3+ SAMPLE Patient Medical Report in PDF
14 hours ago Step 3: Report the specimens. Whatever test and examination that you have given to the patient, have the result documented. These will be the laboratory results and test results to have an analysis of what disease could have touched the patient. There should be a clear notation how you have derived the specimens. >> Go To The Portal
What is a patient care report?
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.
What should a doctor document in a medical report?
One thing that a doctor should have documented in the patient medical report is the medical diagnosis that he has found in the patient. Whatever disease that a patient has should be clearly stated in the medical report. The name of the disease should be clearly written and some explanations about the current condition of the patient.
Why medical professionals need medical reports?
In order for medical professionalsto know a patient’s progress or medical status, creating medical reports are what they need. A medical report is an updated detail of a medical examination of a certain patient. It is a vital written document that describes the findings of an individual or group of people.
Who has the right to see the patient medical report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report.
What does normal mean in medical terms?
1. Functioning or occurring in a natural way; lacking observable abnormalities or deficiencies. 2. Occurring naturally and not because of disease, inoculation, or any experimental treatment. Used of immunity.
How do you describe patient status?
Patient is conscious, but may be uncomfortable. Indicators are favorable. Serious - Vital signs may be unstable and not within normal limits. Patient is acutely ill.
How do you write a patient summary report?
0:122:55SOAR Medical Summary Report Tutorial - YouTubeYouTubeStart of suggested clipEnd of suggested clipInclude descriptions of the applicants appearance mannerisms. And briefly describe any symptoms theMoreInclude descriptions of the applicants appearance mannerisms. And briefly describe any symptoms the applicant displays.
What should be included in a patient report?
A structured format incorporating elements of background information, medical history, physical examination, specimens obtained, treatment provided and opinion is suggested.
How do you know if a patient is stable?
If a patient's General Appearance, Level of Consciousness, and Vital Signs are all normal, the patient is stable. If possible, treatment should be rendered starting with the least invasive that is appropriate for that patient's hemodynamic status.
How would you describe a patient's general appearance?
General Appearance Considerations for all patients include: looks well or unwell, pale or flushed, lethargic or active, agitated or calm, compliant or combative, posture and movement.
How do you write a good medical case report?
Provide details of the clinical presentation and examinations, including those from imaging and laboratory studies. Describe the treatments, follow-up, and final diagnosis adequately. Summarize the essential features and compare the case report with the literature. Explain the rationale for reporting the case.
How do you write a patient case report Example?
This section provides the details of the case in the following order:Patient description.Case history.Physical examination results.Results of pathological tests and other investigations.Treatment plan.Expected outcome of the treatment plan.Actual outcome.
How do you prepare a patient report?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
What are five characteristics of good medical documentation?
What are five characteristics of good medical documentation?Accuracy In Medical Communications. One of the most important characteristics of good medical communications is the level of accuracy.Accessibility of the record.Comprehensiveness.Consistency In Medical Communications.Updated information.
What is a patient report?
A patient report is a medical report that is comprehensive and encompasses a patient's medical history and personal details. It's often written when they go to a health service provider for a medical consultation. Government or health insurance providers may also request it if they need it for administration reasons.
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
What is a patient medical report?
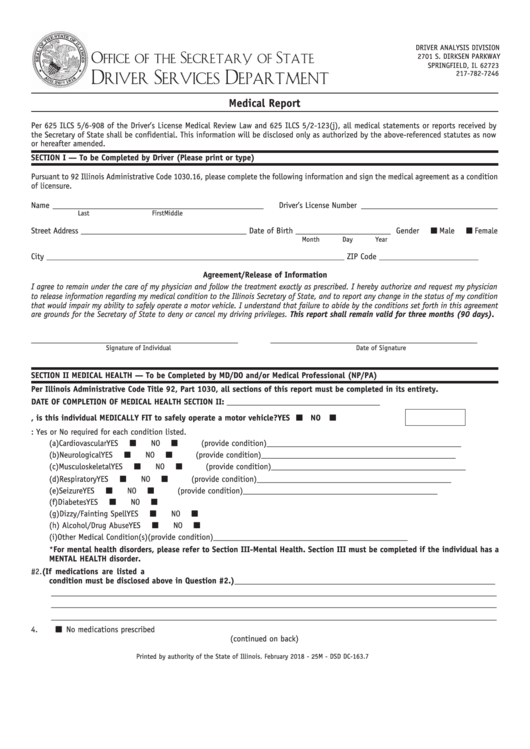
Patient Medical Report Example – This is what you need if you’re looking for a generic medical report template. This medical report targets any patient with certain illnesses, ideal for clinic or hospital use. This contains needed information such as patient’s complete name, address, contact details, questions about medical status/history, and other related medical questions.
