Office Evaluation of the Patient With Musculoskeletal …
15 hours ago In the office evaluation of patients with musculoskeletal complaints, the history is the most informative element. Least helpful are laboratory tests. Although erythrocyte sedimentation rate (ESR), rheumatoid factor, and other widely available tests are sensitive to the presence of rheumatic diseases, they are not specific for any of them. >> Go To The Portal
In the office evaluation of patients with musculoskeletal complaints, the history is the most informative element. Least helpful are laboratory tests. Although erythrocyte sedimentation rate (ESR), rheumatoid factor, and other widely available tests are sensitive to the presence of rheumatic diseases, they are not specific for any of them.
Full Answer
What is the approach to a musculoskeletal complaint?
The approach to a patient’s musculoskeletal complaint is a standardized, often sequential search for what can and what cannot be managed by the examining doctor. There is always an ultimate decision: rule in or rule out referable conditions.
What are common chief complaints in outpatient musculoskeletal (MSK) clinic?
Common chief complaints in outpatient musculoskeletal (MSK) clinic • Combined: common (eg, chronic MSK pain with neuropathic components involved) • Disability: restriction or lack of ability to perform an activity ( 1) • Important clues for differential diagnosis and approach to the plan
What do you look for in a physical exam for osteoarthritis?
• Quick limb and joint inspection for atrophy, masses, edema/fullness, scars/wounds, involuntary movement (tremor, myokymia, or fasciculation, etc), erythema, and so on Focal (part of joint, often superficial structure like bursal effusion) versus general (joint effusion)
How would you assess a patient with a musculoskeletal injury?
Look for swelling, bruising, wounds, and redness. Palpation should be directed at eliciting pain and localising areas of point tenderness in order to identify the problematic area. Palpation should include all bony prominences, joint margins and soft tissues, including muscles ligaments and tendons.
How do you describe musculoskeletal assessment?
A thorough musculoskeletal examination should include inspection, palpation of soft tissues surrounding the joint of interest, and assessment of both muscle strength and flexibility. First, gait should be observed. There may be an antalgic gait or a slow gait pattern because of pain in a specific joint.
What are musculoskeletal complaints?
Musculoskeletal disorders (MSD) are injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs.
What can you do to help a client with musculoskeletal problems?
How Is Musculoskeletal Pain Treated?Injections with anesthetic or anti-inflammatory medications in or around the painful sites.Exercise that includes muscle strengthening and stretching.Physical or occupational therapy.Acupuncture or acupressure.Relaxation/biofeedback techniques.More items...•
How do you assess musculoskeletal system as a nurse?
Also, a nursing health assessment of the musculoskeletal system involves palpation of the joints. Palpate the joints and assess the temperature of the skin and the muscles. Palpate for warmth, tenderness, swelling or masses. If pain or tenderness are noted, further assess to specify the joint or structure involved.
What is musculoskeletal assessment in nursing?
To assess the musculoskeletal system, you carefully inspect your patient, examining the symmetry of the joints, muscles, and bones and checking for swelling, redness, and ease of movement. Then you palpate over the joints, noting any areas of warmth or tenderness.
What are five 5 signs and symptoms of a musculoskeletal injury?
What are the symptoms of musculoskeletal pain?Aching and stiffness.Burning sensations in the muscles.Fatigue.Muscle twitches.Pain that worsens with movement.Sleep disturbances.
What is an example of a musculoskeletal disorder?
Work-related musculoskeletal disorders (WMSDs) are a group of painful disorders of muscles, tendons, and nerves. Carpal tunnel syndrome, tendonitis, thoracic outlet syndrome, and tension neck syndrome are examples.
What does musculoskeletal mean in medical terms?
Listen to pronunciation. (MUS-kyoo-loh-SKEH-leh-tul) Having to do with muscles, bones, tendons, ligaments, joints, and cartilage.
Why is it important to assess the musculoskeletal system?
The musculoskeletal exam helps to identify the functional anatomy associated with clinical conditions, thereby differentiating the underlying system involved and could correctly point towards the condition helping in early diagnosis and intervention.
How do you remember the musculoskeletal assessment?
I PASS stands for Inspection, Palpation, Active ROM (& Passive ROM), Strength, Special Tests. This is a good mnemonic for doing Musculoskeletal exams e.g. shoulder, knee, etc.
What are expected findings on assessment of the musculoskeletal system?
Normal or abnormal findings that could be elicited by observation and palpation include: symmetry/asymmetry - skin color and appearance, rash, ulcers, lack of sweating hair abnormalities - warmth and heat - Swelling including effusions, nodules, and inflammatory findings like synovial and periarticular thickening - ...
How do you describe muscle strength in nursing?
Muscle strength is graded on a 0-to-5 scale:0 no muscular contraction detected.1 a barely detectable flicker or trace of contraction.2 active movement of the body part with gravity eliminated.3 active movement against gravity.4 active movement against gravity and some resistance.More items...
What is MSK pathology?
MSK pathologies: fibromyalgia most common (MC), polymyalgia rheumatica, metabolic muscle disorders, systematic inflammatory disease (polyarthralgia), and so on
What is knowledge of the regional/surface anatomy?
