Neurological Assessment of Acute Stroke
11 hours ago Cortisol 63.6. Troponin T is 0.44. D-dimer 4388. Urinalysis this morning showed positive nitrites, rbc’s, wbc’s bacteria and protein. CT of the head this morning showed no acute intracranial abnormality. Chest x-ray showed diffuse infiltrate/edema. MRI of head showed acute/subacute infarct, medial right frontal lobe. >> Go To The Portal
The National Institutes of Health Stroke Scale (NIHSS) is used not only to assess unconsciousness but also to assess deficits and provides a standardized approach to neurological testing. An overall NIHSS score of 0-1 is normal; 1-4 is mild stroke; 5-15 is moderate stroke; 15-20 is moderate stroke; and more than 20 is severe stroke.
Full Answer
What is included in a neurologic assessment for a stroke?
Neurologic assessment 1to determine if the stroke or other acute complications are evolving. An endotracheal tube is used on patients with troubled breathing. The tube establishes if airways are clear. Hemodynamic monitoring is done to patients to monitor an increase in blood pressure.
How many stroke patients did not receive ongoing neurological care?
We have no information as to how many of the remaining patients were seen by neurologists in consultation, but it is clear that the majority of stroke patients did not receive ongoing neurological care. Why did this happen if the care neurologists provide to patients is valuable?
How can neurologists reduce the cost of stroke care?
With MCOs exerting enormous pressure to reduce the cost of medical care, neurologists need information that enhances their ability to identify all such cost-effective strategies for patients who have a stroke.
Why do we use Medicare data for stroke screening?
Because the data come from a national database, we can look at a large, diverse Medicare population, identify services regardless of site of care or provider, and track individuals during and subsequent to hospitalization for a stroke.
How do you document neurological findings?
Documentation of a basic, normal neuro exam should look something along the lines of the following: The patient is alert and oriented to person, place, and time with normal speech. No motor deficits are noted, with muscle strength 5/5 bilaterally. Sensation is intact bilaterally.
What are the 5 components of a neurological examination?
The neurologic examination is typically divided into eight components: mental status; skull, spine and meninges; cranial nerves; motor examination; sensory examination; coordination; reflexes; and gait and station. The mental status is an extremely important part of the neurologic examination that is often overlooked.
What are the 7 areas of documentation of the neurological exam?
The neurological exam can be organized into 7 categories: (1) mental status, (2) cranial nerves, (3) motor system, (4) reflexes, (5) sensory system, (6) coordination, and (7) station and gait. You should approach the exam systematically and establish a routine so as not to leave anything out.
What are the components of a neurologic exam for ischemic stroke?
There are many aspects of this exam, including an assessment of motor and sensory skills, balance and coordination, mental status (the patient's level of awareness and interaction with the environment), reflexes, and functioning of the nerves.
What is a full neurological exam?
A complete neurologic examination should contain an assessment of sensorium, cognition, cranial nerves, motor, sensory, cerebellar, gait, reflexes, meningeal irritation, and long tract signs. Specific scales are useful to improve interobserver variability.
What does a neurological exam show?
A neurological examination assesses motor and sensory skills, hearing and speech, vision, coordination, and balance. It may also test mental status, mood, and behavior. The examination uses tools such as a tuning fork, flashlight, reflex hammer, and a tool for examining the eye.
How do nurses measure neurological status?
A thorough neurologic assessment will include assessing mental status, cranial nerves, motor and sensory function, pupillary response, reflexes, the cerebellum, and vital signs. However, unless you work in a neuro unit, you won't typically need to perform a sensory and cerebellar assessment.
What is the most reliable indicator of a patient's neurologic function?
A patient's mental status is the most reliable indicator of brain function, so when there is altered mental status, obtaining a history and assessing for cerebellar function, weakness and paresthesia becomes far more difficult.
What are the three components of a neurological exam?
