SBAR Nursing: How To Use The SBAR Method (With …
17 hours ago · In nursing, the situation, background, assessment and recommendation (SBAR) technique is a tool that allows health professionals to communicate clear elements of a patient's condition. SBAR is a communication framework that facilitates the sharing of information between team members, encourages quick response times and places emphasis on providing … >> Go To The Portal
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended. SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
Full Answer
What are the SBAR questions to ask a reporting nurse?
Although a SBAR is a great tool, the oncoming nurse should still ask the reporting nurse important questions regarding the patients status that may not be included in the SBAR. Does that patient have any family?
What is SBAR in Nursing and why is it important?
The SBAR technique is beneficial because it gives nurses a framework to communicate important details of precarious scenarios quickly and efficiently. It ensures other healthcare team members receive all the relevant information in an organized and timely manner with specific instructions on how to respond.
Can a nurse give report outside of a patient's room?
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended. SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
What are the disadvantages of the SBAR technique for bedside reporting?
This is because some nurses feel too intimidated to give recommendations to physicians. One disadvantage of using the SBAR technique for bedside reporting is when you have to wake the patients up or their families when you start the discussion.

What information should the nurse include when using SBAR?
This includes patient identification information, code status, vitals, and the nurse's concerns. Identify self, unit, patient, room number. Briefly state the problem, what is it, when it happened or started, and how severe.
What are examples of SBAR?
SBAR ExampleSituation: The patient has been hospitalized with an upper respiratory infection. ... Background: The patient is a 72-year-old female with a history of congestive heart failure and chronic obstructive pulmonary disease. ... Assessment: Patient's breathing has deteriorated in the last 30 minutes.More items...
Why is SBAR considered important for patient safety?
[7] The main purpose of SBAR technique is to improve the effectiveness of communication through standardization of communication process. Published evidence shows that SBAR provides effective and efficient communication, thereby promoting better patient outcomes.
What is the SBAR model?
SBAR is an acronym for Situation, Background, Assessment, Recommendation; a technique that can be used to facilitate prompt and appropriate communication. This communication model has gained popularity in healthcare settings, especially amongst professions such as physicians and nurses.
How do I write a nursing note SBAR?
The components of SBAR are as follows, according to the Joint Commission:Situation: Clearly and briefly describe the current situation.Background: Provide clear, relevant background information on the patient.Assessment: State your professional conclusion, based on the situation and background.More items...
What does SBAR mean in healthcare?
situation, background, assessment and recommendationCommunicating with SBAR. The SBAR (situation, background, assessment and recommendation) tool is provided below to aid in facilitating and strengthening communication between nurses and prescribers throughout the implementation of this quality improvement initiative.
What does the SBAR approach to patient safety encourage?
The SBAR approach to patient safety encourages: Consistency in assessment and practices. As a manager in a new nursing home, where might you consult for guidance and evidence to support the development of safe patient practices?
What is the purpose of the SBAR communication tool?
SBAR helps to provide a structure for an interaction that helps both the giver of the information and the receiver of it. It helps the giver by ensuring they have formulated their thinking before trying to communicate it to someone else.
How does SBAR help communication?
Widely used to standardize patient handoff practice, SBAR was first developed by the U.S. Navy to improve communication of critical information. Applied to the clinical setting, it can be used to organize information into a logical, easily recalled pattern, which expedites the handoff process and reduces error.
What is Isbar in nursing?
What is ISBAR? The ISBAR framework represents a standardised approach to communication which can be used in any situation. It stands for Introduction, Situation, Background, Assessment and Recommendation.
What is a SBAR in nursing?
What is SBAR? It’s a communication method used to promote and simplify communicating important patient information to other members of the healthcare team. The SBAR method strategically helps communicate a specific patient situation along with the patient’s background, your assessment, and possible recommendations.
Why is it important for a nurse to listen to the listener?
Furthermore, it helps the nurse focus on the problem at hand, be organized, and helps the listener determine what the nurse is trying to convey. Plus, if the listener (like the doctor) has questions about the patient that information should be easily accessible so the nurse can quickly respond to the doctor’s questions.
What is background information?
Background (focused information that the listener needs to know in order to understand the current patient problem)
What is a nurse to provider communication?
Nurse-to-provider communication. Used to help the nurse when calling to report a patient’s deteriorating condition or requesting something for the patient. Nurse-to-Nurse or other nursing staff. during transfers to other units or patient report hand-offs. It can also be used with other members of the healthcare team like physical therapy, ...
