4+ Nursing Bedside Shift Report Templates in PDF
28 hours ago Nurse Bedside Shift Report (Implementation Handbook) Guide to Patient and Family Engagement 4 :: • Time management and accountability between nurses. After implementing bedside shift report, nurses have reported a better ability to prioritize their work or cases during their shift and an overall decrease in staff time. 4,6 One study >> Go To The Portal
Are there any templates available for designing the bedside shift report?
We have structured several templates on the bedside shift report that you might use for designing your nursing report. Check them out today! 1. Nursing Bedside Shift Report Template 2.
What is a nurse bedside shift report?
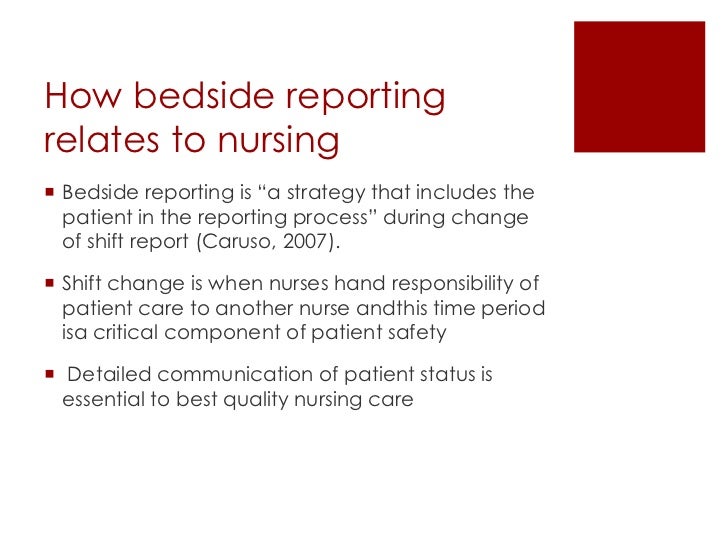
Nurse shift changes require the successful transfer of information between nurses to prevent adverse event s and medical errors. Patients and families can play a role to make sure these transitions in care are safe and effective. This handbook gives you an overview of and a rationale for nurse bedside shift report.
How does bedside shift impact patient satisfaction?
Implementation of bedside shift report increased patient satisfaction. By involving the patients in their plan of care and keeping all caregivers updated on that plan, patients feel more secure, and are more likely to participate in their own care and follow recommended health care options.
What should be included in a shift report?
You should record their name, age, address, contact details, etc. It can help you to take care of the patients according to their health condition. The shift report should explain and detail about the patient’s experience with the services provided by the bedside.

What should be on a bedside shift report?
According to AHRQ, the critical elements of a BSR are: Introduce the nursing staff, patient, and family to each another. Invite the patient and (with the patient's permission) family to participate. The patient determines who is family and who can participate in the BSR.
How do you write a good shift report?
5 Tips for an Effective End-of-Shift ReportGive a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
How do I write a nursing shift report?
It should include the patient's medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
What should a handoff report include?
Nurses complete their handoff report with evaluations of the patient's response to nursing and medical interventions, the effectiveness of the patient-care plan, and the goals and outcomes for the patient. This category also includes evaluation of the patient's response to care, such as progress toward goals.
How do you write a patient report?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
Why should nurses do bedside report?
Bedside shift report (BSR) enables accurate and timely communication between nurses, includes the patient in care, and is paramount to the delivery of safe, high quality care.
How do you organize a nursing report sheet?
0:2711:10How to Organize a Nursing Report Sheet - YouTubeYouTubeStart of suggested clipEnd of suggested clipName I always do their last name first followed by their first name since that's how all the medicalMoreName I always do their last name first followed by their first name since that's how all the medical documents always have it and I usually capitalize.
What is a SBAR handoff report?
Fortunately, there's a system in place to organize your nursing handoff report in a systematic and concise manner. This system is called the SBAR method. SBAR stands for Situation, Background, Assessment and Recommendation.
What is SBAR template?
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
What is the goal of a bedside shift report?
The goal of the Nurse Bedside Shift Report strategy is to help ensure the safe handoff of care between nurses by involving the patient and family. The patient defines who their family is and who can take part in bedside shift report.
What is the guide to patient and family engagement in hospital quality and safety?
The Guide to Patient and Family Engagement in Hospital Quality and Safety is a resource to help hospitals develop effective partnerships with patients and family members with the ultimate goal of improving multiple aspects of hospital quality and safety.*
What is a shift report?
STANDARDIZING communication during patient handoff (shift report) is one of the 2006 National Patient Safety Goals established by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO). To meet this goal, nurses in one of our hospital's medical/surgical units decided to adopt a standardized template for handoffs between shifts. The nurse-manager asked me to investigate nursing literature and find a handoff system that would comply with JCAHO standards and unit goals.
What is intershift handoff?
Performed properly, intershift handoff lets nurses share essential information about patients with the colleagues who'll be accepting responsibility for them, ensuring continuity of care. Performed poorly, though, handoff can convey inappropriate or incomplete information and waste everyone's time.
What does "shift report" mean?
When we say “shift”, it means a change of place, position or movement of a certain person or thing.
Where is the header on a medical report?
Header – the header is placed in the upper right portion of the paper together with the date of when the report was made.
Why should shift reports be honest?
It depends on the type of format a company uses. Shift reports should be honestly made because at the end of the day, it will still be checked by your managers. It must be supplied with the right number of details regarding your daily work.
What does "shift" mean in a job?
When we say “shift”, it means a change of place, position or movement of a certain person or thing. Submitting a shift report is also an effective tool in communicating to your employers.
Can shift reports be manipulated?
Shift reports can also be manipulated or tampered. If the quality of report is different from others, it might be difficult for the receiver to understand the entirety of it. Here are some ideas for what to include in your end-of-shift report to oncoming nurses.
What is shift change report?
Therefore the communication between nurses about the patient is recorded and is called as a shift change report.
How to have a smooth shift change?
Reporting is the best way to have a smooth nursing shift change. Oral communication may not always help. One or two emergency cases can be reported orally to the oncoming nurse for providing immediate care. However, not all can be remembered. It is a good practice to use shift change sheet as an effective communication tool in between nurse.
What time does a nurse leave a hospital?
This time varies from hospital to hospital it can be from 3 AM to 3 PM, 9 AM to 9 PM etc. However, there is a shift and of course, the nurse will leave hospital handing over the responsibility to the duty nurse. Unlike another profession, nursing job deals with people who are sick.
What is the patient identification heading?
Under the patient identification heading the patient’s name, id number given in the hospital, room number, age, gender, date of birth must be mentioned. Additional details like a patient’s father or spouse name and contact details also can be given in case if any emergency call needs to be placed by the nurse.
Do nurses feel panicked about ICU duty?
We understand that nurses feel panic about attending ICU duty. Patients in the intensive care unit need extra attention and hence nurses must be vigilant all the time. So let us see how they can use the change report sheet for their best use.