IOM report: patient safety--achieving a new standard for …
2 hours ago IOM report: patient safety--achieving a new standard for care. IOM report: patient safety--achieving a new standard for care. IOM report: patient safety--achieving a new standard for care Acad Emerg Med. 2005 Oct;12(10):1011-2. doi: 10.1197/j.aem.2005.07.010. Author Institute of … >> Go To The Portal
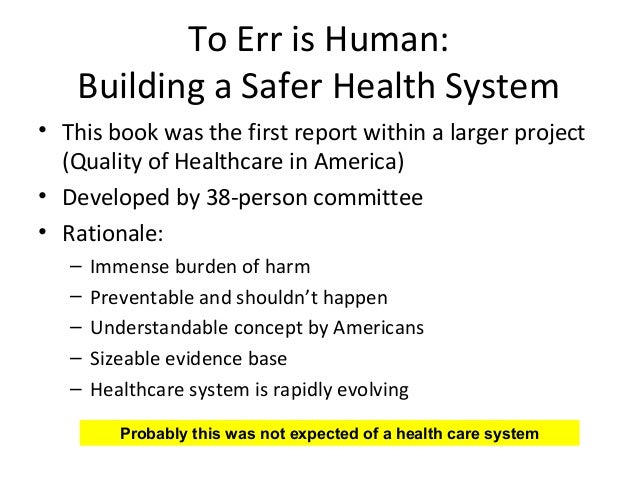
The Institute of Medicine (IOM) released a report in 1999 entitled “ To Err is Human: Building a Safer Health System ”. 1 The report stated that errors cause between 44 000 and 98 000 deaths every year in American hospitals, and over one million injuries. 1 Health care appeared to be far behind other high risk industries in ensuring basic safety.
Full Answer
What is the IOM report?
The IOM in a report revealed that more than one million Afghan citizens have been deported or forced to return to Afghanistan in 2021, with more than thousands fleeing the country in quest of a better quality of life. IOM Afghanistan has also created a ...
How to improve patient safety?
- Advancing Patient Safety
- AHRQ-Funded Patient Safety Research Featured in Health Affairs
- Health Care Safety Hotline
- National Academy of Medicine Reports
- National Action Plans
- Papers on Diagnostic Safety Topics
- PSNet
How do you improve patient safety in hospitals?
PHILADELPHIA, Dec. 9, 2021 /PRNewswire/ -- ObservSMART, a patient safety compliance system, announced today that Day Kimball Hospital in Putnam, Connecticut, has begun using its technology to ...
What are the major patient safety issues in hospitals?
- providing global leadership and fostering collaboration between Member States and relevant stakeholders
- setting global priorities for action
- developing guidelines and tools
- providing technical support and building capacity of Member States
- engaging patients and families for safer health care
- monitoring improvements in patient safety
What is the 2000 IOM report?
Tracking The Changing Safety Net The 2000 IOM report found that the federal government lacked any comprehensive, coordinated ability to track and monitor the changing status of America's health care safety net and its success in meeting the needs of our most vulnerable populations.
What did the IOM errors report show?
The Institute of Medicine (IOM) released a report in 1999 entitled “To Err is Human: Building a Safer Health System”. The report stated that errors cause between 44 000 and 98 000 deaths every year in American hospitals, and over one million injuries.
What does IOM mean in healthcare?
the Institute of MedicineOne of the most influential is the framework put forth by the Institute of Medicine (IOM), which includes the following six aims for the health care system. Safe: Avoiding harm to patients from the care that is intended to help them.
What is the IOM report To Err is Human?
On November 29, 1999, the Institute of Medicine (IOM) released a report called To Err is Human: Building a Safer Health System. The IOM released the report before the intended date because it had been leaked, and one of the major news networks was planning to run a story on the evening news.
What did the IOM report To Err is Human find as contributors to medical errors?
