How to Conduct Nursing Assessment (with Examples)
12 hours ago Nurses assess patients regularly while providing care. Nursing documentation provides a clear picture of: the patient’s needs or goals, the nurses actions based on the needs assessment. the outcomes and evaluations of those actions. Every assessment is documented along with any changes to the patient’s care plan. >> Go To The Portal
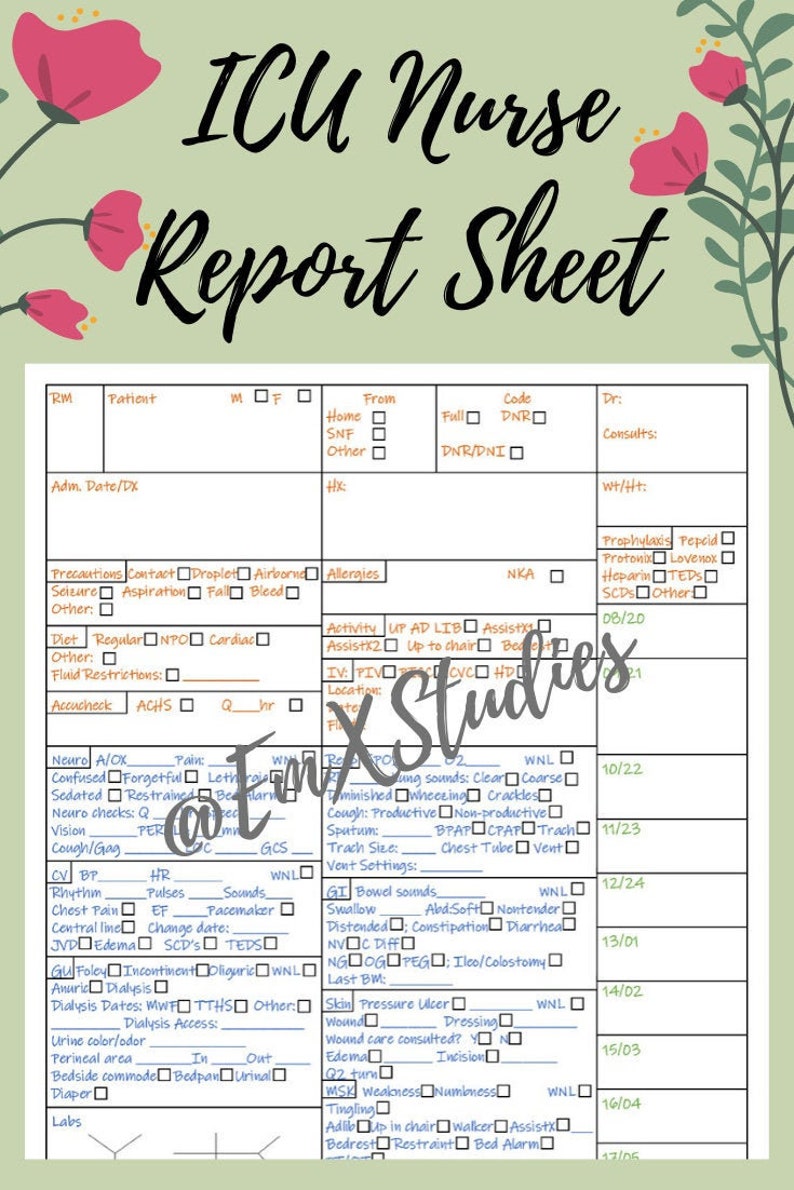
What is a nursing report?
Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient. Nursing report is usually given in a location where other people can not hear due to patient privacy.
How do you assess a patient in nursing?
You can use the head-to-toe approach, starting with the head and next and slowly progressing down to the body and examining the feet last. After preparing the assessment approach that you are going to use to assess the patient, prepare yourself, the environment, and the patient.
What should the nurse do during the assessment process?
Throughout the assessment process, the nurse should refer any serious concerns to the ANUM and to medical team. An admission assessment should be completed by the nurse with a parent or care giver, ideally upon arrival to the ward or preadmission, but must be completed within 24hours of admission.
Why is it important for a nurse to give a report?
It is not only important for the nurse but for the patient as well. Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient. Nursing report is usually given in a location where other people can not hear due to patient privacy.
What do you do when assessing a patient?