Knowledge of the regional/surface anatomy: especially superficial structure (hand and foot) leading to localization of pathology
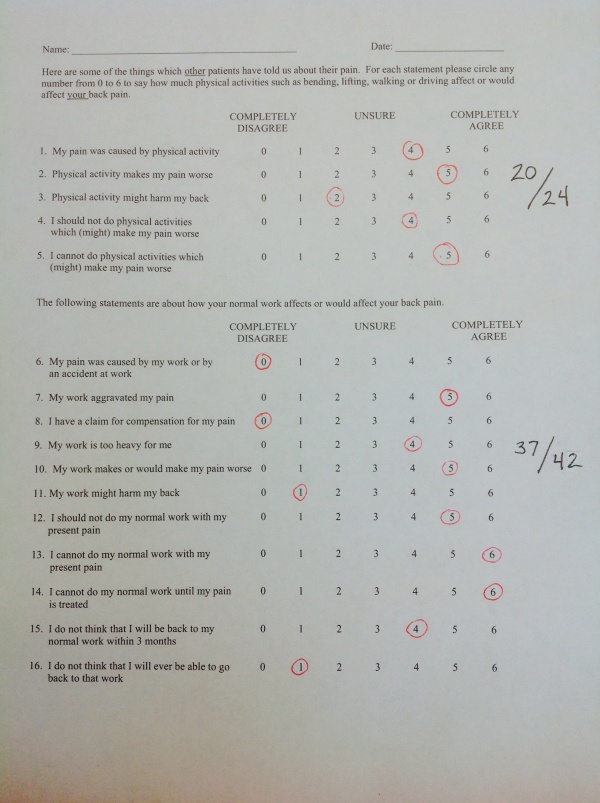
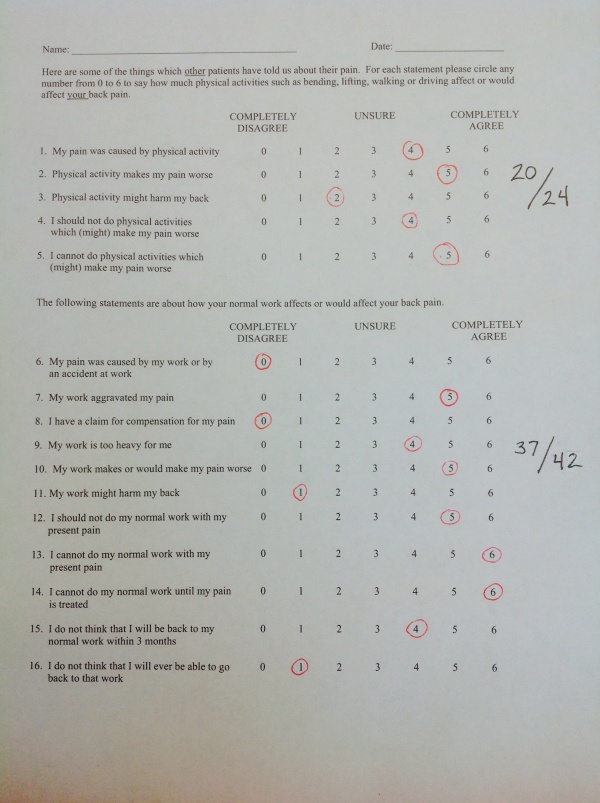
What are the psychosocial factors of low back pain?
Psychosocial factors: low social support at work, and low job control. Less job satisfaction and depressive symptoms. Patients receiving worker’s compensation with chronic low back pain have longer length of time to return to work ( 25 ).
What is knee buckling?
Knee buckling or “giving out”: lumbar radiculopathy, plexopathy, myopathy, and so on, in addition to knee pain and instability. Foot drop/slap: L4–5 radiculopathy, peroneal/sciatic neuropathy, myopathy, tendon rupture, stroke (spasticity, with vascular risk factors) and other neuromuscular disorders, and so on.
What is the difficulty with toileting, bathing, and tub transfer?
Difficulty with toileting, bathing, and tub transfer: lower extremity dysfunction (hip, knee, and ankle), upper extremity dysfunction and neurological diseases
What are the symptoms of a chronic illness?
Multiple symptoms, including pain and fatigue (very common) A history of other poorly explained chronic symptoms or syndromes: common. Irritable bowel syndrome, chronic fatigue syndrome, menorrhagia, or fibromyalgia. Mood dysfunction (depressed or anxious): common but not exclusive.
How many patients believe stress is relevant?
Only 20% of patients believe that stress is relevant (lower than patients with disease)
What happens if vertebrae are misaligned?
Misaligned Vertebrae: If vertebrae are misaligned or slipped into abnormal position, the result may be disc and/or nerve problems.
Which part of the spine is most vulnerable to pain?
The lower back, or lumbar spine, bears most of the body’s weight-making it especially vulnerable to pains and problems. Between the vertebrae are circular discs of jelly like material encased in tough cartilage. Discs facilitate movement of the spine, serving as shock absorbers and reducing friction.
Why does my shoulder blade hurt?
Pain in the shoulder blade may also be due to cervical disc trouble. It is also a common site for referred pain secondary to gall stones or a transverse humeral ligament tear or rupture. This shoulder blade pain may radiate from the shoulder blade up to the base of the skull. Pressure on the nerve that innervates the arm area from cervical disc injury can also cause pain in the shoulder, arm and chest.
Why does my back hurt?
The underlying cause of back pain is an imbalance of the bony framework of the body, especially the spinal column.
What is a ruptured disc?
Ruptured Discs: Occasionally a disc ruptures. In a rupture, the tough outer portion of the disc is torn or split and the soft inner portion then protrudes, often pressing against spinal nerves.
Can whiplash cause torticollis?
Another way of developing acute torticollis is a whiplash injury or by simply stretching. Severe neck stiffness can result, sometimes with discomfort in both arms, and pins and needles in the fingers.
Can a spinal disc be compressed?
Slipped Discs: Any of the spinal discs may be injured or degenerate. But because of their location, discs in the lower spine are subjected to the greatest weight-bearing stress and are most likely to slip or be compressed. The disc’s outer covering weakens and bulges, putting pressure on spinal nerves.