Patient Engagement, Usability, and Meaningful Use Stage …
9 hours ago Nov 02, 2015 · The Stage 3 rules are a mixed bag for the application of patient portal software — most of the objectives and their accompanying measures seem quite attainable, but one patient engagement measure in particular could prove a significant challenge for providers. Here’s what you need to know. >> Go To The Portal
Building a meaningful use stage 3 patient portal Developing patient portal systems present significant adaptive challenges to any healthcare providers who earn payments through CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
Full Answer
What does Stage 2 meaningful use mean for providers?
Nov 02, 2015 · The Stage 3 rules are a mixed bag for the application of patient portal software — most of the objectives and their accompanying measures seem quite attainable, but one patient engagement measure in particular could prove a significant challenge for providers. Here’s what you need to know.
Is Meaningful Use Stage 3 a carrot or a stick?
Sep 14, 2021 · Building a meaningful use stage 3 patient portal. Developing patient portal systems present significant adaptive challenges to any healthcare providers who earn payments through CMS. However once implemented, a patient portal that conforms to the best practices of meaningful use it will deliver vastly improved patient care. It is not too late to achieve Stage 3 …
Are EHR incentive programs meeting Stage 2 Meaningful Use Regulations?
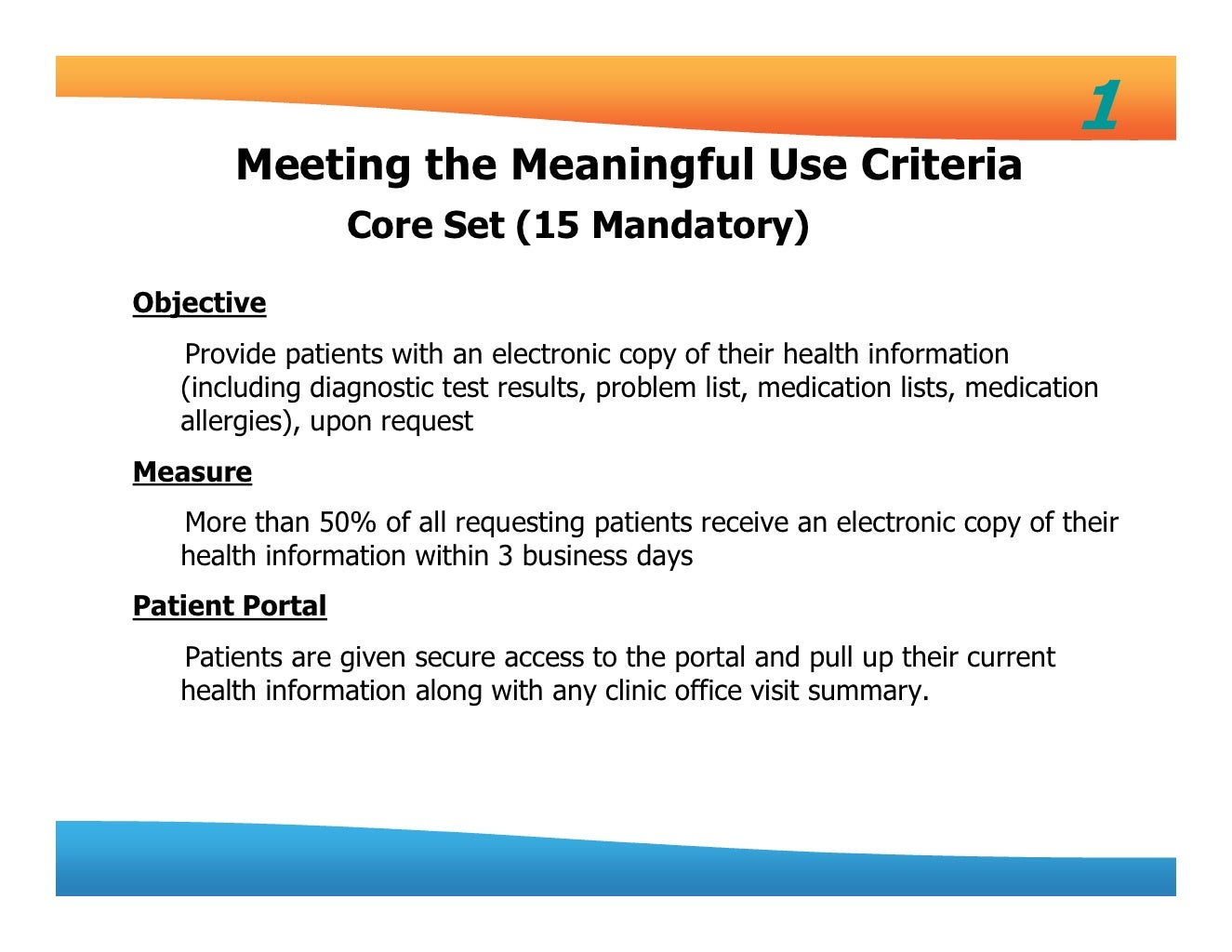
1. The patient (or patient-authorized representative) is provided timely access to view online, download, and transmit his or her health information; and . 2. The provider ensures the patient's health information is available for the patient (or patient-authorized
Can a provider attest to the stage 3 requirements?
