Nursing Report Sheet Template: 15 Best Templates and Images in …
32 hours ago Another thing to consider and is necessary in the nursing incident report is the casualties or any person who was involved or in pain, for example, a patient, a significant other, or even a nurse. Next are the persons who were notified like the treating physician, the emergency personnel, or the administration. The actions or interventions are also necessary for the nursing incident report as this can be used for the investigation of what happened … >> Go To The Portal
For example: Write this: “The patient, who typically uses a cane, was walking down the hall when he slipped on the wet floor. The patient was not using his cane at the time of the fall.”
Full Answer
What is a nursing report?
by CNACTEdit@rs| Oct 9, 2018 A nursing report sheet is a paper template that a nurse uses throughout the day to keep track of what is going on with his or her patients. At the beginning of the day, a nurse might start a report sheet based on the information the leaving nurse provides.
What are some examples about the nursing process?
- The social status. ...
- The actual job it’s self is rewarding, you’ll see the difference you’ve made
- The actual nature of the job allows you to climb the career ladder easily and quickly, meaning if your stuck in a certain sector of nursing you will have training ...
What are examples of nursing diagnosis?
Examples of this type of nursing diagnosis include:
- Risk for imbalanced fluid volume
- Risk for ineffective childbearing process
- Risk for impaired oral mucous membrane integrity
What is a nursing incident report?
- Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes. ...
- Quality assurance. Quality assurance is all about patient safety, customer satisfaction, and improving healthcare quality. ...
- Educational tools. ...
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
What is a nursing report sheet?
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report.
How do you organize a nursing report sheet?
0:1210:04Nurse Brain Sheet | ORGANIZE YOUR NURSING SHIFT | Nursing ReportYouTubeStart of suggested clipEnd of suggested clipOrganization tips for you to be successful during your nursing shift the main one being a reportMoreOrganization tips for you to be successful during your nursing shift the main one being a report sheet and this is what people call their nurse brains.
How do you do a patient report?
0:3611:43How to Give a Good Nursing Shift Report (with nursing report sheet ...YouTubeStart of suggested clipEnd of suggested clipReport and assessment sheet this is the sheet that I recommend that you print out about 30 minutesMoreReport and assessment sheet this is the sheet that I recommend that you print out about 30 minutes before the end of any shift and print out one for every patient.
What should a nursing report include?
It should include the patient's medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
How do I write a good bedside report?
5 Best Practices For an Effective Bedside Shift ReportShift Reports Should be Done at the Bedside. ... A Great Bedside Report Sets the Tone for the Shift. ... Be Mindful of Patient Privacy. ... Benefits of a Great Shift Report. ... Ask The Oncoming Nurse “What Other Information Can I Provide For You?
How do I create a report sheet?
0:5111:10How to Organize a Nursing Report Sheet - YouTubeYouTubeStart of suggested clipEnd of suggested clipName I always do their last name first followed by their first name since that's how all the medicalMoreName I always do their last name first followed by their first name since that's how all the medical documents always have it and I usually capitalize.
How can I get better at giving a report?
5 Tips for an Effective End-of-Shift ReportGive a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
How do you organize yourself as a nurse?
All of these organization tips are super helpful, no matter how long you've been a nurse.#1 Do A Quick Pre-Report Chart Review. ... #2 Set Up Your Report Sheets The Same Way. ... #3 Review Your Patient's Chart Before You See Them. ... #4 Plan Your Day. ... #5 Keep Your Pockets Organized. ... #6 Stay Organized At Home.
How do I report a nursing assessment?
The following are comprehensive steps to write a nursing assessment report.Collect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
What to expect after writing a report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes...
What do I need to tell the patient and the patient’s family?
Educate the patient or the significant other on what to expect regarding the incident report. Impart an explanation when results of some procedures...
Do you dread writing a nurse report?
Now, that depends on the person writing it. Stressing over getting the report done or about what to include are common concerns for nurses. Always...
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes...
What Do I Need to Tell the Patient and the Patient’s Family?
Educate the patient or the significant other on what to expect regarding the incident report. Impart an explanation when results of some procedures...
Do you dread writing a nurse incident report?
Now, that depends on the person writing it. Stressing over getting the report done or about what to include are common concerns for nurses. Always...
What is a nursing report?
A nursing report focuses on providing accurate details of nursing by developing conducted research understood to the complete level of practicing nurses, educators, and interested members of the public. The sample report templates act as a huge help when it comes to constructing a precise nursing report. You may also check here Report Examples
Why is it important to have a nursing report?
