Patient Identification Techniques – Approaches, …
18 hours ago The report discusses patient identification strategies involving policies and procedures, registration, standardisation, technology, patient and family engagement, and event reporting … >> Go To The Portal
Patient identification is the process of “correctly matching a patient to appropriately intended interventions and communicating information about the patient’s identity accurately and reliably throughout the continuum of care” 1.
Full Answer
What are the implications of accurate patient identification?
Accurate patient identification may also have downstream implications for the secondary use of data for population health, quality improvement, public health, research and detection of waste, fraud, and abuse 1156. 5 Some Recommendations
What is incorrect patient identification (IPI)?
Incorrect patient identification can occur during multiple procedures and processes, including but not limited to patient registration, electronic data entry and transfer, medication administration, medical and surgical interventions, blood transfusions, diagnostic testing, patient monitoring, and emergency care.
When did the patient identification and matching final report come out?
Patient Identification and Matching Final Report PATIENT IDENTIFICATION AND MATCHING FINAL REPORT February 7, 2014 Prepared for the Office of the National Coordinator for Health Information Technology under Contract HHSP233201300029C by:
Can improving design of patient identifiers reduce misidentification?
Improving Design of Physical, Electronic, and Assigned Patient Identifiers Can Decrease Misidentification
What are 3 ways to identify a patient?
Patient identifier options include:Name.Assigned identification number (e.g., medical record number)Date of birth.Phone number.Social security number.Address.Photo.
What are the 2 patient identifiers?
The practice of engaging the patient in identifying themselves and using two patient identifiers (full name, date of birth and/or medical ID number) is essential in improving the reliability of the patient identification process.
What is the patient identification?
Patient identification is the process of “correctly matching a patient to appropriately intended interventions and communicating information about the patient's identity accurately and reliably throughout the continuum of care” 1 .
What are the 2 most important patient identifiers?
An assigned identification number (e.g. medical record number, etc). Telephone number or another person-specific identifier.
What are the 18 identifiers of PHI?
18 HIPAA IdentifiersName.Address (all geographic subdivisions smaller than state, including street address, city county, and zip code)All elements (except years) of dates related to an individual (including birthdate, admission date, discharge date, date of death, and exact age if over 89)Telephone numbers.Fax number.More items...
What are unique patient identifiers?
A unique patient identifier (UPI) is a method for standardizing patient identification. Individuals are assigned a unique code, and that code, rather than a Social Security Number, name, or address, is what is used by healthcare organizations to identify and manage patient information.
Why do we need patient identification?
Patient identification and the matching of a patient to an intended treatment is performed routinely in all care settings. Incorrect identification can result in wrong person, wrong site procedures, medication errors, transfusion errors and diagnostic testing errors.
What is positive patient identification?
Positive patient identification (asking the patient to state their name and date of birth and matching this information against the patients identification band and any other associated paperwork) is essential at every stage of the transfusion process, e.g.
How do you check a patient?
1:202:49Checking In a Patient - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd then right-click the appointment. And select check-in in a similar manner as in the scheduledMoreAnd then right-click the appointment. And select check-in in a similar manner as in the scheduled appointment tab. Or once highlighted you can click the check in button.
What are not acceptable patient identifiers?
Identifiers can be the patient's name, an assigned identification number, a telephone number or another person-specific identifier. A patient's room number or physical location is not considered an acceptable identifier.
What are some key identifiers used in healthcare?
The seven groupings of outcome measures CMS uses to calculate hospital quality are some of the most common in healthcare:#1: Mortality. ... #2: Safety of Care. ... #3: Readmissions. ... #4: Patient Experience. ... #5: Effectiveness of Care. ... #6: Timeliness of Care. ... #7: Efficient Use of Medical Imaging. ... #1: Data Transparency.More items...•
How do hospitals identify patients?
Each facility has its own protocol for identifying unknown emergency room patients that usually involves assigning the patient an identification tag with a hospital number or medical record number, but the dangers and risks of treating a patient with no identification rise precipitously in the absence of any formal ...
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
What is incorrect patient identification?
Incorrect patient identification can occur during multiple procedures and processes, including but not limited to patient registration, electronic data entry and transfer, medication administration, medical and surgical interventions, blood transfusions, diagnostic testing, patient monitoring, and emergency care.
