A 2020 Vision of Patient-Centered Primary Care - PMC
15 hours ago Commentary on the IOM report. Patient care. Commentary on the IOM report. Patient care J Am Coll Dent. Spring 1995;62(1):23-4. Author J F Hasler 1 Affiliation 1 University of Maryland Dental School, Baltimore, USA. PMID: 7730514 No abstract available ... Patient-Centered Care / organization & administration* >> Go To The Portal
As discussed in the IOM’s Crossing the Quality Chasm Crossing the Quality Chasm: A New Health System for the 21st Century is a report on health care quality in the United States published by the Institute of Medicine on March 1, 2001. A follow-up to the frequently cited 1999 IOM patient safety report To Err Is Human: Building a Safer Health S…Crossing the Quality Chasm
Full Answer
What is patient centered care and how is it better?
- treating you with dignity, respect and compassion
- communicating and coordinating your care between appointments and different services over time, such as when making a referral from your GP to a specialist
- or sharing your care between a community health service and a hospital
- tailoring the care to suit your needs and what you want to achieve
How to provide excellent patient centered care?
- The patient care environment should be peaceful and as stress free as possible. ...
- Patient safety is key. ...
- Patient care should be transparent. ...
- All caregivers should focus on what is best for the patient at all times.
- The patient should be the source of control for their care. ...
What is patient centric care really means?
Patient-centered care is the practice of caring for patients (and their families) in ways that are meaningful and valuable to the individual patient. It includes listening to, informing and...
What are the benefits of patient centered care?
- The health care system’s mission, vision, values, leadership, and quality-improvement drivers are aligned to patient-centered goals.
- Care is collaborative, coordinated, and accessible. ...
- Care focuses on physical comfort as well as emotional well-being.
How does the IOM define patient-centered care?
The IOM (Institute of Medicine) defines patient-centered care as: “Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.”[1]
What are the 5 key elements of patient-centered care?
Research by the Picker Institute has delineated 8 dimensions of patient-centered care, including: 1) respect for the patient's values, preferences, and expressed needs; 2) information and education; 3) access to care; 4) emotional support to relieve fear and anxiety; 5) involvement of family and friends; 6) continuity ...
What might be good indicators of patient-centeredness as recommended by IOM?
The IOM endorsed six patient-centeredness dimensions that stipulated that care must be: respectful to patients' values, preferences, and expressed needs; coordinated and integrated; provide information, communication, and education; ensure physical comfort; provide emotional support; and involve family and friends.
What are the 4 C's of patient-centered care?
The four primary care (PC) core functions (the '4Cs', ie, first contact, comprehensiveness, coordination and continuity) are essential for good quality primary healthcare and their achievement leads to lower costs, less inequality and better population health.
What are the 7 core values of a person-Centred approach?
In health and social care, person-centred values include individuality, rights, privacy, choice, independence, dignity, respect and partnership.
What are the 8 core values of person-centred care?
The eight values in person-centred healthcare are individuality, rights, privacy, choice, independence, dignity, respect, and partnership. All that you need is a healthcare professional who, at the very least, ask three questions: Why are you here?
What are the 6 IOM aims?
Its follow-up report, Crossing the Quality Chasm: A New Health System for the 21st Century (2001), introduced the IOM Six Aims for Improvement: care that is safe, timely, effective, efficient, equitable and patient-centered (STEEEP).
How do you evaluate patient-centered care?
The IOM endorsed six dimensions of patient-centered care which stated that care must be: 1) respectful to patients' values, preferences, and expressed needs; 2) coordinated and integrated; 3) provide information, communication, and education; 4) ensure physical comfort; 5) provide emotional support – relieving fear and ...
How do you evaluate patient Centred care?
The Institute of Medicine (IOM) considers care to be patient centered if it, is “respectful of and responsive to individual patient preferences, needs, and values and ensures that patient values guide all clinical decisions.”1 The IOM further separates patient-centered care into 8 dimensions, including respect for ...
What are examples of patient-centered care?
Patient-centered care examplesLetting the patient choose who can visit them.Allowing the patient to pick their own visiting hours.Inviting the patient's family members to participate in decision-making.Providing accommodations for visitors, like food and blankets.