The Institute of Medicine (IOM) released their landmark report, To Err Is Human, in 1999 and reported that as many as 98,000 people die in hospitals every year as a result of preventable medical errors.
Which was the purpose of the Institute of Medicine IOM report on preventing medication errors?
The report was commissioned by the Centers for Medicare and Medicaid Services at the direction of Congress and released on 20 July. It found that drug related errors are the most common medical errors and can occur at every stage from prescription through to monitoring the patient's response.
What is the IOM report on nursing?
Released in October 2010, the Institute of Medicine (IOM) report, The Future of Nursing: Leading Change, Advancing Health, is a thorough examination of the nursing workforce.
What are the IOM standards?
IOM Standards for Systematic ReviewsManage bias and conflict of interest (COI) of the team conducting the systematic review; and.Manage bias and COI for individuals providing input into the systematic review.
What is the role of IOM in nursing?
IOM and HMD The National Academies are private, nonprofit institutions that provide independent, objective analysis and advice to the nation and conduct other activities to solve complex problems and inform public policy decisions related to science, technology, and medicine.
What has been the historical importance of the Institute of Medicine IOM reports since 1999?
What has been the historical importance of the Institute of Medicine (IOM) reports since 1999? 1. They stimulated the development of strategies that will improve quality of care.
What does err is human mean?
Definition of to err is human formal. : it is normal for people to make mistakes.
Which quality issues were found in the Institute of Medicine IOM study To Err is Human: Building a Safer Health System?
Which quality issues were found in the Institute of Medicine (IOM) study, To Err is Human: Building a Safer Health System? Many errors are preventable. Data from the IOM study concluded that up to 98,000 patients die each year from preventable medical errors.
What does the term medical error mean to you?
Medical error: the failure of a planned action to be completed as intended (an error of execution) or the use of a wrong plan to achieve an aim (an error of planning) (Reason, 1990). 35. An unintended act (either of omission or commission) or one that does not achieve its intended outcome (Leape, 1994).
What is medical error in healthcare?
A medical error is defined as the "failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim (1)." Most medical errors do not result in medical injury, although some do, and these are termed preventable adverse events.
How often do medical errors occur?
One in 5 Americans has experienced a medical error while receiving health care (Institute for Healthcare Improvement/NORC at the University of Chicago, 2017). Almost 1 in 5 medication doses given during hospital stays are given in error (DataRay, 2002).
Where is the Institute of Medicine?
Institute of Medicine, Home Secretary, 2101 Constitution Avenue, Washington, DC 20418, USA.
When was the IOM report released?
Setting a Direction. In early 2000, just 60 days after the IOM report was published, the Federal Government, through an AHRQ-led task force, released Doing What Counts for Patient Safety: Federal Actions to Reduce Medical Errors and Their Impact.
What is the Patient Safety and Quality Handbook?
Given the central role that nurses serve in patient care and the likelihood that they are among the first health care professionals to recognize errors and prevent harm to patients, the Agency teamed with the Robert Wood Johnson Foundation to develop and distribute a handbook for nurses entitled Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Even though working conditions may be less than optimal and the needs of patients are quite diverse, the opportunities for patient safety and quality improvement are clearly addressed. More than 22,000 copies of the three-volume handbook have been distributed to nursing schools and clinicians in the field.
What is AHRQ Advances in Patient Safety?
AHRQ released Advances in Patient Safety: From Research to Implementation as a way to share the progress occurring in the first half of the decade. The four-volume publication, comprising 140 articles, sought to bridge the gap between the research underway and its integration into practice. The compendium covered a wide range of research paradigms, clinical settings, patient populations, reporting systems, measurement and taxonomy issues, tools and technology, implementation challenges, safety culture, and organizational considerations. The volumes helped fuel efforts to improve patient safety and provided a measure of progress. More importantly, they also provided a sense of remaining challenges.
What is AHRQ WebM&M?