How many people are affected by patient identification errors?
Many patient identification errors affect at least two people. For example, when a patient receives a medication intended for another patient, both patients— the one who received the wrong medication and the one whose medication was omitted—can be harmed.
How many events were eliminated by the Ecri Institute?
Of the 10,915 events, the analysts eliminated 3,302 reports that were not wrong-patient events and classified the remaining 7,613 events using the patient identification event taxonomy.
What is the 5th Deep Dive analysis of a patient safety topic?
For its fifth Deep Dive analysis of a patient safety topic, ECRI Institute PSO selected patient identification. Safe patient care starts with delivering the intended interventions to the right person. Yet, the risk of wrong-patient errors is ever-present for the multitude of patient encounters occurring daily in healthcare settings.
Why are patient identification errors so bad?
In addition to their potential to cause serious harm, patient identification errors are particularly troublesome for a number of other reasons, including: Most, if not all, wrong-patient errors are preventable.
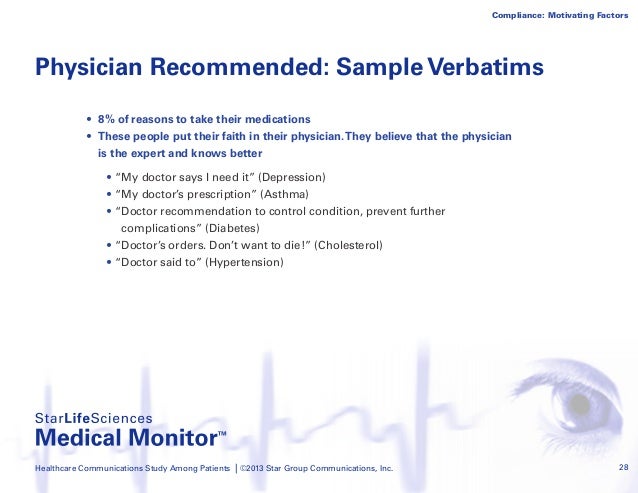
How to engage patients and their family members in patient identification?
Engage patients and their family members in patient identification by explaining the purpose of the organisation’s approach to patient identification and emphasising patients’ and family members’ roles in ensuring correct identification.
Why do you display patient names on the screen?
Display patient names on adjacent lines of a computer screen in a visually distinct manner to reduce the likelihood of selecting the wrong patient name.
What is a Patient Medical Report?
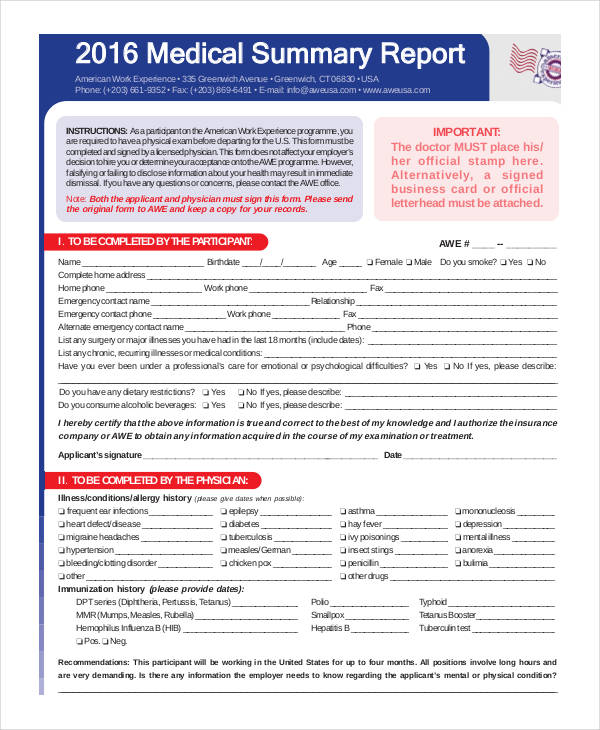
A patient medical report is a comprehensive document that contains the medical history and the details of a patient when they are in the hospital. It can also be given as a person consults a doctor or a health care provider. It is a proof of the treatment that a patient gets and of the condition that the patient has. It has the complete diagnosis on the patient, clearly stating the disease that should be treated. Through a patient medical report, anyone can analyze the health condition of a person. It sometimes contain a patient chart where the demographic profile of the patient is introduced. All types of medical records need a medical report. Patient medical records are simple data about the patient while a patient medical report is more elaborate and comprehensive. Though the importance of medical records and the purpose of medical records are almost the same with a patient medical report, the patient medical report is more beneficial. It has a complete summary of the diagnosis on the patient and have some recommendations for the health of the patient.