What are the 4 P's in nursing?
Attention will be focused on the four P's: pain, peripheral IV, potty, and positioning. Rounds will also include an introduction of the nurse or PCT to the patient, as well as an environmental assessment.
What is patient-centered care and why is it important?
Patient-centered care (PCC) has the potential to make care more tailored to the needs of patients with multi-morbidity. PCC can be defined as “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions” [9].
What are the principles of patient centered care?
To clarify, the authors of this paper suggest that the principles of patient-centered care include respect for patients’ values, preferences, and expressed needs; coordination and integration of care; and providing emotional support alongside the alleviation of fear and anxiety associated with clinical care. Similar to the NCQA report, the authors of this paper agree that patient-centered care initiatives are a parallel and possibly underlying dimension of health literacy, language access, and cultural competence efforts in that patient-centered health initiatives are associated with beneficial health outcomes, including improved patient experience, safety, and clinical effectiveness.
What is integrated measure of health literacy?
An integrated measure of health literacy, language access, and cultural competence would enable a hospital or health system to establish baselines and evaluate progress as part of the American Hospital Association’s (AHA) renewed efforts to improve care to diverse patients and improve health equity. AHA’s commitment to revitalizing its prior equity and diverse care initiatives was underscored in a change in the name of the association’s efforts in 2018. AHA said that its renamed Institute for Diversity and Health Equity “more accurately depict [s] our mission now that we have realigned ourselves as a core membership resource within the AHA” [26].
What is the importance of cultural competence in health care?
An integrated measure of health literacy, language access, and cultural competence could reduce health disparities, could highlight patient engagement, would contribute to improvement in patient care practices, and would not duplicate existing improvement activities.
What are the three domains of quality performance measures?
The development of integrated quality performance measures for three domains—health literacy, language access, and cultural competence —was proposed at a 2015 workshop of the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine [9].
What is NCQA?
NCQA concluded that implementing more health literacy, language access, and cultural competence initiatives within the health care delivery system could contribute to improved health care in the United States—and that ensuring quality improvements might occur if these activities were assessed systematically.
What is the risk of BRCA 1 and 2?
Women with BRCA 1and 2gene mutations are at higher risk for developing breast and ovarian cancer , and may face difficult decisions about breast cancer screening, as well as consideration of prophylactic mastectomy or oophorectomy to reduce the risk of cancer3(Jolie, 2013; Schwartz et al., 2009).
What is the cause of communication problems in cancer patients?
A lack of understandable and easily available information on prognosis, treatment options, likelihood of treatment responses, palliative care, psychosocial support, and the costs of cancer care contribute to communication problems, which are exacerbated in patients with advanced cancer.1.
How does cancer affect emotional health?
The emotional repercussions of a cancer diagnosis can prevent patients from engaging in effective communication with their clinicians about their diagnosis and treatment. Patients can become anxious; feel vulnerable, alone, and fearful; and experience feelings of losing control when receiving a cancer diagnosis.
What are the most important reports for setting the context of the work of informatics?
Some of the most important reports for setting the context of the work of informatics have been those from the Institute of Medicine (IOM). These reports have now spanned over 20 years, with many serving to raise awareness of problems and provide a context for informatics solutions. Some of the IOM’s seminal reports have covered the topics of electronic health records [1, 2], telemedicine [3], computer networks and the Internet [4], privacy and security [5], medical errors and patient safety [6, 7], healthcare quality [8], health professions education [9], reducing costs while improving outcomes [10], and safety of health information technology [11].
How does informatics help the healthcare system?
Informatics is of course central to the notion of the learning healthcare system by capturing, analyzing, and acting on data from the entire spectrum of care . There is another figure in the report that provides a “schematic” of the healthcare system that allows all of the critical informatics challenges and opportunities to be enumerated. This figure shows that the overall patient care experience begins from science, moving to evidence of what from the science improves patient care, followed by the delivery of that best care that will ideally result in the optimal patient outcomes and satisfaction. When any of these elements is carried out suboptimally, there are missed opportunities, waste, and harm. The only additions I would make to this figure would be feedback loops among the elements, i.e., the patient experience informs new science, evidence, and care, while the care experience feeds back to science and evidence, and so forth.