The cranial nerve exam tests the sensory and motor functions of each of the nerves, as applicable. Two major sections, the sensory exam and the motor exam, test the sensory and motor functions associated with spinal nerves. Finally, the coordination exam tests the ability to perform complex and coordinated movements.
What neurological assessments do you use to identify a stroke?
There are multiple scales that are commonly used worldwide in the assessment of stroke victims, including the five listed below:National Institutes of Health Stroke Scale (NIHSS)Cincinnati Prehospital Stroke Scale (CPSS)Face Arm Speech Test (FAST)Los Angeles Prehospital Stroke Screen (LAPSS), and.More items...
How do you evaluate a stroke patient?
Some of the tests you may have include:A physical exam. Your doctor will do a number of tests you're familiar with, such as listening to the heart and checking the blood pressure. ... Blood tests. ... Computerized tomography (CT) scan. ... Magnetic resonance imaging (MRI). ... Carotid ultrasound. ... Cerebral angiogram. ... Echocardiogram.
What are the four components of a rapid neurological assessment?
Rapid Neurological Exam ChecklistEyes - Can patient see, is vision normal, is eye movement normal.Hearing - Can patient hear equally in both ears, is hearing normal.Smell - Can patient smell (coffee, peppermint, etc.)Facial Muscles - Is the face equal in muscle tone and control, have patient smile.More items...
How do you pass a neuro psychiatric exam?
5 tips to pass the neuro-psychiatric examFollow the instructions. The ability to follow instructions is an important aspect of everyday life. ... Be honest and true with your answers. ... Practice a little bit of drawing. ... Improve your English language skills. ... Be confident in the interview.
How do you do a neurological exam quickly?
0:382:04Quick neurological exam for primary care - YouTubeYouTubeStart of suggested clipEnd of suggested clipWith their feet together both the front foot and the back of the foot touching not standing toMoreWith their feet together both the front foot and the back of the foot touching not standing to attention. Please can you stand with your feet together. And close your eyes.
When is a neurological assessment appropriate?
A neuro assessment is conducted if a person has experienced trauma or head injury, or reports a range of symptoms that may include dizziness, blurry vision, confusion, or difficulty with motor functions. This is done to detect neurological damage or disease.
Why is it important to analyze the results of prospective controlled trials?
Most of us are accustomed to weighing therapeutic decisions by analyzing the results of prospective controlled trials. Because the collection of that kind of primary outcome data is very time consuming and expensive, health-service researchers and managed care organizations (MCOs) also rely on less expensive secondary data sources, such as the Medicare administrative data that serve as a basis for this report. Unfortunately, there are disadvantages to using administrative data sets to analyze the nation's healthcare investment. To avoid drawing unsubstantiated conclusions from the data, it is important that we consider alternative explanations for the observations.
Why is retrospective analysis of management decisions useful?
Although prospective controlled studies will always be the gold standard for comparing alternative therapies, retrospective analysis of management decisions in large, unselected populations is useful in helping to define current medical practice.
Do neurologists treat stroke patients?
A neurologist was listed as the attending physician for only 11.3% of the stroke patients in this study, but in another 24.7% of patients a neurologist and primary-care physician both billed for routine hospital visits. Not unexpectedly, fewer stroke patients were cared for by neurologists in community hospitals than in larger medical centers, but even within the centers many patients were not followed up by neurologists. We have no information as to how many of the remaining patients were seen by neurologists in consultation, but it is clear that the majority of stroke patients did not receive ongoing neurological care. Why did this happen if the care neurologists provide to patients is valuable? Since the patients all were treated in US hospitals, researchers did not influence practice or introduce any selection bias. This snapshot of American stroke treatment should be most disturbing to those stroke victims who did not have the benefit of ongoing neurological care if, in fact, neurologists provide value-added services.
What is a thrombotic stroke?
