How to Write a Good Medical History: 6 Steps (with …
26 hours ago Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion. The abstract of a patient case report should succinctly include the four … >> Go To The Portal
How to Write a Good Patient Medical Report.
- Step 1: Create an introduction about the background. Have an abstract about the patient medical report. Make an introduction about it. Data like the ...
- Step 2: Write the medical history of the patient. Before you will deliver your observations for the patient, you must first tackle about his medical ...
- Step 3: Report the specimens. Whatever test and examination that you have given to the patient, have the result documented. These will be the ...
- Step 4: Be clear about the diagnosis. The main point of the patient medical report is the diagnosis that you have for the patient. Whatever disease ...
- Step 1: Include the important details of your current problem. Timing - When did your problem start? ...
- Step 2: Share your past medical history. ...
- Step 3: Include your social history. ...
- Step 4: Write out your questions and expectations.
How do you write a patient history step by step?
Steps Take down the patient's name, age, height, weight and chief complaint or complaints. Gather the primary history. Ask the patient to expand on the chief complaint or complaints. Expand with the secondary history. This is where you ask about any symptoms the patient is experiencing that are related to the chief complaint.
How do you write a hospital report for a patient?
The more details you can include the better. Include information about how the patient responded to any treatments you performed and then write about putting the patient in your rig and transporting her to the hospital. Conclude with the time you turned her over to the emergency room and what condition she was in at the time.
Why is it important to take patient history?
Taking a history from a patient is a skill necessary for examinations and afterwards as a practicing doctor, no matter which area you specialise in. It tests both your communication skills as well as your knowledge about what to ask.
What is the history component of a patient presentation?
The history component is comparable to telling a story and should include a beginning and some form of development to adequately describe the patient’s presenting problem.
What is the level of detail in a medical history?
What to ask a patient about a complaint?
What is secondary history?
How many times has wikihow been viewed?
What to include in a review of symptoms?
How many references are there in wikihow?
What is included in family status?
See more
About this website
How do you write patient history?
Procedure StepsIntroduce yourself, identify your patient and gain consent to speak with them. ... Step 02 - Presenting Complaint (PC) ... Step 03 - History of Presenting Complaint (HPC) ... Step 04 - Past Medical History (PMH) ... Step 05 - Drug History (DH) ... Step 06 - Family History (FH) ... Step 07 - Social History (SH)More items...
What should be included in a patient's history?
At a minimum it should include the following, but be prepared to take down any information the patient gives you that might be relevant:Allergies and drug reactions.Current medications, including over-the-counter drugs.Current and past medical or psychiatric illnesses or conditions.Past hospitalizations.More items...
How do you write a report about a patient?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
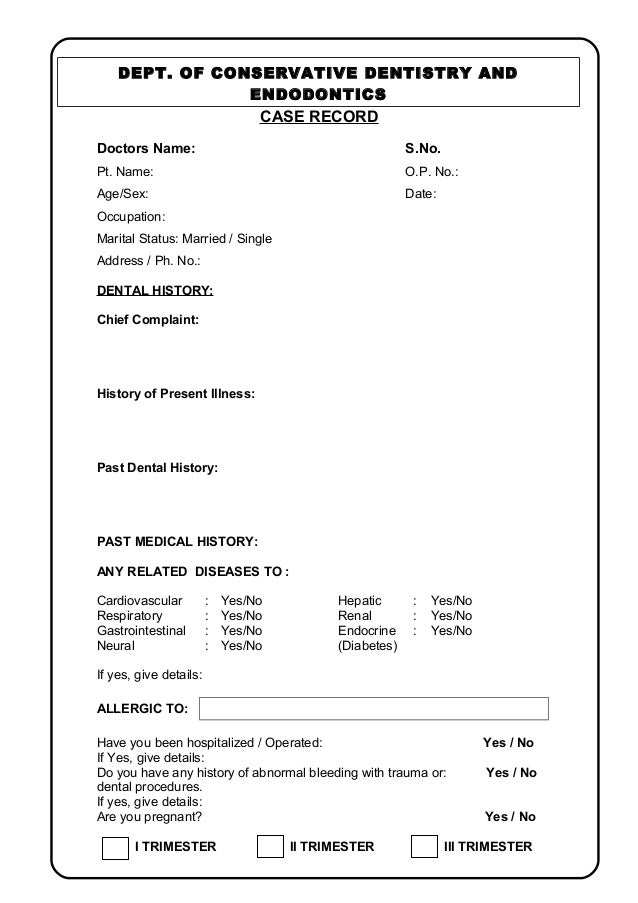
What should I write in my past medical history?