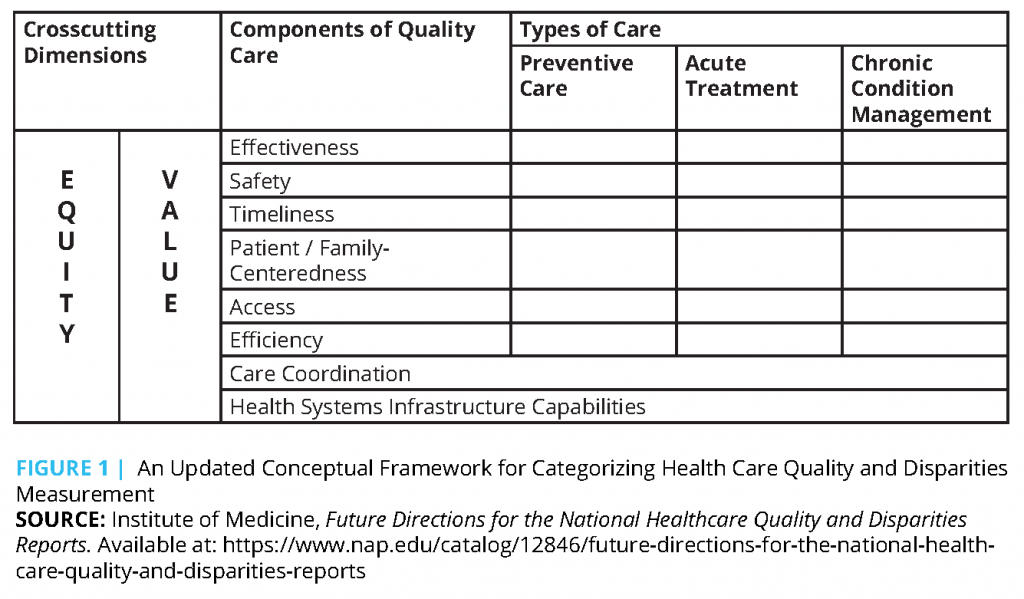
Why are IOM domains important?
Frameworks like the IOM domains also make it easier for consumers to grasp the meaning and relevance of quality measures. Studies have shown that providing consumers with a framework for understanding quality helps them value a broader range of quality indicators. For example, when consumers are given a brief, understandable explanation of safe, ...
What are the six aims of the health care system?
[1] Safe: Avoiding harm to patients from the care that is intended to help them. Effective: Providing services based on scientific knowledge to all who could benefit ...

Introduction
Background
- The provision of high-quality care has long been a goal of the medical care system. Yet a 2000 report from the Institute of Medicine (IOM), To Err Is Human, documented that as many as 98,000 Americans die each year as a result of medical errors, and many more thousands experience nonfatal injuries . In Crossing the Quality Chasm: A New Health Syste...
Description of Commissioned Paper
- The development of integrated quality performance measures for three domains—health literacy, language access, and cultural competence—was proposed at a 2015 workshop of the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine . The Roundtable commissioned the National Committee for Quality Assurance (NCQA) to prepare a p…
Conclusion
- The authors of this paper suggest that the adoption of an integrated measure of health literacy, language access, and cultural competence would enable hospitals and health systems, as well as health consumer leadership organizations, to address specific as well as broader patient-centered framework issues in health equity. Health care organizations could adopt pledges to act, as well …
Join The Conversation!
- Tweet this! “Reducing disparities requires attention to the essential components of equitable, patient-centered, high-quality care – that is, to culturally and linguistically appropriate care as well as attention to health literacy.” https://doi.org/10.31478/201902a#NAMPerspectives Tweet this! In order to ensure our health care system is moving toward providing equitable, patient-centered c…
References
- French, J. B., S H. Scholle, J. Ng, and M. Taylor. 2017.Measuring improvement in the patient-consumer experience of health care: Aligning and leveraging measures of health literacy, language access...
- Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728
- French, J. B., S H. Scholle, J. Ng, and M. Taylor. 2017.Measuring improvement in the patient-consumer experience of health care: Aligning and leveraging measures of health literacy, language access...
- Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/12875