WHEN YOU PERFORM a physical assessment, you'll use four techniques: inspection, palpation, percussion, and auscultation. Use them in sequence—unless you're performing an abdominal assessment. Palpation and percussion can alter bowel sounds, so you'd inspect, auscultate, percuss, then palpate an abdomen.
What does a nurse do during assessment?
The techniques used may include inspection, palpation, auscultation and percussion in addition to the "vital signs" of temperature, blood pressure, pulse and respiratory rate, and further examination of the body systems such as the cardiovascular or musculoskeletal systems.
What are the five steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
What comes after assessment in nursing?
The nursing process functions as a systematic guide to client-centered care with 5 sequential steps. These are assessment, diagnosis, planning, implementation, and evaluation.
Why do we assess patients?
Assessments help nurses objectively identify the unique needs and concerns of each patient as well as any potential barriers to care that may affect compliance and outcomes.
How do you do nursing assessments?
0:4042:05Head-to-Toe Assessment Nursing | Nursing Physical Health ... - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo first what you want to do is you want to perform hand hygiene and provide privacy to the patientMoreSo first what you want to do is you want to perform hand hygiene and provide privacy to the patient then introduce yourself to the patient. And explain what you're going to be doing.
What are the 4 types of nursing assessments?
4 types of nursing assessments:Initial assessment. Also called a triage, the initial assessment's purpose is to determine the origin and nature of the problem and to use that information to prepare for the next assessment stages. ... Focused assessment. ... Time-lapsed assessment. ... Emergency assessment.
What is the final step of patient assessment?
Evaluation phase The final phase of the nursing process is the evaluation phase. It takes place following the interventions to see if the goals have been met. During the evaluation phase, the nurse will determine how to measure the success of the goals and interventions.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
Which action would the nurse perform in the assessment phase of the nursing process?
The assessment phase of the nursing process includes gathering data by interviewing, observing, and performing a basic physical examination of people with common health problems with predictable outcomes.
What are the 5 stages of the nursing process quizlet?
The nursing process involves five steps: assessment, diagnosis, planning, implementation, and evaluation.
How do you collect information from a patient?
You can collect patient data in several different ways — by conducting an interview in a clinical setting, by having the patient complete a paper form, or by having the patient fill out an online form. There are pros and cons to each method.
What is a nursing assessment?
A nursing assessment is a process where a nurse gathers, sorts and analyzes a patient’s health information using evidence informed tools to learn more about a patient’s overall health, symptoms and concerns. This includes considering the patient’s biological, social, psychological, cultural and spiritual values and beliefs.
What is included in a nursing assessment?
During a nursing assessment the nurse collect both subjective and objective information using evidence informed tools to assess the patient as a whole. A nursing assessment may include, but is not limited to the following:
Do I need an order to do a nursing assessment?
Nurses have the authority to perform a nursing assessment using their nursing knowledge, skill and judgment. Employer policies may provide additional direction related to nursing assessments, such as processes, tools and best practices. Nurses do not require a directive or order to perform assessments.
What should a nurse consider when determining an assessment?
A theory, framework or evidence-based tool should be used when describing the patients’ situation. Nurses should also consult the patient and other members of the health care team to create a patient-centered care plan.
When should I document my assessment?
Nurses assess patients regularly while providing care. Nursing documentation provides a clear picture of:
What is the purpose of the nursing assessment assignment?
The purpose of this assignment is to describe how a nurse assesses a patient admitted to a hospital ward. It will discuss the history of the patient, any pre-existing medical conditions and the reason they were admitted to the ward. It will also describe the hospital setting, the nursing model used, the risk assessment tools and the information collected from the assessment including the needs identified and what can be and will be done.
What are the symptoms of Ethel's fall?
Symptoms include, memory loss, disorientation and changes in personality (Ouldred, 2007). Ethel’s friend had called an ambulance immediately after the fall, and she was admitted to the ward through accident and emergency. Ethel’s fall had resulted in a fracture to the neck of femur in her left leg.
How is data collected?
Data can be collected in a number of different ways, from observing a patient, communicating with them and through their clinical notes. Collection of information can also be made through a secondary source (a relative), if, for example, the primary source (the patient) was unconscious.
What is the evaluation phase of a nurse?