What should be documented in a patient's medical report?
One thing that a doctor should have documented in the patient medical report is the medical diagnosis that he has found in the patient. Whatever disease that a patient has should be clearly stated in the medical report. The name of the disease should be clearly written and some explanations about the current condition of the patient.
Why should a patient's medical report include lab results?
It is also needed because sometimes the laboratory and the test results are the proof of the sickness of the patient. For example, if the patient has a blood cancer, it can be seen with the blood tests. If the patient has a brain tumor, it can be seen through a brain CT scan. A CT scan for the body can also tell whether we have a fracture or not.
Why should medication be documented in a medical report?
The treatments or medications should also be documented because it can provide a good information about the medical history of a patient. Put the names of the medicines and tell how often did the patient takes it. You can also document its effect and tell whether it is effective for them.
What is a recommendation statement?
These are statements about the recommendations of the doctor. They are statements whether a patient can do a particular thing or not. It tell limitations on thing that they should not do for a while and it tell the abilities that they, of course, have. This is necessary so that the sickness will not get worse.
Is a medical report a legal document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patient is under your care. Thus, it can be used in court as an essential proof. So, keep a patient medical report because you may need it in the future.
Do health care providers have access to patient medical records?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report. It can be a proof if there is any doctor withholding treatments. So, to avoid conflict, the patient medical report should be shown to the patients. HIPAA (Health Insurance Portability and Accountability Act) has been passed in the Congress of United States. Passed in 1996, it specifies who can have an access to all the health information. You can research for that law, so you can have the exact details to who can have an access to a patient medical report. It is better because you can have a legal source. It can tell you all the things that you need to know about it.
What is the Patient Identification and Matching Initiative?
The Patient Identification and Matching Initiative, sponsored by the Office of the National Coordinator for Health Information Technology (ONC), focused on identifying incremental steps to help ensure the accuracy of every patient’s identity, and the availability of their information wherever and whenever care is needed.
When was the final report of the Office of the National Coordinator for Health Information Technology?
Office of the National Coordinator for Health Information Technology Patient Identification and Matching Final Report February 7, 2014
How many attributes are needed for patient matching?
While some health systems indicated that they only require three or four very stable data attributes to achieve high quality matching, several with deep experience in patient matching methods noted that they are better served by a larger number of attributes, no matter what those attributes are. For example, Geisinger Health System collects a long list of demographics that are separated into fields: first name, middle name, last name, date of birth, gender, whole social security number, street address, city, state, ZIP, and phone.
When did 1ONC start patient matching?
1ONC formally launched the Patient Matching Initiative in September 2013.
When was the 2014 HHSP233201300029C prepared?
February 7, 2014 Prepared for the Office of the National Coordinator for Health Information Technology under Contract HHSP233201300029C by:
Who created the ONC report?
This report was created by Audacious Inquiry, LLC under a contract with the Office of the National Coordinator for Health Information Technology (ONC). The content, views, and opinions do not necessarily reflect those of the Department of Health and Human Services or ONC.
Why is matching records so complicated?
Matching records to the correct person becomes increasingly complicated as organizations share records electronically using different systems, and in a mobile society where patients seek care in many healthcare settings. Many healthcare organizations use multiple systems for clinical, administrative, and specialty services, which leads to an increased chance of identity errors when matching patient records. Additionally, many regions experience a high number of individuals who share the exact name and birthdate, leading to the need for additional identifying attributes to be used when matching patient records.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is 62 percent of incidents not reportable?
Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements. Because of this, the first step to incident management in any healthcare facility is writing strong, clear reporting requirements. Then, staff can submit reports that help correct problems of all types.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What is a harmful incident?
A harmful incident results in injury or illness to a patient or another person. For example, a patient could fall out of bed and break their arm or scratch a nurse as she takes their temperature.
What Is Patient Incident Report?
