How Nurses Should Document Pain - My Nursing Note
5 hours ago And again, we recommend this being filled out about 30 minutes to the end of your shift where there’s not a lot of options for changes to happen. So this first area here, what we fill out here is … >> Go To The Portal
How do you assess pain in a nursing home patient?
Use these subjective and objective data under the “nursing assessment” column of your care plan: Patient complains of pain. Appetite changes. Self-focused. Guarding behavior, protecting body part. Intolerant (e.g., altered time perception, withdrawal from social or physical contact) Facial mask of pain.
How do you write a nursing care plan for chronic pain?
Chronic Pain Nursing Care Plan 1 Causes 2 Signs and Symptoms 3 Goals and Outcomes. Patient reports pain at a level less than 3 to 4 on a 0 to 10 rating scale. ... 4 Nursing Assessment. A thorough assessment of chronic pain is necessary for the development of an effective pain management plan. 5 Nursing Interventions. ...
What questions should a nurse ask during a pain assessment?
Additionally, the nurse should ask the following questions during pain assessment to determine its history: (1) effectiveness of previous pain treatment or management; (2) what medications were taken and when; (3) other medications being taken; (4) allergies or known side effects to medications. 4. Determine the client’s perception of pain.
What does a nurse do when a patient is in pain?
A nurse might note the characteristics of the pain, a diagnosis of the pain itself or source of pain, and then set a plan for course of action.
How do you document patient pain?
Six Tips to Documenting Patient PainTip 1: Document the SEVERITY level of pain. ... Tip 2: Document what causes VARIABILITY of pain. ... Tip 3: Document the MOVEMENTS of the patient at pain onset. ... Tip 4: Document the LOCATION of pain. ... Tip 5: Document the TIME of pain onset. ... Tip 6: Document your EVALUATION of the pain site.More items...•
How do I document a pain assessment for nursing?
Nurses can help patients more accurately report their pain by using these very specific PQRST assessment questions:P = Provocation/Palliation. What were you doing when the pain started? ... Q = Quality/Quantity. What does it feel like? ... R = Region/Radiation. ... S = Severity Scale. ... T = Timing. ... Documentation.
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do you conduct a pain assessment?
Pain must be assessed using a multidimensional approach, with determination of the following:Onset: Mechanism of injury or etiology of pain, if identifiable.Location/Distribution.Duration.Course or Temporal Pattern.Character & Quality of the pain.Aggravating/Provoking factors.Alleviating factors.Associated symptoms.More items...•
How can you assess a patient's pain level?
Measuring pain Pain should be measured using an assessment tool that identifies the quantity and/or quality of one or more of the dimensions of the patients' experience of pain. This includes the: intensity of pain; intensity and associated anxiety and behaviour.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
How do you give a good report?
1:2020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd what I do with my report should sheet. At the end of the day I always tread it so tip alwaysMoreAnd what I do with my report should sheet. At the end of the day I always tread it so tip always shred your report sheet whenever you're done giving a report you don't want to stick it in your locker.
How do you organize a nursing report sheet?
0:1210:04Nurse Brain Sheet | ORGANIZE YOUR NURSING SHIFT | Nursing ReportYouTubeStart of suggested clipEnd of suggested clipOrganization tips for you to be successful during your nursing shift the main one being a reportMoreOrganization tips for you to be successful during your nursing shift the main one being a report sheet and this is what people call their nurse brains.
What is the format for report writing?
Report writing is a formal style of writing elaborately on a topic. The tone of a report and report writing format is always formal. The important section to focus on is the target audience. For example – report writing about a school event, report writing about a business case, etc.
What is a nurse report?
Nursing report is given at the end of the nurses shift to another nurse that will be taking over care for that particular patient. Nursing report is usually given in a location where other people can not hear due to patient privacy.
How do you do nursing documentation?
Nursing Documentation TipsBe Accurate. Write down information accurately in real-time. ... Avoid Late Entries. ... Prioritize Legibility. ... Use the Right Tools. ... Follow Policy on Abbreviations. ... Document Physician Consultations. ... Chart the Symptom and the Treatment. ... Avoid Opinions and Hearsay.More items...
What questions should a nurse ask during a pain assessment?
Additionally, the nurse should ask the following questions during pain assessment to determine its history: (1) effectiveness of previous pain treatment or management; (2) what medications were taken and when; (3) other medications being taken; (4) allergies or known side effects to medications. 4.
What is the duty of a nurse to ask about pain?
Acknowledge and accept the client’s pain. Nurses have the duty to ask their clients about their pain and believe their reports of pain. Challenging or undermining their pain reports results in an unhealthy therapeutic relationship that may hinder pain management and deteriorate rapport.
What is the nonpharmacologic treatment for pain?
Restriction of movement of a painful body part is another nonpharmacologic pain management. To do this, you need splints or supportive devices to hold joints in the position optimal for function. Note that prolonged immobilization can result in muscle atrophy, joint contracture, and cardiovascular problems.
What are the physiological signs of acute pain?
