork by giving nurses the opportunity to work together at the bedside, ensuring accountability. Using a standardized format reduces the risk of miscommunication because it overcomes different communication styles. Better communication also helps the oncoming nurse prioritize assignments according to need. The nurse is informed about the patient earlier in the shift because report time is shortened. Nurses are always on the same page during the report because they're both looking at the same information at the same time. 12
What is a SBAR board?
The SBAR communication tool can be adapted for BSR as follows. A dry erase board placed in the patient's line of vision can be used to convey information such as the names of nurses and healthcare providers and to highlight the patient's goal for the day.
Why is BSR important in nursing?
Because nurses are the first line of defense when it comes to patient safety, BSR is an integral part of the care plan. The nurse is accountable for the communication that occurs during the change-of-shift report.
How many people died from BSR in 2010?
According to the Inspector General Office, Health and Human Services Department, less-than-competent hospital care contributed to the deaths of 180,000 Medicare patients in 2010. However, the real number may be higher: According to one estimate, between 210,000 and 440,000 patients who go to ...
How many breaths per minute did the nurse take in 1920?
When two nurses entered her room at 1920 for the BSR, her respiratory rate had dropped to 6 breaths/minute. One nurse stayed in the room while the other obtained and administered naloxone as per protocol. The patient quickly recovered without complications.
Why is standardized format important for nurses?
Using a standardized format reduces the risk of miscommunication because it overcomes different communication styles. Better communication also helps the oncoming nurse prioritize assignments according to need. The nurse is informed about the patient earlier in the shift because report time is shortened.
What are nursing sensitive measures?
These included patient-centered outcomes considered to be markers of nursing care quality (such as falls and pressure ulcers) and system-related measures including nursing skill mix, nursing care hours, measures of the quality of the nursing practice environment (which includes staffing ratios), and nursing turnover . These measures are intended to illustrate both the quality of nursing care and the degree to which an institution’s working environment supports nurses in their patient safety efforts. Nurse-sensitive indicators are a metric for the degree to which acute care hospitals provide quality, patient safety, and promote a safe and professional work environment. Nurse-sensitive measures continue to set the standard for quality and safety in care in the acute scare setting. As of 2021, there are 39-nurse sensitive measures.
What is nurse sensitive indicator?
Nurse-sensitive indicators are a metric for the degree to which acute care hospitals provide quality, patient safety, and promote a safe and professional work environment. Nurse-sensitive measures continue to set the standard for quality and safety in care in the acute scare setting. As of 2021, there are 39-nurse sensitive measures.
How many states have nurse staffing laws?
According to the American Nurses Association, only 14 states have passed nurse staffing legislation as of March 2021 and most states do not specify registered-nurse (RN)-to-patient ratios, which vary by state and are also setting-dependent.
What is missed nursing care?
Missed nursing care is a phenomenon of omission that occurs when the right action is delayed, is partially completed, or cannot be performed at all. In one British study, missed nursing care episodes were strongly associated with a higher number of patients per nurse. Missed nursing care errors have been identified as common and universal and secondary to systemic factors that bring undesirable consequences for both patients and nursing professionals. Omission of care has been linked to both job dissatisfaction and absenteeism for nurses, as well as to medication errors, infections, falls, pressure injuries, readmissions, and failure to rescue.10 In addition, If bullying is present within the workplace, more nurses are likely to self-report missed nursing care.11
Why are nurses important?
Nurses play a critically important role in ensuring patient safety while providing care directly to patients. While physicians make diagnostic and treatment decisions, they may only spend 30 to 45 minutes a day with even a critically ill hospitalized patient, which limits their ability to see changes in a patient’s condition over time. Nurses are a constant presence at the bedside and regularly interact with physicians, pharmacists, families, and all other members of the health care team and are crucial to timely coordination and communication of the patient’s condition to the team. From a patient safety perspective, a nurse’s role includes monitoring patients for clinical deterioration, detecting errors and near misses, understanding care processes and weaknesses inherent in some systems, identifying and communicating changes in patient condition, and performing countless other tasks to ensure patients receive high-quality care.
Why is vigilance important in nursing?
Nurse staffing and patient safety. Nurse staffing ratios. Nurses' vigilance at the bedside is essential to their ability to ensure patient safety. It is logical, therefore, that assigning increasing numbers of patients eventually compromises a nurse’s ability to provide safe care.
What is the causal relationship between nurse-to-patient ratios and patient outcomes?
The causal relationship between nurse-to-patient ratios and patient outcomes likely is accounted for by both increased workload and stress, and the risk of burnout for nurses. The high-intensity nature of nurses' work means that nurses themselves are at risk of committing errors while providing routine care.
Popular Posts:
- 1. carecentrix cigna patient portal
- 2. mercymaine hospital patient portal
- 3. mercy medical iowa patient portal
- 4. st ritas lima ohio patient portal
- 5. alabama family practice patient portal
- 6. dr guth hermatige tn patient portal
- 7. patient portal fenway health
- 8. cedar sinai patient portal login
- 9. dr grunstra patient portal
- 10. piedmont ent patient portal