In the evaluation phase of assessment, ensure the information collected is complete, accurate and documented appropriately. The nurse must draw on critical thinking and problem solving skills to make clinical decisions and plan care for the patient being assessed. If any abnormal findings are identified, the nurse must ensure that appropriate action is taken. This may include communicating the findings to the medical team, relevant allied health team and the ANUM in charge of the shift. Patients should be continuously assessed for changes in condition while under RCH care and assessments are documented regularly.
What should nursing staff discuss?
Nursing staff should discuss the history of current illness/injury (i.e. reason for current admission), relevant past history, allergies and reactions, medications, immunisation status, implants and family and social history. Recent overseas travel should be discussed and documented.
What is shift assessment?
Initial shift assessment is documented on the patient care plan and further assessments or changes to be documented in the progress notes. Clinical judgment should be used to decide on the extent of assessment required. Patient assessment commences with assessing the general appearance of the patient.
What is a structured physical examination?
A structured physical examination allows the nurse to obtain a complete assessment of the patient. Observation/inspection, palpation, percussion and auscultation are techniques used to gather information. Clinical judgment should be used to decide on the extent of assessment required.
What should be assessed during admission?
Assessment of the patients’ overall physical, emotional and behavioral state. This should occur on admission and then continue to be observed throughout the patients stay in hospital.#N#Considerations for all patients include: looks well or unwell, pale or flushed, lethargic or active, agitated or calm, compliant or combative, posture and movement.
Why is an examination of the throat and throat important?
Assessment of ear, nose, throat and mouth is essential as upper respiratory infections, allergies; oral or facial trauma, dental caries and pharyngitis are common in children. This includes a thorough examination of the oral cavity.The examination of the throat and mouth is completed last in younger, less cooperative children.
When to do musculoskeletal assessment?
A musculoskeletal assessment can be commenced while observing the infant/child in bed or as they move about their room. Be aware that during periods of rapid growth, children complain of normal muscle aches. Throughout this assessment limbs/joints should be compared bilaterally.
Purposes of health assessment
To collect data about the normal abilities of the client, risk factors that may create health problems, and current changes in the function of the health.
Framework for health assessment in nursing
Three major frameworks are there for health assessment in nursing. They are functional health work, head-to-toe framework, body system framework.
Observation techniques during a health assessment
During the health assessment nurses need to have an analytical ability to observe and interpret the non-verbal activities of the client. Non-verbal activities are important because they provide a clue to understanding the feelings. Nurses should observe the following things during health assessment:
4 Techniques of health assessment
Health assessment requires techniques, skills, and knowledge. Examiner uses his/her senses like sight, smell, touch, and hearing to gather data during physical examination. The techniques that are required in health assessment are inspection, palpation, percussion, and auscultation.
Assessment of skin, hair, and nails
Skill hair and nails have a variety of functions in the human body. Nurses need to take subjective health history of nails, skin, and hair care. To collect the required information nurse need to do an accurate assessment of skin, hair, and nails by asking questions on health practices, lifestyle, and family history.
Assessment of head and face
Take detailed history for any presence of eye problems and use COLDSPA method to get detailed information about any symptom.
Why do nurses give reports outside of the room?
If you are required to give report outside of a patient’s room try to keep your voice down so other patients and family members can not hear. Most nurses use the SBAR tool as a guide to help them give report, which is highly recommended.
Why is it important to get a nursing report before you start your shift?
It is not only important for the nurse but for the patient as well. Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient.
What does SBAR stand for in nursing?
SBAR stands for S ituation, B ackground, A ssessment, and R ecommendation.
Can family members remain in the room during CPR?
Research indicates that family members want the option of remaining in the room during procedures such as cardiopulmonary resuscitation (CPR) and that this decreases anxiety and facilitates grieving. The other options may be appropriate if the family decides not to remain with the patient. Click again to see term 👆.
Should ICU visitation be individualized?
ICU visiting should be individualized to each patient and family rather than being dictated by rigid visitation policies. Inviting the family to participate in a multidisciplinary conference is appropriate but should not be the initial action by the nurse.

Popular Posts:
- 1. dermatology associates dover patient portal
- 2. cphospital patient portal
- 3. georgia state university patient portal
- 4. fairchild patient portal
- 5. patient pursuit login
- 6. patient portal for steward health care foxboro
- 7. st vincent patient portal fishers
- 8. tms patient portal
- 9. family healthcare patient portal
- 10. doctors report for patient template