Past illnesses: e.g. cancer, heart disease, hypertension, diabetes. Hospitalizations: including all medical, surgical, and psychiatric hospitalizations. Note the date, reason, duration for the hospitalization. Injuries, or accidents: note the type and date of injury.
What are the 7 components of health history?
Components of a Comprehensive Health HistoryHistory of Presenting Illness.Past Medical History.Glycemic Control.Nutritional Status.Allergies.Medications.Family History.Psychological Well Being.
How do you present a medical history?
You should begin every oral presentation with a brief one-liner that contains the patient's name, age, relevant past medical history, and chief complaint. Remember that the chief complaint is why the patient sought medical care in his or her own words. An example of an effective opening is as follows: “Ms.
How do you start a report?
The first section you start writing in your report is always a summary or introduction. This should stretch across just one or two pages to give your reader a brief glimpse into what your results or findings are.
What is the format for report writing?
Report writing is a formal style of writing elaborately on a topic. The tone of a report and report writing format is always formal. The important section to focus on is the target audience. For example – report writing about a school event, report writing about a business case, etc.
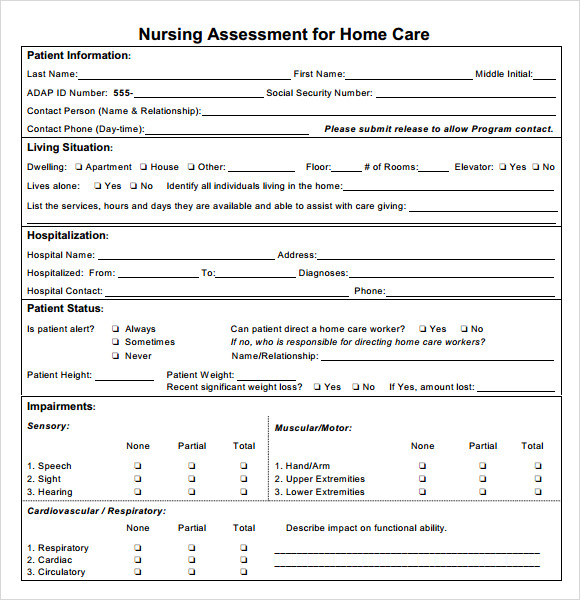
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do you take good patient history?
Greet the patient by name and introduce yourself. Ask, “What brings you in today?” and get information about the presenting complaint. Collect past medical and surgical history, including any allergies and any medications they're currently taking. Ask the patient about their family history.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
Sample of Nursing Health History - 1049 Words | Studymode
Nursing Health History Nursing health history is the first part and one of the mostsignificant aspects in case studies. It is a systematic collection ofsubjective and objective data, ordering and a step-by-step processinculcating detailed information in determining client’s history, healthstatus, functional status and coping pattern.
Example of a Complete History and Physical Write-up
Example of a Complete History and Physical Write-up Patient Name: Unit No: Location: Informant: patient, who is reliable, and old CPMC chart. Chief Complaint: This is the 3rd CPMC admission for this 83 year old woman with a long history of hypertension who presented with the chief complaint of substernal “toothache like” chest pain of 12 hours
What is patient case report?
Patient case reports are valuable resources of new and unusual information that may lead to vital research.
What should be included in the abstract of a patient case report?
The abstract of a patient case report should succinctly include the four sections of the main text of the report. The introduction section should provide the subject, purpose, and merit of the case report.
Why should you ask a patient about his medical history?
Ask the patient about his medical history. You should put it to have a better analyzation of the medical condition of the patient. It can also make the doctors to be careful with the medication that they can give to the patient. Whatever is the sickness that a patient has before he is admitted to the hospital should be written in the patient medical report.
Who makes the patient medical report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physicians, nurses, and doctors of medicine. It also includes the psychiatrists, pharmacists, midwives and other employees in the allied health. It is part of their job to make a patient medical report because the health condition of all the patients should be documented. Hospitals keep history of medical records. The functions of medical records are more than important, so they continually keep track on the patient’s health conditions.
Why should a patient's medical report include lab results?
It is also needed because sometimes the laboratory and the test results are the proof of the sickness of the patient. For example, if the patient has a blood cancer, it can be seen with the blood tests. If the patient has a brain tumor, it can be seen through a brain CT scan. A CT scan for the body can also tell whether we have a fracture or not.