The physiological signs that occur with acute pain emerge from the body’s response to pain as a stressor. Other factors such as the patient’s cultural background, emotions, and psychological or spiritual discomfort may contribute to the suffering of acute pain.
How long does acute pain last?
The unexpected onset of acute pain reminds the patient to seek support, assistance, and relief. It has a duration of fewer than 6 months.
What are the other coanalgesics?
Other coanalgesics. Include anxiolytics, sedatives, antispasmodics to relieve other discomforts. Stimulants, laxatives, and antiemetics are other coanalgesics that reduce the side effects of analgesics.
What is the unpleasant feeling of pain?
The unpleasant feeling of pain is highly subjective in nature that may be experienced by the patient. The International Association for the Study of Pain (IASP) defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”.
What is pain in nursing?
Pain is a common symptom that children and older people experience. Nurses are in a position to assess pain in patients mostly children and older people exclusively owing to their relationship and interaction with the patients. Pain is multi-dimensional and subjective making its assessment challenging at times.
Why is pain assessment important?
Accurate pain assessment is vital for the development of effective pain management. Pain is a nervous system triggered feeling usually associated with the physical disorder such as illness or injuries. Pain is a common symptom that children and older people experience. Nurses are in a position to assess pain in patients mostly children ...
What is compressive pain assessment?
Wherefore, a compressive pain assessment must comprise the duration, location of pain, intensity, quality, elevating factors, timing, and the impact the pain is making on a day to day activity coordination the increment rate and Patients’ pains perception ...
What is biopsychosocial pain?
Biopsychosocial phenomenon usually impacts pain development, for example, social history issues, past pain experiences, cultural and religious beliefs, and first pain experience. For a pain assessment to be comprehensive, it is essential to note that the evaluation should happen when the patient is present. The nursing guideline precisely seeks ...
What is pain assessment?
Herein, pain assessment is the process of objectively understanding the state and condition of pain by observing the patient and measuring the intensity of the pain. The assessment is a broad concept that involves clinical judgment which is grounded in observation, uniqueness, and context of the individual experience with the pain.
What is the pain caused by neurological dysfunction?
Other Types of Pain. There is another type of pain that arises due to neurological dysfunction and not damage. This condition is known as Fibromyalgia. Fibromyalgia is a condition that is not clearly understood, but it commonly brings a multi-system failure which leads to widespread pain in the entire body.
What is the term for pain caused by the central nervous system?
2. Neuropathic pain. Neuropathic Pain arises when the reporting system (nervous system), central or peripheral is damaged either from diseases, injury, etc. Multiple sclerosis, chemotherapy, and phantom pain are some of the conditions that may damage neurons leading to neuropathic pain.
Why is it important to take pain seriously?
Each patient will experience pain differently , and it is imperative to take a patient’s pain seriously in order to provide high-quality care.
How often do nurses assess vision?
The nurse will assess the patient’s vision every 5 hours while patient is awake until vision is completely restored. The nurse will educate the patient on signs of a pending migraine. The nurse will educate the patient on the proper administration of Motrin.
Can nursing care plan change after surgery?
The strategy may change depending on the presenting symptoms or medical history of the patient: for example, a nursing care plan for pain after surgery will require a different approach than a patient in pain without an easily explained source.
Do nurses have to manage pain?
It’s up to nurses working in both inpatient and outpatient healthcare facilities to manage pain as it is experienced by their patients. But not all pain is created equally – pain levels can vary wildly, depending on their origin, and the pain tolerance of the patient in question.
Can chronic pain be a symptom?
Patients with chronic pain, owing to any number of conditions or disabilities, may experience acute pain which is either a symptom of their chronic illness, or an additional separate source. Similarly, acute pain may be experienced periodically over a great length of time, thus blurring the lines between the two categories.
How to manage pain?
Anticipate the need for pain management. Early and timely intervention is the key to effective pain management. It can even reduce the total amount of analgesia required. Provide a quiet environment. Additional stressors can intensify the patient’s perception and tolerance of pain. Use nonpharmacological pain relief methods (relaxation exercises, ...
What are the nonverbal indicators of pain?
It helps ensure that the patient receives effective pain relief. Observe for nonverbal indicators of pain: moaning, guarding, crying, facial grimace. Some patients may deny the existence of pain. These behaviors can help with proper evaluation of pain.
What is chronic pain?
Non-malignant chronic pain, on the other hand, refers to pain that persists beyond the expected time of healing.
How long does acute pain last?
It can happen after a medical procedure, surgery, trauma or acute illness. It has a duration of less than 6 months.
Why do people see doctors in 2020?
April 13, 2020. 151928. Pain is one of the most common reasons why patients see their doctors. And despite the advances in technology and methods to relieve it, a lot of patients still experience undertreatment. This makes it important for nurses to have the skills not just in assessing the pain but managing it as well.
Is pain subjective?
What your patient says about the pain he is experiencing is the best indicator of that pain. We can’t prove or disprove what the patient is feeling. We also can’t assume. Pain can be classified into two types.
Causes
The most common cause of acute pain is damage to the body tissues. This can be related to three different types of injury agents; physical, biological or chemical. Acute pain can also be related to psychological causes or exacerbations of existing medical conditions.