It is important for good clinical communication to have a concise nursing report. A great report provides an accurate reflection of nursing assessments to support the medical team to provide great care. Objective. To provide a structured and standardized approach regarding nursing report and documentation.
What is included in a clinical report?
Any relevant clinical information is also included such as a change in condition, adverse findings or events, patient outcomes, clinical investigations, and other relevant aspects. Don’t forget to close the report with companion documents. These are patient identification, nursing assessment, and legislative compliance.
How to make a good decision in a report?
Support your decision with statistics and facts. As much as possible, keep your report short and concise. The shorter the better. You need to summarize your message and write it down on the first page. Make sure to keep the body of your report as short as possible.
What Is a Nursing Incident Report?
A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side.
What Are the Information Needed in a Nursing Incident Report?
An incident report should be completed every time that an accident or any mishaps in giving care to the patient or any instances or possibilities of deviating from the normal operation and routine of the facility and/or from the patient.
What Is the Desired Outcome of Writing a Nursing Incident Report?
In writing an incident report a positive outcome should always be manifested but that depends on the event of the accident. There are times that the outcomes are deviated from what we expect and manifest. For pessimistic situations that will not happen in the future, a good, desired outcome must be manifested in writing a nursing incident report.
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Incidents happen from time to time. We cannot deny the fact that accidents of different kinds may occur or happen unexpectedly. Such cases may happen inside a hospital facility. It can happen in the operating room, wards, nurses’ station, laboratories, and even emergency rooms.
Purpose of a Nursing Incident Report
Nursing incident reports are used to initiate communication in sequencing events about the important safety information to the hospital administrators and keep them updated on aspects of patient care. Writing an incident report has its own purpose that will provide us a clearer understanding of how it works and how it is done.
How to Write a Nursing Incident Report
This is to confirm that an accident or incident has occurred that requires an incident report. Clinical reasoning and judgment must be possessed by a clinical health practitioner or any healthcare professional. It is a skill that is needed to be learned in a span of time.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes that need to be made in the facility or to facility processes to prevent recurrence of the incident and promote overall safety and quality of care.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
You Need a Nursing Brain Sheet That Works for YOU
For the longest time I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . put at closer inspection you start to see all the details and information you have available with it. From lab values, to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experience nurse.
6. Just the Boxes
I’ll be honest . . . after a couple years of being a nurse my “brainsheet” has evolved into more of a few freehand drawing on a sheet of paper. If that sounds like you, this is probably the one for you. With little more than a few suggestions . . . this is a pretty basic organizer for nurses.
What Is a Nursing Incident Report?
We know what an incident report is and what it looks like. But do we have any idea as to what a nursing incident report is and what it looks like? Is there even any difference between these two kinds of reports? A nursing incident report is a kind of report that is filled out by nurses or anyone in the health care or medical field.
How to Write a Nursing Incident Report?
Being able to know what can and cannot be written in a nursing incident report is important. Take note that this document is a formal written report, and must be treated as such all the time. So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report.
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird’s eye view of how the incident happened and what can be done to resolve it.
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything in the report and to make sure that anyone who was there is also aware of what happened. That they can assure the one reading your report that it really happened.
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details are an important part of the incident report.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
How long does a nurse brain report take?
The amount of time you have for each patient's report depends on where you work and the nurse to patient ratio, but it's usually around 5 minutes per patient. Your Nurse's Brain can function as a nursing handoff report template. If you have kept track of this information using your Nurse’s Brain, it’s easy to quickly transfer ...
What to do at the end of a nursing shift?
At the end of your nursing shift, you’ll have a short window of time to give a report to the oncoming nurse. During this transfer of responsibility, the oncoming nurse needs to know the most important information about your patients, so it’s your job to give a concise, organized report on each of them. The amount of time you have ...
Why don't you give every detail on a patient?
There are some areas you don’t need to give every detail on because they are either not relevant to the admitting diagnosis or something the oncoming nurse can easily look up . Using too much time on one patient will reduce the amount of time you have to give a report on the next patient.
Why is handoff important in nursing?
Giving a focused, efficient report is an important communication skill in nursing. Others will respect the care and organization you put in--which can improve your nursing relationships with coworkers. Giving a good report builds trust, ensures continuity of care, and improves patient safety.