Why are medical reports important?
This is both under their supervision and that of the patient’s other significant physicians. Medical reports can provide significant, lifesaving information to health and medical care professionals. Not just that, they can track all medical procedures performed on a patient. Therefore medical reports are essential in every medical field.
What are the different types of medical reports?
Types of Medical Report Templates 1 Patient Medical Report Example – This is what you need if you’re looking for a generic medical report template. This medical report targets any patient with certain illnesses, ideal for clinic or hospital use. This contains needed information such as patient’s complete name, address, contact details, questions about medical status/history, and other related medical questions. 2 Hospital Medical Report Template – This type of medical report is designed for hospital use. Information includes patient’s name, ward, hospital name, medical consultant, discharge summary, the reason for admission and medical diagnosis, and past medical history. 3 Medical Examination Report Example – If you’re making medical reports intended for medical examinations, perhaps you might want to download this template for more convenience. This is a complete template that targets examination reports in a medical setting. 4 Medical Incident Report Template – This type of medical report focuses on any incident or accident that may happen within a medical setting. This is filled so that recording of details about incidents that occur at the medical facility will be tracked down and certain measures or sanctions will be implemented. 5 Medical Fitness Report Template – Making medical reports for fitness progress? This template is what you need. This aims at providing a thorough and complete report for medical fitness. The template contains information such as applicant’s name, address, license number, name of the hospital/clinic who conducted the report, and questions related to medical fitness.
Why is it important to update medical reports?
In every patient’s life, change always comes, may it be a changed name, address, medical progress, or a new health diagnosis and prescription.
What is a medical incident report template?
Medical Incident Report Template – This type of medical report focuses on any incident or accident that may happen within a medical setting. This is filled so that recording of details about incidents that occur at the medical facility will be tracked down and certain measures or sanctions will be implemented.
When writing a patient's medical history, relevant medical conditions should be considered?
Thus, it can be in a report sample PDF document or report sample doc format. It is always a best practice to provide comments on specific investigations, measures, and management of the patient.
Is it a good practice to provide comments on specific investigations, measures, and management of the patient?
It is always a best practice to provide comments on specific investigations, measures, and management of the patient. However, there are times that if treatment is ongoing, an additional report may be needed.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
How to Write a Medical Summary Report?
However, in general, a medical summary report only gets difficult if you have to fill in the blanks of your summary report. To avoid doing this in the future, check out the following tips for you to get started.
What is the purpose of doing a medical summary report?
As it is not common for people in the medical field to waste time reading the whole information, a medical summary report gives out the shortened and important details.
Why is it important to write a medical summary?
The purpose of writing a medical summary report is to take out the unnecessary information and leave the important ones. For a patient’s medical history, that is important for doctors so they could give out a proper diagnosis.
Why is it important to add medical history to a patient's medical history?
This is important as this can help understand the underlying issues a patient may have. As well as any kind of illness that may have been passed on to the patient by which side of the family.
Why do we keep a copy of medical summary?
The reason for keeping copies of every medical summary report, is when you may need one to compare or to need one in general, it is there. The reason for comparing often only happens between the patient’s files. To see if there are any improvements or none at all.
Do all doctors and nurses use a medical summary report?
This depends on the doctors and nurses, but the majority often use medical summary reports to shorten the report by taking away the information that may not be as important.
How to write a response to a patient's letter?
When constructing your response, it can be helpful to constantly imagine yourself in the patient’s shoes as they read your letter, having experienced what they have, their level of knowledge about medical matters and their lived experience of the event. As you write, think about how the words you choose make them feel, add to their understanding of the situation and help them psychologically heal.
What to say to a patient who has communication issues?
Sometimes they will agree that on that occasion their professionalism slipped and they may be able to explain why (e.g. long working hours, heavy patient load or recent professional or personal distressing event). It is appropriate to tell that patient that you have spoken with the member of staff concerned and that they express regret about what happened. If the staff member outright denies any communication issue, they still need to reflect on the fact that whatever took place, it resulted in an upset patient. Sometimes differences are unresolvable, however we can still express regret at their unhappy experience.
How to write a letter of complaint?