Signs and Symptoms
Some signs of pain are easy to recognize, such as verbal reports from the patient, expressions of pain such as crying, or significant changes in vital signs. Other manifestations of acute pain can be more difficult to spot.
Assessment
When assessing pain it is important to use the standard protocols for assessing and documenting pain and responses to intervention. It is also important to use the most appropriate pain scale available for each patient.
Nursing Care Plans for Acute Pain
The following are four example nursing care plans for caring for a patient in acute pain.
References and Sources
Shelly Caruso is a bachelor-prepared registered nurse in her fifth year of practice. She began her career as a nursing assistant and has worked in acute care for nearly eight years. In addition to her hospital and trauma center experience, Shelly has also worked in post-acute, long-term, and outpatient settings.
Definition of pain
A generally unpleasant emotional and sensory experience that occurs in response to actual or potential tissue trauma or inflammation Referred to as the fifth vital sign.
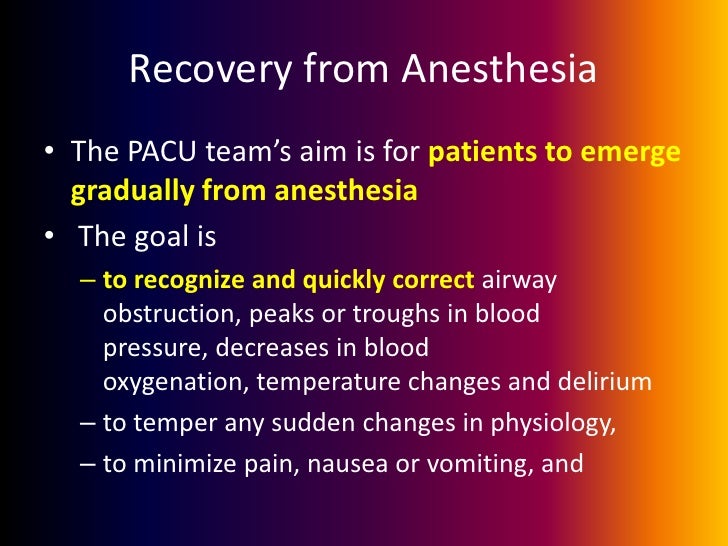
Acute pain
Mild to severe pain lasting less than 6 months; usually associated with a specific injury; associated with a sympathetic nervous system response; results in increased pulse rate and volume, increased respiratory rate and depth, increased blood pressure, and increased glucose levels; urine production and peristalsis decrease.
Chronic pain
Mild to severe pain lasting longer than 6 months; associated with the parasympathetic nervous system; the patient may not exhibit signs and symptoms associated with acute pain; may lead to depression and decreased functional status
Why do family members question the legitimacy of the patient's pain reports?
Family members, friends, co-workers, employers, and healthcare providers question the legitimacy of the patient’s pain reports because the patient may not look like someone in pain. The patient may also be involved of using pain to earn attention or to avoid work, commitments, and responsibilities. ADVERTISEMENTS.
What is the most reliable information about chronic pain?
Patient’s self-report is the most reliable information about the chronic pain experience. Assess and note for signs and symptoms related to chronic pain such as weakness, decreased appetite, weight loss, changes in body posture, sleep pattern disturbance, anxiety, irritability, agitation, or depression.
How long does chronic pain last?
Chronic pain is often described as any pain lasting more than 12 weeks. The pain may be classified as chronic malignant pain or chronic nonmalignant pain. Malignant pain is linked top a particular cause like cancer. In nonmalignant pain, the original tissue injury is not progressive or has been healed but the patient still experiences pain.
How to improve pain control?
One of the most important steps toward improved control of pain is a better patient understanding of the nature of pain, its treatment, and the role patient needs to play in pain control. Discuss patient’s fears of undertreated pain, addiction, and overdose.
What are the factors that cause chronic pain?
Here are some factors that may be related to chronic pain: Disease process (compression/destruction of nerve tissue/body organs, infiltration of nerves or their vascular supply, obstruction or a nerve pathway, inflammation) Injuring agents (biological, chemical, physical, psychological)
What factors influence pain?
Evaluate factors such as gender, cultural, societal, and religious features that may influence the patient’s pain experience and reaction to pain relief. Recognizing the variables that influence the patient’s pain experience can be instrumental in developing a plan of care that is acceptable to the patient.
Is nonmalignant pain progressive?
In nonmalignant pain, the original tissue injury is not progressive or has been healed but the patient still experiences pain. Chronic pain can be mild or excruciating, episodic or continuous, merely inconvenient or totally incapacitating.
Popular Posts:
- 1. my doctor's office patient portal mercy health physician partners
- 2. mount nittany patient portal
- 3. next generation healthcare patient portal
- 4. patient portal sw orlando family
- 5. brown clinic patient portal
- 6. columbuxs brown online patient portal
- 7. ohio covid vaccine patient portal
- 8. bethesda medical associates patient portal
- 9. patient portal phoenix children's
- 10. bozemandeaconess patient portal