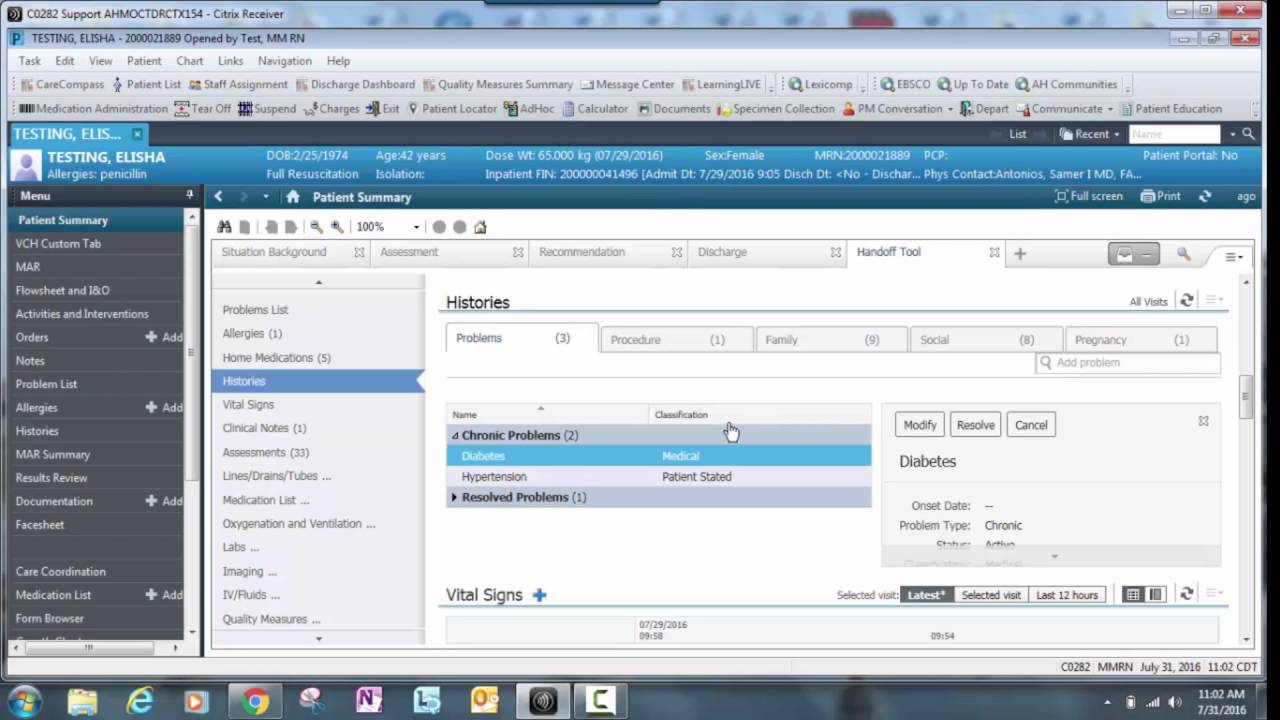
What is a nurse's brain?
RECAP: What is a Nurse’s Brain? A Nurse’s Brain, also known as a nursing report sheet, is a term for a sheet of paper that nurses use to capture important patient information and stay organized. It contains sections for key areas like patient history, diagnoses, labs, medications, body systems status, and more.
What is an end of shift report?
An end of shift report is a detailed record of a patient’s current medical status. It’s written by nurses who are finishing up their shifts and are then given to nurses who are beginning their next shifts.
Why is it important to engage with a patient during a handoff?
Engaging with a patient and their families during a handoff with an oncoming nurse ensures a safe and effective transfer between shifts.
What is nursing handoff?
Nursing Handoff: an essential yet terrifying part of your job as a new nurse. If you have ever felt overwhelmed, unprepared, or straight up shoook during handoff, you are not alone. Giving a thorough and accurate report during change-of-shift is critical for patients, but it can give any new/student nurse anxiety beyond belief.
Why is it called a brain sheet?
They are common in nursing, especially when you are just starting off, to organize your thoughts and tasks throughout the shift. Yes, it’s called a brain sheet because literally, this becomes your BRAIN.
Popular Posts:
- 1. inland hospital patient portal
- 2. omnimotions patient portal
- 3. quadramed patient portal
- 4. pma haverhill patient portal
- 5. genesis patient login
- 6. healow patient portal customer service phone number
- 7. bhshttps://bhsphysiciansnetwork.com/patient-resources/patient-portal/
- 8. sjc patient portal
- 9. aetnahealth patient portal
- 10. aiken regional patient portal