Medical events can occur for a variety of reasons. Simply put, the medical system views each incident to be something that poses a threat to the health of patients or medical staff members in some way. “Incident Reporting in Healthcare,” as described in the realm of healthcare, is defined as the process of obtaining incident data and accurately presenting it for action. A newly discovered problem is recognized in order to aid in the identification and correction of the mistakes that occur. An incident report can be filed by a designated staff member (someone who has been granted permission to file reports) or by an employee who has witnessed the incident firsthand. The majority of the time, a nurse or other staff member will file a report within 24 to 48 hours of the incident occurring. It is preferable to capture and document an occurrence as soon as it occurs in order to achieve the best possible outcome.
What is the best way to write a patient incident report?
For example, employing precise and simple language will make the inquiry process more efficient and less time-consuming overall. Additionally, appropriate grammar, spelling, and punctuation should be used. Grammar errors can distort the interpretation of details contained within the report, making it more difficult to conduct an investigation into the incident.
What is a negative incident?
A Negative Occurrence: The effect of a detrimental incident is the injury or illness of a patient or another individual. It is possible for a patient to tumble out of bed and break their arm, or for a nurse to scratch them when she is taking their temperature. Missed the Mark by a Hair: A near miss occurs when there was a possibility for injury to a patient or when another person was on the verge of being harmed, but the situation was rectified before the harm could occur. For example, a patient may be apprehended while attempting to leave the facility early or may trip, but a nurse will grab them before they are injured. An incident with No Harm: A no-harm occurrence occurs when something happens to a patient or to another person, but no observable injury or illness results as a result of the event. For example, a patient may be given a blood transfusion intended for another patient, but no harm is done because the blood is compatible with the other patient.
What is incident reporting?
Incident reporting is usually used as a catch-all word for all-volunteer patient safety event reporting systems, which rely on persons who are directly involved in the events to provide specific information about what happened.
Why is incident reporting important?
The ultimate purpose of incident reporting is to improve the safety of the patient. By promoting higher safety standards and decreasing medical errors, incident reporting helps you create a more stable environment for your patients to flourish in. When your hospital provides high-quality patient care over time, it will eventually develop a positive reputation.
Why do medical incidents go unreported?
When an occurrence results in a person’s harm or property damage, it is necessary to file an incident report. Unfortunately, for every medical error that is recorded, there are about 100 other errors that go undetected. There are a variety of reasons why medical accidents go unreported, but one of the most common is a lack of knowledge on when to file a report.
How can hospitals improve their efficiency?
It is also possible to improve the efficiency of healthcare operations by using reporting tools. Hospitals can keep themselves out of legal issues by acquiring and evaluating incident data on a daily basis. A comprehensive medical error study analyzed the medical systems of 17 countries in Southeast Asia and investigated how inadequate reporting raises the cost burden on healthcare institutions and providers.
What is patient misidentification?
Patient misidentification is a medical error experienced across all medical departments and avoiding these errors requires far-reaching preventive strategies.
How to reduce identification errors?
A joint ED/Radiology workgroup to explore ways to improve the safety and efficiency of transport between ED and Radiology also could be established. Utilizing the electronic medical record to flag patients who are ready to be scanned could decrease errors as well. Use of bar code scanners to decode the patient's wristband and confirm their identity before performing a procedure, as is done in some hospitals, could additionally reduce errors.
What was the event 4 of the EKG?
Event #4 was a 21-year-old female patient seen in the ED. While receiving an electrocardiogram (EKG), this patient was found by the EKG technician to have another patient’s ID band on her wrist. The ID band belonged to a 60-year-old male and had been placed on the patient by the triage nurse.
Why do you need to increase staffing for CT scans?
Increasing staffing for CT during busy times in the late afternoon and evening would help maintain throughput without compromising patient identification in the CT suite . Another possible solution is to have a technologist in another area process CT images to improve the safety and efficiency of scanning. Furthermore, the pre-scanning workflow could include an uninterrupted pause for a designated staff member to perform the final check process, confirming the patient's name and medical record number (MRN).
How to improve communication between ED and CT?
To improve communication between the ED and CT suite, a cultural shift away from using room numbers to identify patients can be implemented. Instead, the name and MRN can be used during all communications and before transporting patients. A joint Radiology/ED workgroup, established to improve coordination, communication, and safety of transport between departments, should report back on progress made on a regular basis to ensure a feedback loop for any implemented changes. Assigning responsibility to a staff member for coordinating this workflow is essential to success.