Thrombotic. Thrombotic stroke is caused when blood clots (thrombus) form in the arteries that supply blood to the brain. The blockage may be as a result of plaque or fatty acids build up causing atherosclerosis or other arterial conditions. Embolic.
What causes a reduction in blood flow in the brain?
Majority of stroke patients suffer from an Ischemic stroke. The arteries to the brain become narrowed or blocked, this causes substantial reduction of blood flow in the brain.
What is a mild stroke called?
Some stroke patients might experience a temporary disturbance of blood flow to the brain causing a mild stroke also referred to as Transient Ischemic (TIA). Most of the transient coronary stroke patients do not suffer from permanent brain damage. 1.
What is a stroke caused by a blocked artery?
There are two leading causes of stroke. When a blocked artery causes stroke, it is referred to as an Ischemic stroke. If the cause is bursting or leaking of blood vessels in the brain, it is called a Hemorrhagic stroke. Some stroke patients might experience a temporary disturbance of blood flow to the brain causing a mild stroke also referred ...
What is a nursing assessment for stroke patients?
NURSING ASSESSMENT FOR STROKE PATIENTS. Stroke is a chronic or acute condition that affects the brain cells and tissues. It can be as a result of a blocked blood vessel that deprives a section of the brain of oxygen or a ruptured vessel that bleeds on brain tissue. In both instances, the condition causes damage to the affected tissue.
What is an embolus?
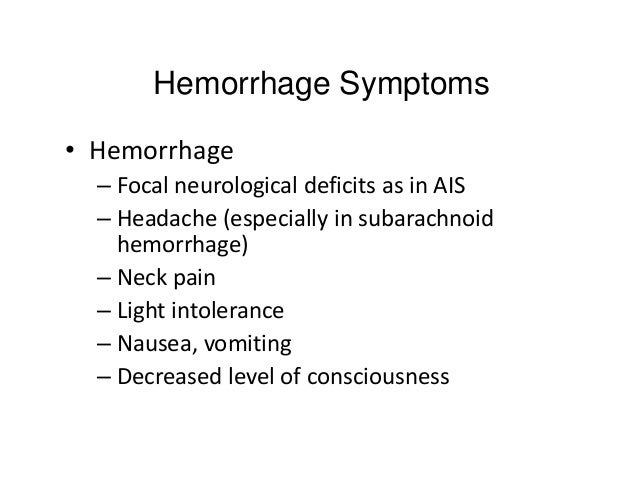
Embolus involves a blood clot or other debris formed in other parts of the body. These clots are swept through the bloodstream and deposited in narrower brain arteries causing a blockage. 2. Hemorrhagic stroke. It refers to when the blood vessels in the brain rupture and start leaking blood into the brain tissues.
Why should special care be given to stroke patients?
Special treatment and care should be given to the patients especially during recovery to avoid recurrent attacks or further complications. Specialized care for stroke patients include
What was the CT of a 20 year old man with no history of stroke?
A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
How long does it take to get a CT to a neurologist?
Door to neurologist –0 minutes Door to CT first slice –10 minutes Door to needle –17 minutes Door to groin puncture –52 minutes Door to recanalization –113 minutes Symptom onset to recanalization –205 minutes
What stem is occlusion in CTA?
The CTA shows an occlusion of the left MCA stem .
What was aspirated from the ICA?
A large thrombus was aspirated from the ICA.
Which hemisphere does CT show hypoperfusion?
CT perfusion images show hypoperfusion to the right hemisphere.

Popular Posts:
- 1. www.dmgnc.com ema patient portal
- 2. hudson valley cardiovascular practice patient portal
- 3. narmc clinic patient portal
- 4. spruce multispecialty group patient portal
- 5. cfhc patient portal login
- 6. sumitt health patient portal
- 7. site:southgatemedicalgroup.com southgate medical patient portal
- 8. patient portal wake internal
- 9. up health system marquette patient portal
- 10. sign in to patient portal at lake medical imaging, the villages, fl