Outline#N#The following structure may be used when writing letters: 1 Acknowledgment of the problem, impact on the individual and distress caused and apology. 2 Summary of events 3 Explanation & clarification of misunderstandings or misconceptions, and acknowledgment of deficient care if appropriate 4 Actions that will occur as a result of the complaint and investigation 5 Close with final apology and details of who to contact in the case of further questions
What do you need to know before writing a complaint letter?
Before writing the letter, you need to understand exactly what happened by accessing patient records and speaking with staff involved if possible. Is there a deficiency in care or has the complaint highlighted an area where change in practice could avoid future adverse events or dissatisfaction? Is the complaint reasonable or does the complainant have unrealistic expectations? It’s rare that there is nothing to learn from a patient who has taken the time to write a complaint and the approach to understanding the situation must be with an open mind.
When can you write a response to a complaint?
Once you have all the information and have decided a plan to address the individual’s concerns, you can write the response.
Can a patient request a written reply?
Sometimes, however, patients specifically request a written reply or decline a face-to-face meeting.
What do you want to know when you are given a medical test?
When you are given a medical test that yields relative results, usually in the form of a number (value), you will want to know what those results mean and how they compare to previous results.
Why is it important to confirm lab results?
Confirmation of your results will give you more information before you make any medical decisions and will give you confidence in the decisions you make based on those results.
What is a test that gives a yes or no answer?
Tests that give "yes" or "no" answers (usually for diagnostic purposes) Tests that give relative results (to measure high or low values compared to a "normal" range) Here is more information about these two kinds of medical tests, and the kinds of questions you'll want answered to better understand what they mean.
Why is it not possible to get a diagnosis if you are exposed to HIV?
Because the test detects proteins produced in response to the disease, rather than the disease itself , it may not be able to make an accurate diagnosis if you are tested too soon after HIV exposure. 1 . Other tests have low specificity.
Does Verywell Health use peer reviewed sources?
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
What does medical records reflect?
Medical records often reflect differing diagnoses and treatment recommendations among multiple caregivers. However, oral or written criticism of previous health care contributes nothing to the patient's needs. Patients may take casual remarks critical of prior care quite seriously, possibly destroying their relationships with previous caregivers and/or you.
What to include in a patient complaint?
Include copies of all clinically-related correspondence from and to patients, as well as notes from phone conversations and office discussions.
What is the importance of complete medical records?
Current, complete records which assist diagnosis and treatment, and which communicate pertinent information to other caregivers also provide excellent records for risk management purposes. The use of encounter forms, checklists, flowsheets, and computer-assisted documentation for high volume activities can save time and may also reduce the communication problems and errors caused by illegible handwriting. Missing, incomplete, or illegible documentation can seriously impede patient care and the defense of a malpractice claim, even when the care was appropriate. The following advice on documentation includes issues identified through analysis of malpractice claims.
What is clinically pertinent information?
The medical record is a primary mechanism for providing continuity and communication among all practitioners involved in a patient's care. To gauge adequacy of your patient's medical records, consider what you would want documented if you were assuming management of the care of a patient you did not know.
Why is it important to keep your medical records up to date?
Keep your records up-to-date in order to provide the best resource for patient care and evidence that appropriate and timely care was provided. Clinically pertinent information. The medical record is a primary mechanism for providing continuity and communication among all practitioners involved in a patient's care.
What is current complete records?
Current, complete records which assist diagnosis and treatment, and which communicate pertinent information to other caregivers also provide excellent records for risk management purposes.
What should not be documented in Massachusetts?
What should not be documented. Derogatory or discriminatory remarks. In Massachusetts, patients have the right to access both office and institutional medical records and may be sensitive to notes they view as disrespectful or prejudicial. Include socio-economic information only if relevant to patient care.
Who is notified of the disclosure of a patient's results?
The ordering physician is notified before the disclosure takes place and has access to the results as they will be conveyed to the patient/surrogate, if results are to be conveyed directly to the patient/surrogate by a third party.
What is the obligation of a physician to be considerate of patients?
Physicians have a corresponding obligation to be considerate of patient concerns and anxieties and ensure that patients receive test results within a reasonable time frame. When and how clinical test results are conveyed to patients can vary considerably in different practice environments and for different clinical tests.
How to ensure that test results are communicated appropriately to patients?
To ensure that test results are communicated appropriately to patients, physicians should adopt, or advocate for, policies and procedures to ensure that: The patient (or surrogate decision maker if the patient lacks decision-making capacity) is informed about when he or she can reasonably expect to learn the results of clinical tests ...