Who funded the 75Q80119C00004?
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality ( AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Is double checking a patient's identification a safety precaution?
Both the Joint Commission Universal Protocol and the WHO Surgical Safety Checklist recommend double -checking identification as a critical precaution. 11 A perfect solution is yet to be found and, especially as technology advances, more active research is needed to find additional innovative solutions.
When should staff verify patient identification?
Staff should verify patient identification upon every encounter that requires confirmation, not just at the onset of care delivery that day – even in facilities where nurses and doctors feel they “know” their patients.
What are some examples of patient identification errors?
Here are some examples of patient identification errors that occurred in last 5 years: A blood labeling error leads to a deadly transfusion.
Why would it be upsetting if you were given the wrong medication?
Needless to say, it would be upsetting if you were given the wrong medication because a nurse confused you with another patient. Even worse, what if a surgeon performed a procedure on you that was meant for another patient? Patient identification errors are the reason health care providers check your wristband and ask for you to confirm your identity before you receive a test or treatment.
How many identifiers are needed for a patient?
Checking at least 2 patient identifiers—usually, name and date of birth, although some providers use a medical record number or another identifier. Checking bar-coded identification information on a patient’s wristband against information on a medication label or the patient’s medical record.
What did the clerk ask the patient to confirm on his wristband?
As a patient checked in for chemotherapy treatment, the clerk asked the patient to confirm the information on his wristband. Although the patient confirmed his identification, he did not notice that the information was for a patient with the same name, but a different birth date.
How many alerts did the doctor override?
Tragically, the doctor overrode 22 alerts triggered by the electronic record system. Although the pharmacy and/or nurses could have intervened and prevented this deadly medication error, it was ultimately the doctor’s mistake.
Why is the US not adopting electronic health records?
In a 2016 STAT article, author John McQuaid explains that the US is far from adopting this solution due to many factors, including privacy and security concerns, political resistance and the widespread use of electronic health records that can’t communicate with each other.
How does ID affect patient care?
Patient identification (ID) errors can disrupt care and harm patients in virtually every facet of clinical medicine, from diagnostic testing to medication administration and even billing. Recognizing the magnitude of this problem, The Joint Commission has named improving the accuracy of patient ID as the most important National Patient Safety Goal since 2014.1In recent years, awareness of the increased prevalence of identity theft and its potential clinical and financial ramifications has exposed additional challenges to confirming patient identity. Steady implementation of computerized order entry (CPOE) systems, electronic health records (EHRs), and bar coding systems has allowed for increased detection and tracking of near misses and actual patient ID errors; it has also highlighted the role health information technology (IT) can play in preventing, but also contributing to ID errors. Such assessments have underscored the complexity of the problem because errors can be introduced by myriad factors at any step of medical care. For instance, mistakes leading to serious medication errors arise during each step of clinical workflow with one-third occurring during order entry, one-third during transcription/dispensing, and one-third during administration.9Studies suggest providers override between 49% and 96% of alerts that arise during order entry.3Given the demanding pace of work many healthcare staff face, designing effective interventions will require attention to impact on workflow. In 2013, ECRI Institute convened the Partnership for Health IT Patient Safety and its component, single-topic focused workgroups. The Patient ID workgroup is a multistakeholder workgroup of 45 providers, researchers, information technology experts, healthcare and patient safety organizations, vendors, and a patient safety advocate. In November 2015, the workgroup began to consider how best to address patient ID errors, beginning with a review of all reported ID events. In conjunction with the workgroup initiative, we performed a literature review, to provide an up-to-date understanding of problems and interventions that have been assessed in the literature. Specifically, we addressed the following key questions:
How many clinicians report charting or entering orders on the wrong patient within the prior 3 months?
At a single U.S. Yamamotoinstitution’s emergency department, 97% of clinicians (66 of 68) reported charting or entering orders on the wrong patient within the prior 3 months.
