How To Fill Out An Emt Patient Care Report Examples?
9 hours ago · How To Fill Out An Emt Patient Care Report Examples? Consult a dictionary before use of language that is vague. use phrases that are vague, like “weakness,” “fall,” or “transport”. A clear clinical picture is elusive from using these terms, so use as general a description or as specific as possible. Table of contents. >> Go To The Portal
Write down the chief complaint of the caller based on what she tells you. Feel free to use shorthand if it’s part of your group’s standard operating procedures, or SOPs. For example, you might write “arrived on scene to find 22 yo female lying on the floor and 23 yo male standing over her.
Full Answer
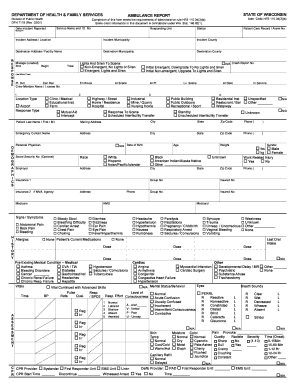
What is an EMS report form?
The EMS Report Form is a medical record of care provided. It is the only written document which can reflect the condition and justify treatment/transport of the prehospital patient at the time of accident or illness. A re-creation of prehospital events should be easily accomplished with a complete and accurately documented EMS Report Form.
How do you write a hospital report for a patient?
The more details you can include the better. Include information about how the patient responded to any treatments you performed and then write about putting the patient in your rig and transporting her to the hospital. Conclude with the time you turned her over to the emergency room and what condition she was in at the time.
Can an EMS provider select “yes” or “no” in a clinical narrative?
However, simply clicking a box or making a selection from a drop-down menu cannot be a substitute for your words in the form of a clear, concise, accurate and descriptive clinical narrative. An EMS provider can select “yes” to the checkbox that the patient experienced chest pain, however that is not enough information.
What does a patient care report consist of?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care. What should not be written in a patient care report?

How do I write a patient care report in EMS?
EMS providers just need to pull the information together and write it down in a way that paints a picture....Follow these 7 Elements to Paint a Complete PCR PictureDispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What should a patient care report include?
What Patient Care Reports Should IncludePresenting medical condition and narrative.Past medical history.Current medications.Clinical signs and mechanism of injury.Presumptive diagnosis and treatments administered.Patient demographics.Dates and time stamps.Signatures of EMS personnel and patient.More items...•
How do you write an ePCR?
How to Write an Effective ePCR NarrativeBe concise but detailed. Be descriptive in explaining exactly what happened and include the decision-making process that led to the action. ... Present the facts in clear, objective language. ... Eliminate incorrect grammar and other avoidable mistakes. ... Be consistent and thorough.
How do you write a patient narrative EMT?
1:2411:38How to Write a Narrative in EMS || DCHART Made Easy ... - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo while in route dispatch advises that the patient can be found outside the residence. Then i talkMoreSo while in route dispatch advises that the patient can be found outside the residence. Then i talk about what i see whenever i get onto the scene upon arrival ems is directed toward the curb.
How do you take care of a patient report?
Document the patient's history completely. Remember bystanders or those close to the patient can often provide valuable information about the patient....Check descriptions. ... Check (and recheck) spelling and grammar. ... Assess your chief complaint description. ... Review your impressions. ... Check the final details.
What does soap mean in EMS?
Subjective, Objective, Assessment and PlanIntroduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
How do I write a paramedic report?
0:4340:58Principles of Medical Documentation and Report Writing - YouTubeYouTubeStart of suggested clipEnd of suggested clipMedical history assessment findings. Medical device data treatments provided medications deliveredMoreMedical history assessment findings. Medical device data treatments provided medications delivered procedures performed and the patient's final disposition. Upon delivery at the hospital.
When you document information on a patient that you treat and care for this written report is called the?
When you document information on a patient that you treat and care for. This written report is called the: Patient care report, run report. You are asked to give testimony in court about the care you gave to a patient.
What is the narrative section of the patient care report?
Detailed explanation of medical necessity: Your narrative should be detailed and provide a clear explanation for why the patient needed to be transported by ambulance. Include what the medical reasons were that prevented the patient from being transported by any other means.
How do you write a narrative document?
10 TIPS FOR WRITING EFFECTIVE NARRATIVE NURSE'S NOTESBe Concise. ... Note Actions Once They are Completed. ... When Using Abbreviations, Follow Policy. ... Follow SOAIP Format. ... Never Leave White Space. ... Limit Use of Narrative Nurse's Notes to Avoid Discrepancies. ... Document Immediately. ... Add New Information When Necessary.More items...•
What is a component of the narrative section of a patient care report?