Feb 08, 2022 · Patient electronic access: To help encourage patient engagement, meaningful use stage 3 includes an objective in which eligible physicians must provide access to EHRs to more than 80% of patients, with the option to view and download the records. What is required for meaningful use?
What is included in meaningful use Stage 3?
Patient electronic access: To help encourage patient engagement, meaningful use stage 3 includes an objective in which eligible physicians must provide access to EHRs to more than 80% of patients, with the option to view and download the records.
What is the emphasis and/or focus for Stage 3 of the meaningful use criteria?
The Stage 3 proposed rule includes a number of administrative and technical changes, including simpler reporting periods and an increased focus on data quality, EHR interoperability, and healthcare analytics.Mar 20, 2015
Which of the following is a Stage 3 requirement for Medicare and Medicaid EHR incentive program?
To meet Stage 3 requirements, EPs must have 2015 Edition certified EHR technology (CEHRT). However, it did not need to be implemented by January 1, 2020. As long as 2015 Edition functionality is deployed by the first day of the EHR reporting period, the EHR can be pending certification.
When did stage 3 of meaningful use start?
Stage 3 was established in 2017 as a result of the 2015 final rule and focuses on using CEHRT to improve health outcomes. The table on the next page outlines the appropriate stages of the PI Programs based on providers' first year demonstrating meaningful use.
What stage are we currently in meaningful use?
Stage 32016 Stage 3: The current stage of Meaningful Use, this period focuses on improving outcomes for patients, with profound emphasis on quality over quantity.Jul 18, 2017
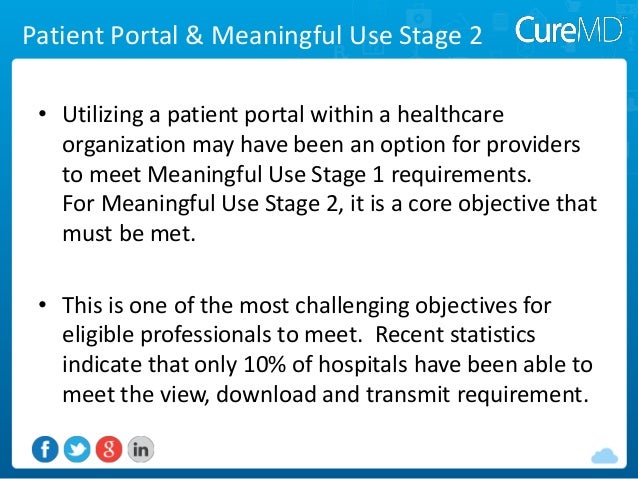
What is meaningful use stage2?
Medicare Meaningful Use Stage 2 Regulations call on care providers to put more advanced processes into place, increase the interoperability of health information and adopt standardized data formats. Stage 2 also places a greater emphasis on exchanging clinical data between providers and enabling patient engagement.
What is the meaningful use program?
'Meaningful Use' is the general term for the Center of Medicare and Medicaid's (CMS's) electronic health record (EHR) incentive programs that provide financial benefits to healthcare providers who use appropriate EHR technologies in meaningful ways; ways that benefit patients and providers alike.
What is required for meaningful use?
There are three basic components of meaningful use: 1) The use of a certified EHR in a meaningful manner. 2) The electronic exchange of health information to improve quality of health care. 3) The use of certified EHR technology to submit clinical quality and other measures.
What is an example of meaningful use?
For example, drug/drug interactions, patient treatment plan management, and the ability of patients to send secure messages are all aspects of meaningful use that may differentiate physicians among patients who are becoming more savvy about what is possible with technology.Jan 1, 2016
How many stages are in meaningful use quizlet?
Meaningful use is measured by specific objectives for using an EHR system that will evolve over three stages with the goal of improving health care, engaging patients, improving coordination, increasing efficiency, and maintaining the privacy of patient health information.