Why are specimen labels unclear?
specimen labels were often unclear due to small font size along with inadequate demarcation between labels printed for different patients. Notably, the majority of identified design flaws could be addressed with relative ease, and in fact, studies often reported that redesigned wristbands were well received by staff and that increased usability may have contributed to increased adherence to ID protocols. Interventions for altering electronic or assigned identifiers were similarly somewhat straightforward. We identified studies that reported decreased ID errors after display of patient photographs along with other identifiers in the EHR3and radiology films.4A new naming convention for neonates designed to be more distinctive also decreased wrong-patient orders.5The relative simplicity of these varied interventions (e.g., larger wristband size, using different ink, adding a photograph) suggests that important strides towards reducing identification errors may be achieved with fairly basic, low-technology measures so long as they reflect smart, thoughtful design. If ID protocols are not being followed, institutions should consider seeking feedback from staff, and minor alterations in design may prove helpful.
What is a special report on ECRI?
This Special Report presents a literature review and is designed to provide a snapshot of the status of this issue at the time literature searches and literature review were conducted. The information contained herein is derived primarily from the available, published, peer-reviewed scientific literature and searches of the World Wide Web. Publications referenced are limited to the English language. The conclusions and recommendations must be interpreted cautiously and judiciously. ECRI Institute implies no warranty and assumes no liability for the information, conclusions, and recommendations contained in this Special Report. The conclusions and recommendations and the studies on which they are based are highly perishable and reflect the state of the issue at the time at which the report was compiled. The report was produced and updated by a multidisciplinary staff of scientists, clinicians, information specialists, medical writers, and other health professionals. For quality assurance, all reports are subject to review by experts within ECRI Institute and one or more selected external experts. Neither ECRI Institute nor its employees accept gifts, grants, or contributions from, or consult for medical device or pharmaceutical manufacturers. The Health Technology Assessment Information Service (HTAIS) provides this Special Report and many other forms of information support to help governments, hospitals, health systems, managed care organizations, health insurers, health professionals, and the public meet the challenge of evaluating healthcare technology and issues objectively and rationally. HTAIS is a service of ECRI Institute, a nonprofit health services research agency. ECRI Institute has been designated an Evidence-based Practice Center by the U.S. Agency for Healthcare Research and Quality. ECRI Institute’s mission is to provide information and technical assistance to the healthcare community worldwide to support safe and cost-effective patient care. The results of ECRI Institute’s research and experience are available through its publications, information systems, databases, technical assistance programs, laboratory services, seminars, and fellowships. All material in this Special Report is protected by copyright, and all rights are reserved under international and Pan- American copyright conventions. Subscribers may not copy, resell, or reproduce information from this Special Report (except to print out or email single copies of reports for authorized use) by any means or for any purpose, including library and interlibrary use, or transfer it to third parties without prior written permission from ECRI Institute.
What are patient ID errors?
Patient identification (ID) errors can disrupt care and harm patients in virtually every facet of clinical medicine, including diagnostic testing, medication administration, and even billing. Recognizing the magnitude of this problem, The Joint Commission has named improving the accuracy of patient ID as the most important National Patient Safety Goal since 2014.1In 2013, ECRI Institute convened the Partnership for Health IT Patient Safety. In support of ongoing work performed by the Partnership’s Patient Identification Workgroup, we performed a literature review to provide an up-to-date understanding of problems and interventions that have been assessed in the literature. Specifically, we addressed the following key questions: 1. What is the prevalence of patient ID errors in clinical care? 2. What are causes of patient ID errors in clinical care?
What is the mislabeling rate for blood transfusion?
At various institutions, rates of specimen mislabeling for blood transfusion ranged from 0.016% to 1.12%. Grimm et al.46
How many radiology reports contain the phrase "wrong patient"?
academic hospitals, a Sadighkeyword search of 1.7 million radiology reports from over about 4.5 years, found 0.004% (67) contained the phrases “wrong patient” or “wrong dictation.” et al.32
Popular Posts:
- 1. eugene urgent care patient portal
- 2. queen city regional clinic patient portal
- 3. transylvania mission patient portal
- 4. cayuga medical center patient portal
- 5. westminster ma. meetinghouse medical group patient portal
- 6. und student health patient portal
- 7. collier blvd physician mgmnt llc patient portal
- 8. premier landmark ima patient portal
- 9. childrens mercy portal patient
- 10. how do i see records of his other doctors from mercy through his family patient portal