The narrative section of the PCR needs to include the following information: Time of events. Assessment findings. emergency medical care provided. changes in the patient after treatment.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
How to determine if a medical necessity is met?
A primary way to determine if medical necessity requirements are met is with documentation that specifically states why you took the actions you did on a call. For example, simply documenting “per protocol” as the reason why an IV was started or the patient was placed on a cardiac monitor is not enough.
What should a PCR tell?
The PCR should tell a story; the reader should be able to imagine themselves on the scene of the call.
Why do you write PCR when you call?
Writing the PCR as soon as the call is over helps because the call is still fresh in your mind . This will help you to better describe the scene and the condition the patient was in during your call.
Why is an IV established on the patient?
This specifically explains why an IV was established on the patient and states facts that can be used to show medical necessity for the call. The same can be said for non-emergency transports between two hospitals. Simply documenting that the patient was transported for a “higher level of care” is not good enough.
When should PCR be completed?
While it is always important to comply with time limits, there are benefits to getting your PCR completed as soon as possible – preferably right after the call is completed and before your shift ends. In a perfect world, every PCR would be completed before the next call, however we all know that is usually not the case.
Should PCR leave the reader asking questions?
Your PCR should never leave the reader asking questions, such as why an ambulance was called, what the initial patient’s condition was upon arrival or how the patient was moved from the position they were found in to your stretcher and ultimately to the ambulance.
Do ambulances have to be medically necessary to be reimbursed by Medicare?
Ambulance services, including the treatments and interventions provided to the patient – need to be medically necessary to be reimbursed by Medicare and other payers – and that is determined primarily by reviewing the PCR.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
What Is An Electronic Patient Care Report?
Medical devices are also known as “ePCRs,” because they contain medical information, assessments, treatment information, narrative, and signatures of patients. EMS units, ambulances, and fire departments created their own paper records of information before contacting ePCRs.
How Do You Write A Good Patient Care Report Part 2?
Talk about something only in limited details. When you are describing a patient who needs more intensive care, avoid using vague terms like “lowness,” “fall” or “transport”. You don’t always provide a clear image of the signs and symptoms at the point of care with these terms.
What Is Patient Care Report?
patient care report (PCR) serves not only as information gathering, but has also been designed to document everything that occurs within the facility during the facility’s care process. Documentation on a PCR can provide critical information that is needed during critical times in the hospitalization.
What Is The Current Standard For Electronic Patient Care Reporting In The Ems Industry?
The industry standard, called electronic patient care reporting or ePCR, is rapidly becoming as ubiquitous as paper forms of reporting. Electronic Prehospital Records Control improves the accuracy and legibility of documentation, as well as the ability of EMS providers to sort and summarize prehospital records with the help of such tools.
What Should Be Included In A Patient Report?
According to this recommendation, an information structure consisting of background stories, medical documentation, physical examination, pathology results and opinions should be adopted.
What Is A Writing Pcr?
Page 1. Students grades three-11 will use three prose constructed response (PCR) writing forms in grades 4 and 5 at the PARCC Summative Assessments. It is common to write in the classroom in informal and formal ways.
What is PCR in ambulance?
This includes a detailed assessment of the situation and a full recounting of the treatment administered to the patient. It is specific, informative, free of ambiguity and negligence. But yet, after all extensive training, the best some medics can do in the detailed assessment is to write "patient has pain to the arm."
What is an impression in medical terms?
An impression encompasses the reasons for patient treatment. Trauma and fall are too vague to be used as impressions. Include the body areas or symptoms that are being treated. In other words, what treatment protocol is being followed?
Wrapping Up
If you’ve been with us from the start we hope you’ve acquired some valuable skills for authoring an effective Patient Care Report.
Chronology
For most of us that use an ePCR program, recording the chronology of events for our incident happens in the section known as the flow chart.
Outside Assistance
We remind you to always include notations about any outside assistance that may have been provided during your incident.
Transport Incidents. Be Specific
Be careful when documenting the events that occur during transport to be specific in nature. Many times we read PCR’s that make general statements such as “…transported without incident.” While you may understand what this means to you, we caution about vague statements that can be interpreted by the reader to potentially mean something else.
Transfer of Care
There are times when you must transfer care to another individual. Of course, protocol will dictate that you turn over care to another healthcare provided who is equally or higher trained in most cases. Be sure to document who you turned over care to when doing so in the field and what their level of training was.
