Printable Med Surg Nurse Report Sheet 4 or 6 Patient …
30 hours ago ICU Nurse Report Sheet, Nurse Brain Sheet, Detailed, Printable, Digital Download. Victoria Holman May 28, 2022. Purchased item: Printable ICU Nurse Detailed Report Sheet, Nurse Brain Sheet, 1 Patient Handoff Template PDF, Digital Download. christianroselaine1 Mar 2, 2022. 10/10 drug cards. Very helpful and easy to study and read. >> Go To The Portal
What is a nursing report sheet?
When a patient has been registered for care in a healthcare institution, nurses form to be one of the primary groups in-charge of taking care of the said patients. In order to make sure that they are able to provide the optimum required care, nurses use a tool known as the Nursing Report Sheet.
What is a med surg organization sheet?
For example, the room where the patient was treated, the name of the patient, the contact of the person closest to the patient, the condition of the patient during treatment, and also the type of care received. Med surg organization sheet functions as a journal report. So that tracking can be done in patients who have just had surgery.
What is completion in a nursing report template?
Completion – Completion is the final section of a nursing report template. This section contains the details regarding the nurse on duty. The various details to be recorded here are the Name, Signature of the Nurse and the Date and Time of the ending of the shift.
Why are nursing report templates important in healthcare?
This means that, even if there is a change in the shifts of a particular group of doctors or nurses, the subsequent shift can continue providing care to their patients without any obstacles. Being such a useful and essential part in healthcare circles, these nursing report templates are implemented by institutions all around the world.
How do I write a nursing report sheet?
0:0020:45Nursing Shift Report Sheet Templates | How to Give a Nursing Shift ReportYouTubeStart of suggested clipEnd of suggested clipSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is atMoreSo to get that you can go to our website registered nurse RN comm. Go to the search bar which is at the top right and type nursing report templates or nursing report sheets.
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
How many patients are on a Med Surg floor?
Med-surg nursing is busy Many manage 5-7 patients at a time. For these patients, they are responsible for a multitude of duties, which can include: Admission/discharge.
What should be included in a nursing shift report?
Written by nurses who are wrapping up their shifts and provided to those nurses beginning the next shift, these details should include a patient's current medical status, along with his or her medical history, individual medication needs, allergies, a record of the patient's pain levels and a pain management plan, as ...
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What are 4 components of correct nursing documentation?
For documentation to support the delivery of safe, high-quality care, it should: Be clear, legible, concise, contemporaneous, progressive and accurate.
Is PCU better than med Surg?
However, overall it would be considered med/surg. PCU is not med-surg it is a step down unit, mostly considering of cardiac patients , but there are other patients with critical illnesses coming from ICU or surgery who require close monitoring or some sort of drip that is admitted to PCU.
What kind of patients do you see on a med Surg floor?
What types of conditions does a med surg nurse treat? A med surg nurse attends to the needs of patients that are: suffering from an acute or a potentially acute illness or injury; experiencing an exacerbation of a chronic condition affecting one or more body systems; and/or preparing for/recovering from surgery.
How do I become a successful med Surg nurse?
Here are some common med-surg nursing tips that you need to remember.Set the right expectations every day. ... Stay organized. ... Keep your essentials on you at all times. ... Eat right. ... Be mindful of your body. ... Take breaks when you need them. ... Ask questions. ... Recognize the signs of burnout.More items...•
What is the SBAR format?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
What is SBAR template?
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
What should be included in SBAR?
The components of SBAR are as follows, according to the Joint Commission:Situation: Clearly and briefly describe the current situation.Background: Provide clear, relevant background information on the patient.Assessment: State your professional conclusion, based on the situation and background.More items...
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
Why is it important to have an ICU nurse report?
Due to this, it is very important that nurses are able to gather the required information. To help with this situation, ICU Nursing Reports were brought into action. ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
What is a nursing report sheet?
The report sheets enable the nurses to record clear information regarding details including the diagnosis, history, allergies, consults, vital signs, lab results, and other such health-related data. Due to their excellent recording system, nursing report sheets are used by physicians, doctors, nurses and other healthcare staff all over the world. ...
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
What is the purpose of the General Information section in a nursing report?
This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient.
What is flow sheet in nursing?
A6. In simple terms, a flow sheet is a single or dual-page form, tasked with the job of gathering all important aspects of a patient’s condition. Similar to the other nursing reports, the flow sheet is tasked with gathering patient information.
What is a lab report?
Labs – Labs refers to the various patient reports which have been derived from the numerous tests conducted on the patient. The constituents of this section are Labs, Needed Labs, and Future Procedures. Completion – Completion is the final section of a nursing report template.