What if you don't know?
What if you don’t know? Just say you’re worried about the patient, the patient is deteriorating or unstable or has changed from their previous status etc.
Why is it so hard to give recommendations to nurses?
This can be the hardest part for some nurses because many times the nurse doesn’t feel comfortable or confident enough to give recommendations.
How to say hello to a patient?
Say hello and the listener’s name along with your name and the unit you’re on, patient’s name, room number, the patient’s current situation (why you’re calling and this should be a short sentence).
What is the most nerve wracking thing to do as a new nurse?
As a new nurse, one of the most nerve-wracking things to do is giving a handoff report to another healthcare provider, be it the next oncoming nurse, the charge nurse, the nurse who covers you on break, the doctors, and the ancillary staff . It is nerve-wracking because you don’t want to miss important information, ...
Why is handoff report nerve wracking?
It is nerve-wracking because you don’t want to miss important information, but you don’t want to give too much or too little information. Providing the right amount of information pertinent to each healthcare provider is what makes a handoff report great. While I was in school, I thought it was a little silly to repeat the information ...
How long does it take to get over COPD?
COPD is a chronic disease that takes many years to overcome if that’s even possible. Quitting smoking, getting in two 15 minute walks in a day, and healthy food will promote healing and getting to a more manageable state. see more. Show more replies. Show more replies.
What to say in the beginning of a drip?
In the beginning, say the situation, any drips, and the plan for the patient. And if you anticipate that you’ll need help from her, this is the time to speak up.
Is SBAR good for nurses?
SBAR is comprehensive and is great for the oncoming nurse. Here are the elements.
Is it good to repeat the information out loud?
But honestly, it’s good to repeat the information out loud, so you know what’s going on.
How to give a Nursing Handoff Report using SBAR
As a nursing student or a new grad nurse, one of the most daunting tasks is giving a handoff report to another nurse/preceptor or presenting to the allied health team (doctor, pharmacist, social worker, dietician, etc) during morning rounds.
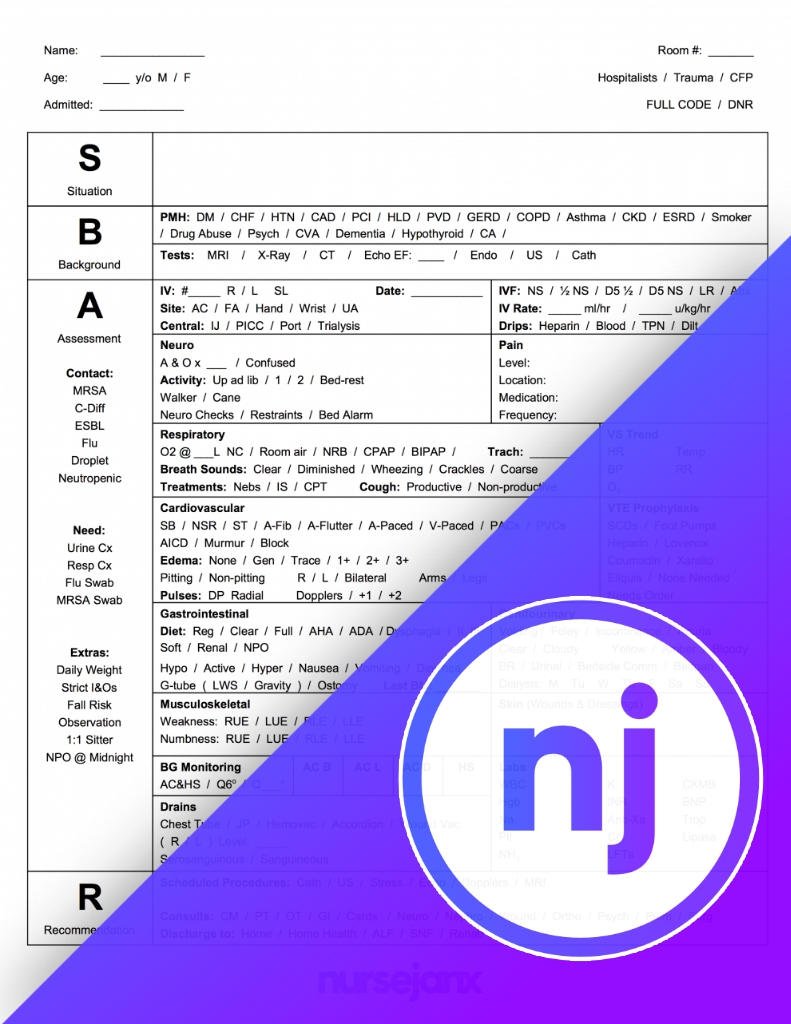
How to Create your SBAR Nurse Report Sheet
You can generate a PDF printout (just like the screenshot above) using the NurseBrain app (available on IOS and Android ).