Times
We close out this discussion by reminding you to be sure to include the times of the incident in your PCR.
Conclusion
Well there you have it. Twelve weeks of a comprehensive discussion concerning writing effective Patient Care Reports. Now it’s up to you to use our recommendations to improve on your documentation skills. Have you arrived? We’re sure not. Even the most seasoned veteran provider can improve on documentation skills. It’s a work in progress.
What is a PCR report?
A patient care report, more commonly known as a PCR, is a summary of what went on during an emergency call. EMS and other first-responders use the PCR to fill in the details of every call -- even the ones that get canceled or deemed false alarms Every department has its own procedures for filing a PCR and many companies now use EPCRs, ...
How to end a PCR?
Finally, end the PCR by accounting for everything you did to help the patient. Record vital signs and whatever steps you took to neutralize bleeding, etc. Write down what medications you gave the patient as well as what other medical treatments you performed. The more details you can include the better. Include information about how the patient responded to any treatments you performed and then write about putting the patient in your rig and transporting her to the hospital. Conclude with the time you turned her over to the emergency room and what condition she was in at the time.
What is a MOI code?
Mechanism Mechanism of Injury (MOI): A two-letter code identifying how an injury was sustained. If the chief complaint is a trauma complaint, at least one mechanism of injury must be listed. Enter the codes of the primary MOI followed by the most significant
Why is documentation important in healthcare?
Documentation should reflect the standard of care in the community and justify the services rendered. The goal is to provide a form that facilitates patient assessment, encourages documentation of treatment, prompts reassessment after intervention, reduces liability, and ultimately improves patient care.
Is an IFT considered an inpatient?
IFTs can be categorized as either outpatient (typically a call originating from an emergency department), or inpatient (a call originating from a hospital ward or ICU). All inpatients will be classified as either medical or trauma. (See Complaints Section for documentation instructions on IFT patients).
What was the Medic 1 response to above location?
(Location): Medic 1 responded to above location on a report of a 62 y.o. male c/o of chest pain. Upon arrival, pt presented sitting in a chair attended by first responder. Pt appeared pale and having difficulty breathing.
Does the patient respond to questions?
Patient does not respond to questions, but crew is informed by family that patient is deaf. Per family, the patient has been "sick" today and after consulting with the patient's doctor, they wish the patient to be transported to HospitalA for treatment.
Be Specific
Paint A Picture of The Call
- The PCR must paint a picture of what happened during a call. The PCR serves: 1. As a medical record for the patient, 2. As a legal record for the events that took place on the call, and 3. To ensure quality patient care across the service. PCRs should go beyond merely stating that a patient was picked up at a certain location, transported to anothe...
Do Not Fall Into Checkbox Laziness
- EMS professionals have long been promised a PCR that basically writes itself. Electronic PCR softwareis a great tool and can improve the efficiency of PCR completion. However, simply clicking a box or making a selection from a drop-down menu cannot be a substitute for your words in the form of a clear, concise, accurate and descriptive clinical narrative. An EMS provide…
Complete The PCR as Soon as Possible After A Call
- Most states, and many EMS agencies themselves, often have time limits within which the PCR must be completed after the call ended – 24, 48 or 72 hours are common time limits. While it is always important to comply with time limits, there are benefits to getting your PCR completed as soon as possible – preferably right after the call is completed and before your shift ends. In a pe…
proofread, proofread, Proofread
- The easiest way to improve your PCR is to proofread before submitting it. We understand the dilemma, after writing the sixth PCR for the day, and having 10 minutes left in the shift, the last thing anyone wants to do is sit there and reread what they have just written. But that is exactly what needs to be done. Poor grammar and spelling is the easiest way to have your abilities calle…
Check Descriptions
Review Abbreviations
Check (and Recheck) Spelling and Grammar
Assess Your Chief Complaint Description
- An area of the PCR that is frequently misused is the chief complaint which should explain why you were called to the scene or why the patient is being treated. Chief complaint is not the cause of the injury. For example, a chief complaint is pain to the right lower arm, not the fact that the patient has fallen off a ladder. Using the patient’s own ...
Review Your Patient Impressions
Check The Final Details of The PCR
Popular Posts:
- 1. au health portal sign in
- 2. curry general hospital patient portal
- 3. northwest health - porter patient portal
- 4. la cardiology patient portal
- 5. firelands community hospital patient portal
- 6. primary care partners patient portal slo
- 7. community hospital patient portal
- 8. patient portal ut medical center
- 9. fwbmc.com/patient-portal
- 10. family healthcare oceana patient portal