AHRQ WebM&M serves as a free, online journal and forum for the examination of a variety of patient safety and quality issues. It features analysis of medical error cases by recognized experts and provides interactive learning modules for health care professionals, clinicians, administrators, patient safety officers, and trainees. Since its launch, AHRQ WebM&M has grown in popularity and continues to be one of AHRQ's most frequently visited Web sites.
What is a PSIC?
In response to the need to expand the patient safety knowledge and skills of midlevel professionals responsible for investigating medical errors and initiating improvements, AHRQ partnered with the Department of Veterans Affairs' National Center for Patient Safety and began the first of four 9-mont h Patient Safety Improvement Corps (PSIC) training programs. Participants received training on tools and topics including analyzing root causes, analyzing health care failure modes and effects, applying human factors principles, assessing patient safety culture, and making a business case for patient safety. By the program's end, teams had been trained in every State, as well as the District of Columbia and Puerto Rico. Feedback the Agency received that PSIC graduates were, in turn, training their own personnel in patient safety principles acquired from the program provided evidence that this program represented a significant step in disseminating patient safety knowledge throughout the country.
What is the most common complication of hospital care?
Data indicate that health care-associated infections (HAIs) are the most common serious complication of hospital care, striking nearly 2 million U.S. hospital patients, resulting in an estimated 99,000 deaths, and costing the health care system up to $20 billion each year, according to the Centers for Disease Control and Prevention (CDC). The most common HAI is methicillin-resistant Staphylococcus aureus (MRSA). With some MRSA-related projects already underway, Congress directed AHRQ to work with its Federal partners at the CDC and the Centers for Medicare & Medicaid Services to develop an action plan to identify and help reduce the spread of MRSA and related HAIs. The action plan is designed to:
How does the Health Information Technology Agency help?
To provide technical assistance and share knowledge and findings , the Agency established a National Resource Center for Health IT. All of the lessons learned from these projects are helping health care providers move closer to a fully operational health IT system in support of improved quality, safety, and continuity of care.
What is health IT?
Health IT, when well designed and implemented, is a tool that can help health information flow in ways that allow for improvements in patient health and safety. Whatever the drawbacks to health IT systems, the evidence suggests that health IT has raised the floor on safety.
Does health IT improve patient safety?
Since then, whether health IT actually improves patient safety has remained an open question. The nation has seen widespread adoption of health IT as a result of the Medicare and Medicaid EHR Incentive Programs. With that increase in adoption, there should be more and better evidence on the actual impact of health IT on safety.
When was the report "To Err is Human" published?
Background: The “ To Err is Human ” report published by the Institute of Medicine (IOM) in 1999 called for a national effort to make health care safer. Although the report has been widely credited with spawning efforts to study and improve safety in health care, there has been limited objective assessment of its impact. We evaluated the effects of the IOM report on patient safety publications and research awards.
What is the conclusion of the report "To Err is Human"?
Conclusions: Publication of the report “ To Err is Human ” was associated with an increased number of patient safety publications and research awards. The report appears to have stimulated research and discussion about patient safety issues, but whether this will translate into safer patient care remains unknown.
Is there a need for continued patient safety research support?
Rather, there is a need for continued patient safety research support and increased healthcare quality research support which has recently stalled . Otherwise, there is a risk that patient safety will be dropped as a priority due to a perceived lack of progress, and the impact of “ To Err is Human ” will be short lived.
What does Illingsworth say about patient safety?
Illingsworth states that although there have been many changes tested and implemented to improve safety, many systems are not designed with patient safety in mind. “It is only the skill and resilience of health care professionals,” he asserts, “that prevents many more episodes of harm.”. However, he also argues, ...
What is the first part of the IHI report?
The first part of the report focuses on the case for change. “As with other safety-critical industries,” Illingworth contends, “it is imperative that when failures do occur, lessons are learned and action is taken to prevent the same issues reoccurring .” This notion of a continuous learning system is key element of IHI’s Framework for Safety.
What are the recommendations of the NPSF?