Why is it important to get a nursing report?
Getting a good nursing report before you start your shift is vitally important. It is not only important for the nurse but for the patient as well. Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient. Nursing report is usually given in a location where other people can ...
Why do nurses give reports outside of the room?
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended.
What does SBAR stand for in nursing?
SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
What is SBAR format?
SBAR provides clinicians an effective and easy-to-use format of communication when clarity is critical to patient outcomes.
What is the most common form of communication used in nursing?
The most common form of communication you will use as a nursing student and nurse is SBAR. Developed in the US Navy, SBAR was developed to streamline and improve communication between personnel on nuclear submarines, and has been adopted by the healthcare industry as an evidence-based tool. It provides clinicians with a systematic framework ...
What medications are culprits?
Any culprit medications (such as diuretics, opioids, antihypertensives).
What happens when you walk into a guest room?
There’s a huge thunderstorm and when you walk into your guest bedroom, you see a large branch from your oak tree has fallen and broken the window. Wind and rain are coming into the room, soaking the carpet and generally ruining what had been a good night’s sleep. The guest room window is broken.
How much weight did Lee gain in 24 hours?
Mr. Lee comes into the ED with shortness of breath, a sudden weight gain of 2kg in 24 hours and dependent edema. He is speaking in three word sentences and appears to be working hard to breathe.
Can a MD return your page?
Be able to give a very brief overview of the patient’s hospital stay. The MD who returns your page, may not be the attending MD. It could be a resident or the on-call physician. Don’t assume the physician knows the patient you are calling about. Know the patient’s admitting diagnosis, when they were admitted and any significant procedures that have been done, such as surgeries or diagnostics.
What is SBAR communication template?
The use of an SBAR communication template provides you with an easy-to-remember concrete mechanism that proves useful for the framing of any conversation, especially the critical ones that require the immediate attention or action of a clinician.
What is a SBAR document?
You can use the SBAR nursing document to communicate any non-urgent and urgent patient information to other healthcare professionals like therapists and doctors. SBAR examples are typically used for: Conversations with physical therapists, physicians, and other medical professionals.
Why is the R in SBAR the weakest point?
Usually, the “R” in SBAR is the weakest point of nurses. This is because some nurses feel too intimidated to give recommendations to physicians. One disadvantage of using the SBAR technique for bedside reporting is when you have to wake the patients up or their families when you start the discussion.
What is a SBAR?
What is the SBAR? The SBAR concept was first developed by the USA Navy as a means of communicating information to nuclear submarines. Because of its success, the SBAR template got introduced to the health care system in the 1990s. The SBAR technique offers a framework of communication between the members of a healthcare team regarding ...
What is SBAR in nursing?
With an acronym that’s easy to remember, SBAR nursing is a concrete tool that can be very useful in framing conversations that require immediate attention or action, especially if they are about patients with critical status.
How to prevent negative outcomes for patients while strengthening teamwork in healthcare?
An excellent way to prevent negative outcomes for patients while strengthening teamwork in healthcare is by improving the communication between caregivers. In this aspect, SBAR examples can provide common expectations like what needs communication, how to structure communication, and what the required elements are.
Why use a SBAR template?
One such technique is the use of an SBAR tool template as this provides a framework for effective communication. As a result, it can help you create an environment that allows people to express their concerns by speaking up. Such actions can reduce the risks of adverse events and foster a safer culture in the hospital.
Popular Posts:
- 1. patient portal lakeview
- 2. mount sinai fertility patient portal login
- 3. trinity oaks family medicine patient portal login
- 4. patient portal hesperia ca
- 5. flagler medical associates patient login
- 6. madras medical group patient portal
- 7. radiology associates tallahassee patient portal
- 8. norman psychiatry patient portal
- 9. should you send a private message through patient portal
- 10. memorial health system patient portal