Why should medication be documented in a medical report?
The treatments or medications should also be documented because it can provide a good information about the medical history of a patient. Put the names of the medicines and tell how often did the patient takes it. You can also document its effect and tell whether it is effective for them.
What is a recommendation statement?
These are statements about the recommendations of the doctor. They are statements whether a patient can do a particular thing or not. It tell limitations on thing that they should not do for a while and it tell the abilities that they, of course, have. This is necessary so that the sickness will not get worse.
Is a medical report a legal document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patient is under your care. Thus, it can be used in court as an essential proof. So, keep a patient medical report because you may need it in the future.
Is a doctor a doctor?
A doctor is a doctor. They are not writers. They can be caught in a difficulty on how to write a patient medical report. If this is the case, turn to this article and use these steps in making a patient medical report.
How many levels of history are there in Medicare?
The Centers for Medicare and Medicaid Services (CMS) Documentation Guidelines for Evaluation and Management Services have four history levels, each of which comprises four elements. 1 To qualify for a given history level, certain elements are required, as depicted in Table 1.
Who must obtain HPI?
HPI includes information obtained from the patient and must be obtained by the provider or a qualified healthcare professional. Some Medicare carriers have established their own policies that require the provider to perform the work of the HPI.
What is the difference between a detailed and a problem focused history?
For example, a problem-focused history requires documentation of the chief complaint (CC) and a brief history of present illness (HPI), while a detailed history requires the documentation of a CC, an extended HPI, plus an extended review of systems (ROS) and pertinent past, family and/or social history (PFSH).
What happens if a clear CC is not documented?
If a clear CC is not documented, the provider may be subject to a denial in the event of an audit and is usually referenced as not being medically necessity. History of Present Illness: The HPI is a chronological description of the patient’s symptoms or clinical problems from the onset and/or how it has developed.
What is a PCR report?
A patient care report, more commonly known as a PCR, is a summary of what went on during an emergency call. EMS and other first-responders use the PCR to fill in the details of every call -- even the ones that get canceled or deemed false alarms Every department has its own procedures for filing a PCR and many companies now use EPCRs, ...
Why is PCR important?
Every piece of information in a PCR is vital because it may have to be used in court.
Why do you take a history?
Taking a history from a patient is a skill necessary for examinations and afterwards as a practicing doctor, no matter which area you specialise in. It tests both your communication skills as well as your knowledge about what to ask. Specific questions vary depending on what type of history you are taking but if you follow the general framework below you should gain good marks in these stations. This is also a good way to present your history.
Who do you need to collect collateral history?
In practice you may sometimes need to gather a collateral history from a relative, friend or carer. This may be with a child or an adult with impaired mental state.
Is it a good idea to find out if a patient has allergies?
At this point it is a good idea to find out if the patient has any allergies.
Can you ask a patient about their history?
During or after taking their history, the patient may have questions that they want to ask you. It is very important that you don’t give them any false information. As such, unless you are absolutely sure of the answer it is best to say that you will ask your seniors about this or that you will go away and get them more information (e.g. leaflets) about what they are asking. These questions aren’t necessarily there to test your knowledge, just that you won’t try and 'blag it'.
What is the level of detail in a medical history?
The level of detail the history contains depends on the patient's chief complaint and whether time is a factor. When there is time for a complete history, it can include primary, secondary and tertiary histories of the chief complaint, a review of the patient's symptoms, and a past medical history.
What to ask a patient about a complaint?
Ask the patient to expand on the chief complaint or complaints . In particular, ask about anything that the patient was unclear about or that you don't understand.
What is secondary history?
Expand with the secondary history. This is where you ask about any symptoms the patient is experiencing that are related to the chief complaint. Associated symptoms are often the key to making a correct diagnosis.
How many times has wikihow been viewed?
To create this article, 9 people, some anonymous, worked to edit and improve it over time. This article has been viewed 58,582 times.
What to include in a review of symptoms?
Include a review of symptoms. This is simply a list, by area of the body, of anything that the patient feels might not be normal. It's best to have the list of body areas in mind as you question the patient so you don't forget to ask about each one. Question the patient about these areas:
How many references are there in wikihow?
To create this article, 9 people, some anonymous, worked to edit and improve it over time. There are 7 references cited in this article, which can be found at the bottom of the page.
What is included in family status?
Family status, including whether the patient is married, who the patient lives with and other relationships. Include questions about the patient's current sexual activity and history. Occupation, particularly if it includes exposure to hazardous materials.