The NPSF report includes eight recommendations (see infographic, right): Ensure that leaders establish and sustain a safety culture. Create a centralized and coordinated approach to patient safety. Create a common set of safety metrics that reflect meaningful outcomes.
What is the NPSF report?
The National Patient Safety Foundation (NPSF) Report: Not Enough Change Since To Err Is Human#N#A committee co-chaired by Dr. Don Berwick and Dr. Kavek Shajania issued the NPSF’s Free from Harm: Accelerating Patient Safety Improvement Fifteen Years after To Err Is Human. Similar to the Health Foundation’s assessment of patient safety in the UK, the NPSF report states that — despite some improvement in patient safety in the United States — the pace and scale of improvement has been disappointingly slow and limited. Patients continue to experience harm when interacting with the health care system and, consequently, much more needs to be done. Like the Health Foundation, NPSF also notes that the problem of making health care safer is far more complex than initially understood.#N#The NPSF report includes eight recommendations (see infographic, right): 1 Ensure that leaders establish and sustain a safety culture. 2 Create a centralized and coordinated approach to patient safety. 3 Create a common set of safety metrics that reflect meaningful outcomes. 4 Prioritize funding for research in patient safety and implementation science. 5 Address safety across the entire care continuum. 6 Support the health care workforce. 7 Partner with patients and families for the safest care. 8 Ensure that technology is safe and optimized to improve patient safety.
Why are IOM domains important?
Frameworks like the IOM domains also make it easier for consumers to grasp the meaning and relevance of quality measures. Studies have shown that providing consumers with a framework for understanding quality helps them value a broader range of quality indicators. For example, when consumers are given a brief, understandable explanation of safe, ...
What are the six aims of the health care system?
[1] Safe: Avoiding harm to patients from the care that is intended to help them. Effective: Providing services based on scientific knowledge to all who could benefit ...
Introduction
- Patient safety was a fairly new field when the Institute of Medicine's (IOM) sentinel report, To Err is Human: Building a Safer Health System, captured the Nation's attention in late 1999. While the IOM made recommendations to Congress for investigating medical errors and improving patient safety, the reality was that extensive foundation building ...
Develop A Solid Evidence Base
- To build a robust patient safety infrastructure, the Agency began its work to gain a better understanding of the systemic factors that combine in unanticipated ways and threaten patient safety. Researchers studied the best ways to identify and report on these factors and examined the impact that working conditions, health care information technology, and enhanced provider …
Design and Evaluate Useful Strategies and Tools
- AHRQ's initial grants helped build a patient safety knowledge base and informed the Agency's thinking about the next steps it needed to take. As the knowledge base continued to evolve, it became clear that AHRQ needed to produce sound research studies and to ensure that the information, educational content, new approaches, and tools it provided were relevant to provide…
Disseminate Information and Tools For Implementation
- As the decade progressed and the knowledge base continued to expand, reports of successful application of evidence-based strategies began to increase. For example, by consistently following evidence-based procedures, some health care systems were achieving significant reductions in health care-associated infections. Unfortunately, these examples were the excepti…
Advancing Patient Safety: A Decade of Evidence, Design, and Implementation
- Patient safety was a fairly new field when the Institute of Medicine's sentinel report, To Err is Human: Building a Safer Health System, captured the Nation's attention in late 1999. While the Institute of Medicine made recommendations to Congress for investigating medical errors and improving patient safety, the reality was that extensive foundation building needed to occur befo…
Popular Posts:
- 1. an adult cystic fibrosis patient presenting with persistent dyspnea: case report
- 2. patient portal of flemingsburg ky
- 3. patient portal radiology limited
- 4. patient scheduling software demo login
- 5. for workmens comp what is a patient ie report
- 6. next gen patient portal log in
- 7. yomaris pena patient portal
- 8. ohsu oregon patient portal
- 9. mdoffice patient portal login
- 10. patient portal mount carmel medical group