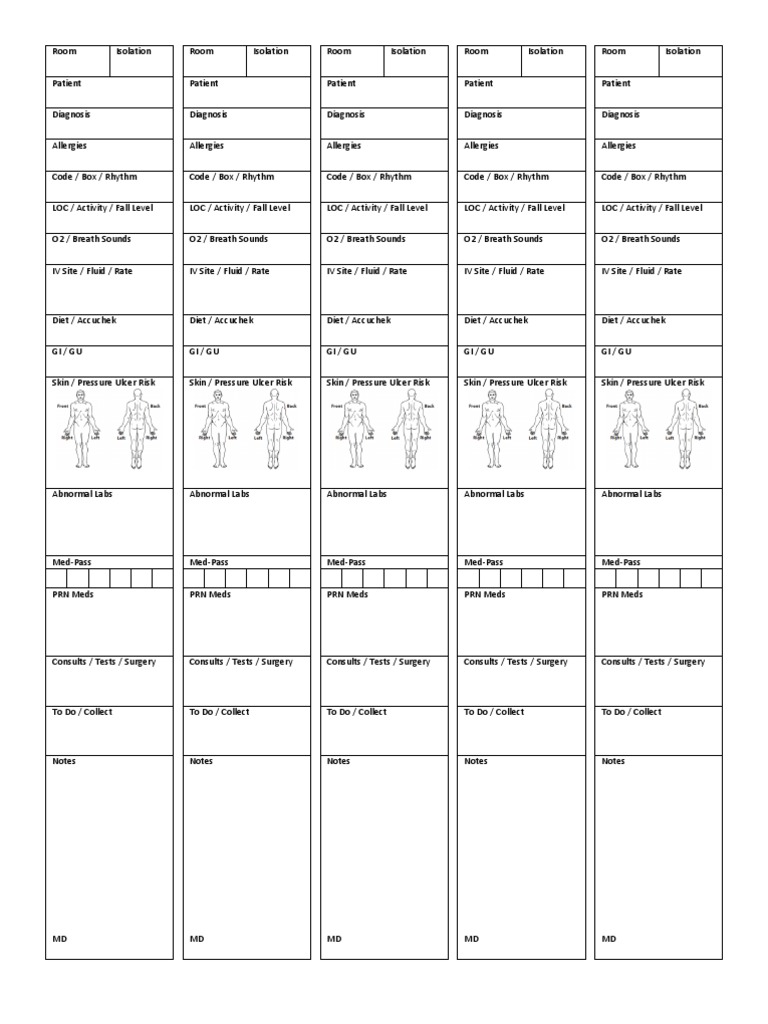
Description
Color coded to differentiate between patients. This is a patient report sheet, allows you to keep all the information organized and efficiently keep track of your patients during day or night shift. It includes all the pertinent information you may need.
More from this shop
Get 10% off your order when you spend $110 at this shop. Discount shown at checkout.
What is an organization sheet in med sg?
What a Med Surg organization sheet contains? At the Med Surg department, there are certainly organization sheets that are part of their duties. Contains data about patients in the scope of their care. For example, the room where the patient was treated, the name of the patient, the contact of the person closest to the patient, ...
What is a med sage?
Med Surg stands for medical-surgical which is a department that contains nurses specifically handling patients who need recovery after undergoing surgery. There is no specific age for patients treated by Med Surg nurses. To be sure, after undergoing surgery, patients will find it difficult to move the body and there are even some patients who need ...
Why is the knowledge possessed by each nurse so different?
The knowledge possessed by each nurse is very different because, in their studies, they have focused on one department. So that the action that can be taken by all the nurses initially is general medical knowledge.
You Need a Nursing Brain Sheet That Works for YOU
For the longest time I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . put at closer inspection you start to see all the details and information you have available with it. From lab values, to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experience nurse.
6. Just the Boxes
I’ll be honest . . . after a couple years of being a nurse my “brainsheet” has evolved into more of a few freehand drawing on a sheet of paper. If that sounds like you, this is probably the one for you. With little more than a few suggestions . . . this is a pretty basic organizer for nurses.

Popular Posts:
- 1. athenahealth patient portal 1121
- 2. my rsfh patient portal
- 3. thundermist west warwick patient portal
- 4. salil k trahan patient portal
- 5. etmc patient portal
- 6. blount memorial breast center patient portal
- 7. give me a report on an accident patient admitted at the hospital
- 8. st thomas mid town patient portal
- 9. patient portal implementation google scholars
- 10. doctor report on patient