What is the difference between EHR and EMR?
An EMR is best understood as a digital version of a patient's chart. It contains the patient's medical and treatment history from one practice. ... By contrast, an EHR contains the patient's records from multiple doctors and provides a more holistic, long-term view of a patient's health.
What is the new name of the meaningful use program?
Promoting InteroperabilityAs part of the 2019 Physician Fee Schedule Final Rule, the Centers for Medicare & Medicaid Services (CMS) changed the name of the program to the Promoting Interoperability (PI) Program and introduced amendments to program requirements for 2019.Jun 13, 2019
What is EHR incentive?
The Medicare and Medicaid EHR Incentive Programs encourage patient involvement in their health care. Online access to health information allows patients to make informed decisions about their care and share their most recent clinical information with other health care providers and personal caregivers.
What is the eligibility for CAH measure 1?
Eligible Hospital/CAH Measure 1: For more than 80 percent of all unique patients discharged from the eligible hospital or CAH inpatient or emergency department (POS 21 or 23):
When does a patient need to be seen by the EP?
The patient needs to be seen by the EP during the EHR reporting period or be discharged from the hospital inpatient or emergency department during the EHR reporting period in order to be included in the denominator.
Does CEHRT require email?
The specifications for measure 1 allow the provision of access to take many forms and do not require a provider to obtain an email address from the patient. Although many CEHRT products may be designed in that fashion, it is not required by the program. If a provider’s CEHRT does require a patient email address, but the patient does not have or refuses to provide an email address or elects to ‘‘opt out’’ of participation, that is not prohibited by the EHR Incentive Program requirements nor does it allow the provider to exclude that patient from the denominator. The patient may also access their information through their patient authorized representative.
What is the numerator for measure 2?
The numerator for Measure 2 is the number of patients (or patient-authorized representative) in the denominator who were provided electronic access to patient-specific educational resources using clinically relevant information identified from CEHRT during the EHR reporting period.
Can paper based actions be counted in measure 2?
Paper-based actions are no longer allowed or required to be counted for measure 2 calculations. Providers may still provide paper based educational materials for their patients, we are just no longer allowing them to be included in measure calculations.
What is an API?
An API is a set of programming protocols established for multiple purposes. APIs may be enabled by a provider or provider organization to provide the patient with access to their health information through a third-party application with more flexibility than is often found in many current ‘‘patient portals.’’
Patient Engagement
- Patient engagement was a very hot topic at the recent HIMSS conference in Chicago. There was no shortage of exhibitors promoting their patient engagement tools and there were also several presentations that contained suggestions for better engaging patients. Some exhibitors that we spoke to were not aware of the proposed patient engagement rules (described below) and were …
Healthcare Usability and The Joint Commission
- Usability was again a hot topic at HIMSS. Well, actually the lack of usability in healthcare software was again a hot topic at HIMSS. For many years, we have been a strong advocate for promoting Usability in healthcare (see www.HealthcareUsability.com(link is external)) . The Joint Commission provides detailed evidence for the need to create #SafeHealthIT. The most salient …
Onc and Meaningful Use Stage 3
- The Office of the National Coordinator (ONC) released their proposed rules for Meaningful Use Stage 3 just in time to be top on the minds of majority of HIMSS attendees. ONC proposed an increase from five to 25 percent for getting patients to view, download, and transmit personal health data. They propose requiring that more than 35 percent of all patients seen by a provider …
How Should EHR Vendors Create Tools For Patient Engagement?
- The answer, of course, is usability and user-centered design. Patient portals cannot merely output information from the patient chart (that is normally viewed by trained medical staff) in a fancy new view. Patient Portals need to be designed with the patient in mind. In order to achieve the improved engagement, Patient Portals need to present information, and workflow, to the patient…
Design For The Users--Not The Requirements
- Use the persona’s to create realistic use cases based upon the real patient and caregiver needs that you understand based upon your research. Usability people often call these use cases “user journey maps.” Now, when you design your portal to engage the patient around their tasks (and not merely to satisfy regulatory requirements) the end users/patients will find the information pr…
Popular Posts:
- 1. kaerwell patient login
- 2. covermymeds patient portal
- 3. mvmg patient portal
- 4. patient guide report
- 5. pure obgyn patient portal
- 6. womens obgyn patient portal
- 7. patient portal family practice holton ks
- 8. colonial orthopaedics patient portal
- 9. chicagoland complete healthcare patient portal
- 10. healthy results patient portal